Polyps in the maxillary sinus appear as a result of chronic inflammatory processes. When growing interfere with breathing, cause chronic runny nose and headaches. Without diagnosis, they are poorly differentiated from other otolaryngological diseases. As a rule, treatment in a clinic according to a unified protocol does not bring results.
Our Center has been specializing in providing care to patients with pathologies of the maxillary sinuses for more than 20 years. The ENT department is equipped with modern diagnostic and functional equipment. Surgical treatment is performed by maxillofacial surgeons with ENT training.
Causes
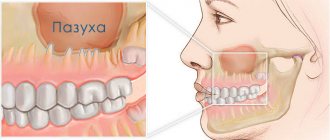
Polyps of the maxillary sinuses are the most frequently detected formations. These are benign neoplasms of the mucous membrane in the form of processes on thin stalks or a wide base. They grow from infected tissues against the background of inflammatory processes, and are combined with the sinus mucosa by connecting elements.
Polyps in the maxillary sinus (nasal polyps)
Main causes:
- frequent infectious diseases without treatment
- chronic inflammation of the maxillary sinus
- hereditary metabolic disorder, immune system malfunction
- sinus damage, presence of foreign bodies after dental treatment
- inflammation of the tooth root at the border with the sinus
- predisposition to allergies
Prevention
You can reduce your chances of polyps appearing or returning after treatment by following these strategies:
- Monitor allergy symptoms. Follow your doctor's recommendations to monitor the course of your allergic disease. If symptoms do not improve, consult your doctor about changing your treatment.
- Avoid irritants to the nasal mucosa. Avoid contact with substances that can cause inflammation or irritation of the mucous membranes (smoke, a suspension of small particles, caustic chemicals, allergens, dust, animal hair).
- Maintain good hygiene. Wash your hands thoroughly and regularly. This is one of the best ways to prevent infections that can cause inflammation of the mucous membranes of the nasal cavity and sinuses.
- Control the humidity in your home. When humidity levels are low, use humidifiers. This will moisturize the airways and improve self-cleaning of the sinuses and nasal cavity.
- Use nasal cleansers. Use a nasal douche (aerosol) with isotonic sodium chloride solution to clean the cavity. This will reduce the concentration of irritating agents on the nasal mucosa (allergens, dust, germs) and reduce inflammation. If you prepare your own saline solution, use distilled or boiled water.
Why are polyps of the maxillary sinuses dangerous?
The insidiousness of the disease is that small polyps do not cause any inconvenience. They grow slowly, without arousing suspicion for years. In our practice, there are situations when they are discovered by chance on a computer tomogram during preparation for treatment, extraction or implantation of teeth. And this is a great success for the patient; timely treatment can be undertaken at the initial stage without radical methods.
Otherwise, the polyps gradually grow, causing inconvenience to the point of blocking breathing . A worried patient runs from one ENT doctor to another. But the hope for a high-quality, timely examination in the clinic is weak; an appointment for a computed tomography scan of the sinuses can be waited for months. And standard drug treatment prescribed without the necessary diagnostics does not help. It is good when a doctor refers a patient to a specialized institution, even at the expense of his own reputation.
Initially, polyps are benign formations, but they are prone to degeneration into malignant ones . Sometimes there is a decrease in size, but these are rare cases. Therefore, when they are detected, you need to keep the situation under control. The best solution to the problem is removal of polyps to eliminate oncological problems.
Symptoms
- congestion in one or both nostrils
- feeling of constriction in the nose and throat
- lack of smell perception
- pain in the facial area
- often pain and pressure are projected onto the orbit, ear canal
- runny nose with copious mucus, frequent sneezing
If polyps of the maxillary sinuses are not removed in a timely manner, the neoplasms slowly grow, causing:
- hearing loss
- voice change
- conjunctivitis
- nosebleeds
- chronic headaches
- softening of surrounding bone tissue
- deformation of adjacent anatomical structures
- infection of the teeth at the border with the sinuses
Polyps are dangerous due to the possibility of tumors blocking the respiratory tract, even leading to death from suffocation
Why you should entrust treatment to the ENT department of dentistry
70% of patients who turned to us for help were previously treated in city clinics with many drug courses and traumatic operations in the form of sinus punctures. But, unfortunately, such methods are not able to get rid of polyps. A tumor in the paranasal sinuses can only be eliminated through surgery.
ENT dentistry is a comprehensive approach to the treatment of tumors in the maxillary sinuses. It combines two areas - otolaryngology and dentistry, allowing you to combine options for dental and ENT treatment .
Intervention in the maxillary sinuses requires highly qualified and trained physicians. Only a maxillofacial surgeon with ENT training can cope with such a task without complications . In addition, special high-tech equipment is required.
Contraindications: who should be careful when removing polyps?
- General health – depending on the general somatic condition of the patient and the presence of concomitant pathologies, polypectomy can be performed under either local or general anesthesia. It is necessary to adequately assess surgical anesthetic risks and conduct preoperative preparation.
- Tendency to bleed . Inherited bleeding tendencies such as hemophilia (an inherited bleeding disorder) require special precautions to prevent serious intra- or post-operative complications.
Diagnosis of polyps in the maxillary sinuses
During the examination, the main thing is to carry out a differentiated diagnosis to exclude other ENT diseases accompanied by similar symptoms
Upon visual examination, an increase in regional lymph nodes and swelling of the tissues in the area of the maxillary sinuses are observed.
X-ray examination in our Center is performed
on a computed tomograph in ENT mode .
Allows you to assess in detail the condition of the paranasal sinuses, determine the location and size of polyps. In difficult or controversial situations, the following may additionally be required:
- Videoendoscopy for examination of the nasopharynx and nasal cavity
- MRI to detect purulent fluid in the nasal appendages
- Bacteriological culture
Risk group
There is a certain risk group for developing nasal polyps. “These are people who work in unfavorable enterprises with a certain harmfulness. We are talking about dusty rooms, closed, with poor ventilation. And if a person breathes such air for years, then his risks increase,” says Vladimir Zaitsev. And, of course, those at risk are those who have a hereditary predisposition.
Soppy story. How to rinse your nose without mistakes Read more
Operation stages
Complex treatment is carried out in 1 day, we strive to combine all activities in one visit
- Preparation The operation is performed only after professional hygiene and sanitation of the oral cavity, and re-treatment of compromised dental roots. Sterility ensures there is no risk of infection.
- Removal Surgery according to the selected protocol for accessing the sinus with putting the patient to sleep with the simultaneous administration of an analgesic. Performed in a sterile operating room.
- Control X-ray examination CT after surgery is mandatory - to assess the quality of the operation performed and the condition of the maxillary sinus.
If a tooth with an inflamed root was removed, which provoked the growth of a polyp, after the operation the orthopedist will install a temporary orthopedic structure. You will never leave our Center without teeth.
On days 10-14, the sutures are removed and a control CT scan is performed. The patient is invited for a preventive examination and a convenient date for the visit is agreed upon.
How is recovery going?
Rest assured that we will not keep you at the Center unnecessarily
No hospitalization
Even in advanced cases with complex localization of polyps, the operation takes no more than 2-4 hours. Waking up after medicated sleep is not accompanied by deterioration of the condition and pain. The use of low-traumatic treatment protocols and the accumulated experience of doctors allow us to perform the operation as carefully as possible in relation to you. Hospitalization with an overnight stay at the clinic is not required .
For elderly patients with chronic cardiovascular diseases, a postoperative recovery service is provided in a day hospital for several hours under the supervision of an anesthesiologist. In any case, you will spend the night at home, in a familiar environment.
Inpatient recovery is necessary if general anesthesia was used, which often leads to complications, weakness and exacerbation of chronic pathologies. If a patient is offered a hospital stay for several days, this means that the clinic does not have modern equipment and qualified surgeons, or they are “squeezing” money out of you.
Branded rehabilitation on the day of treatment
The author's accelerated rehabilitation program ensures complete elimination of unpleasant consequences in the form of swelling, hematomas, muscle spasms, and pain.
Medicines to take home
After the operation, you will receive a free set of necessary medications to avoid purchasing counterfeit products. You don't have to run around pharmacies looking for the right medication in your postoperative condition.
The package with medications contains instructions with recommendations in the postoperative period. Please follow them to avoid complications.
Antrochoanal polyps (ACP) account for 4–6% of all nasal polyposis [1], and in children their frequency reaches 33% [2]. This is, as a rule, a unilateral process, although there are isolated observations of bilateral ACP [3, 4].
Typical clinical symptoms of ACP are difficulty in nasal breathing, rhinorrhea and postnasal drip [2, 5]. Other symptoms include headache, hyposmia, snoring, obstructive sleep apnea syndrome, halitosis, and nosebleeds [2]. However, with gigantic sizes of ACP reaching the lower parts of the pharynx, dyspnea, dysphagia, and, in rare cases, cachexia are associated [6-12].
We provide a description of two clinical cases of ACP. In the first case, the gigantic size of ACP caused the appearance of unusual clinical symptoms of the disease. In the second observation, we were able to track the rate of transformation of the antral polyp into ACP.
Clinical observation 1
Patient K.
, 17 years old, was admitted to the ENT clinic in January 2016 with complaints of lack of nasal breathing, rhinorrhea, hyposmia, shortness of breath during exercise and a feeling of suffocation when lying on her back, as a result of which the patient had been sleeping on her stomach in recent months. The patient believes that difficulty in nasal breathing appeared 4 months before visiting the ENT clinic; its occurrence is associated with an acute respiratory viral infection.
On examination: the right half of the nose is filled with thick viscous mucus, a small amount of mucus is noted in the left half. The nasal septum is deviated to the right. Pharyngoscopy reveals a polyp-like formation hanging from the nasopharynx, pushing the soft palate anteriorly and covering the entire posterior wall of the pharynx. When pressing on the root of the tongue, it was not possible to see the edge of this formation, although it turned out to be mobile. An endoscopic examination of the nasal cavity after evacuation of mucus with an electric suction revealed an ACP pedicle in the right half, emanating from the maxillary sinus; the posterior sections of the nasal cavity are completely occupied by a polyp, which partially obstructs the lumen of the choana on the opposite side.
The patient underwent spiral computed tomography (SCT) of the paranasal sinuses, which revealed an ACP emanating from the right maxillary sinus, descending into the hypopharynx almost to the level of the upper edge of the epiglottis (Fig. 1, a-c).
Rice. 1. CT tomogram of the paranasal sinuses of patient K. a, b - axial projection: the ACP is determined, emanating from the right maxillary sinus and occupying the entire nasopharynx; c — coronal projection: the polyp descends into the hypopharynx to the level of the edge of the epiglottis; d - removed polyp.
Removal of the ACP was performed under endoscopic control under local anesthesia, since intubation was impossible due to the distal part of the polyp, which occupied almost the entire hypopharynx. First, the polyp was grabbed with a clamp through the mouth, then its pedicle was crossed at the exit level through the accessory anastomosis in the posterior fontanella, after which the polyp was removed through the mouth (see Fig.
rice. 1, d). During the revision of the sinus, the remaining part of the polyp was removed through the enlarged anastomosis.
This observation is of interest due to the gigantic size of the polyp, which caused bilateral nasal obstruction and breathing difficulties in the supine position.
In the literature, there are only a few descriptions of cases of dyspnea caused by ACP [7, 9]. The patient had no difficulty swallowing food, although the polyp had a large anteroposterior size and descended into the laryngopharynx. It is noteworthy that the patient gives a clearly underestimated duration of the disease - 4 months. Probably, during this period she began to have difficulty breathing through the opposite half of her nose, which was the reason for going to the doctor.
Clinical observation 2
Patient F.
, 17 years old, was admitted to the ENT clinic in January 2016 due to lack of breathing through the left half of the nose, rhinorrhea, and postnasal drip. Considers himself sick for 6 months. In September 2015, he addressed similar complaints to an otolaryngologist, but upon examination, no pathological changes were revealed in the nasal cavity; SCT dated September 09, 2015 revealed a cyst of the left maxillary sinus (Fig. 2, a, b).
Rice.
2. CT scan of patient F. a, b — CT scan dated 09.09.2015: a cyst of the left maxillary sinus is detected, the nasal cavity is free; c, d — SCT dated January 12, 2016: there is a cyst and ACP. In January 2016, during anterior rhinoscopy and endoscopic examination, the patient was found to have ACP on the left. SCT of the paranasal sinuses dated January 12, 2016 revealed ACP originating from the left maxillary sinus (see.
rice. 2, c, d). The polyp was removed endoscopically.
This case is interesting because we were able to document the period during which the polyp spread from the maxillary sinus into the nasal cavity, and then into the choana. This took 4 months.
The etiology of ACP is unknown. The role of chronic inflammation and allergies in the formation of ACP is discussed in the literature, but none of the theories has been confirmed to date [2, 13].
Morphological studies of ACP and multiple nasal polyps reveal some differences in their microscopic and ultrastructural structure [14], as well as in the processes of angiogenesis [15], which indicates differences in the mechanisms of formation of these pathological formations.
Many authors [1, 16] believe that the formation of ACP is associated with a pre-existing cyst in the maxillary sinus, which can be asymptomatic for a long time [17], but then its membrane gives rise to the growth of a polyp, which penetrates into the nasal cavity through a natural or additional anastomosis with subsequent spread towards the choana. P. Frosini et al. [1] explain the formation of ACP by an increase in pressure in the maxillary sinus, which develops as a result of the pathology of the ostiomeatal complex. The assumption about the role of anatomical and physiological characteristics and impaired sinus ventilation in the pathogenesis of ACP is confirmed by the study of S. Aydin et al. [18], who demonstrated a statistically significant increase in the volume of both maxillary sinuses in patients with ACP compared to healthy people. In addition, there is evidence of a frequent combination of ACP and pathology of the lateral wall of the nasal cavity. Thus, A. Zakrzewska et al. [19] studied the anatomical features of two groups of children (15 people each): with chronic rhinosinusitis (group 1) and ACP (group 2). In the group of children with ACP, 7 people had an additional anastomosis of the maxillary sinus and 4 had a significant increase in the size of the natural anastomosis, while in patients with chronic rhinosinusitis, such a pathology was not detected in any case.
The role of increasing the size of the maxillary sinus outlet and the formation of additional anastomoses with the nasal cavity in the formation of ACP is emphasized by G.Z. Piskunov and S.Z. Piskunov [20]. The authors believe that in conditions of impaired aerodynamics of the nasal cavity and increased aeration of the maxillary sinus, mucoid degeneration of the own layer of the mucous membrane develops with the formation of false cysts, from which the formation of a polyp stalk begins. The authors consider the absence of internal diapedesis of neutrophilic granulocytes to be an important feature of pseudocysts, which explains the rarity of purulent inflammation in ACP. The authors explain the growth of the polyp towards the anastomosis by the suction effect during breathing.
Contrary to the popular belief about the typical structure of the ACP with the presence of a cystic part in the maxillary sinus, in recent years there have been reports of the absence of cystic changes in the part of the ACP that forms its pedicle [21, 22]. A. El-Sharkawy [21] found a cystic part of the ACP in 3 of 36 operated children; in the remaining 33 patients, the intra-sinus part was polyposis.
H. Mostafa et al. [22], having analyzed 25 cases of endoscopic removal of ACP, noted that the intramaxillary part of the polyp was cystic in only 2 (8%) patients, and in 23 (92%) patients it was a polyp stalk, not different in structure from the rest of the formation. The authors studied the structure of the transition zone between the stalk of the polyp and the normal mucous membrane of the sinus in order to identify disorders in the lymphatic system of this area. The density of lymphatic vessels was assessed by identifying endothelial receptors for hyaluronic acid (LYVE-I). As a result of the study, it was found that in the transition zone their density is significantly higher than in the surrounding mucous membrane, this indicates the presence of lymphatic obstruction (primary or secondary, as a result of inflammation). According to the authors, the detected lymphatic obstruction may play a decisive role in the processes of occurrence and growth of ACP.
The role of inflammatory triggers in the occurrence of ACP continues to attract the attention of researchers. In recent years, data have been obtained to exclude the possible participation of staphylococcal superantigen in the pathogenesis of ACP [23, 24]. There are studies on the role of matrix proteinases in the pathogenesis of ACP [25], but this area requires further study.
Human papillomavirus infection (PVI) is discussed as one of the possible causes of ACP. Thus, M. Knör et al. [26] in a study of 257 fragments of the nasal mucosa found DNA sequences of the human papillomavirus (HPV) in choanal polyps in 55.8% of cases, in the tissues of ordinary polyps in 15.1% and in the mucous membrane of the nasal turbinates in 5 .8%, which, according to the authors, indicates the presence of latent PVI. Similar data on the presence of HPV were obtained when examining tissue from inverted nasal papilloma [27]. Taking into account the peculiarities of the interaction of HPV with tissues, in particular its ability to disrupt programmed cell death, studying the role of PVI in the development of hyperplastic processes seems to be a promising direction.
Treatment for ACP is always surgical. The previously used traditional polypotomy and Caldwell-Luc surgery have now given way to endoscopic techniques. Simple polypotomy gives a high percentage of relapses, especially in children and young people. The Caldwell-Luc procedure provides a good overview of the sinus, but is fraught with the danger of complications in the form of prolonged anesthesia and swelling of the cheek, damage to the infraorbital nerve, tooth buds and growth centers of the upper jaw in children, which subsequently leads to the development of sinus hypoplasia [28].
It should be emphasized that incomplete removal of the antral part of the polyp is associated with the risk of its recurrence. The relapse rate of ACP ranges from 5.3 [29] to 11.1% [21], the relapse period is 1.2±0.6 years [30], and relapses are observed more often in children [5]. S. Chaiyasate et al. [30] recommend monitoring patients after removal of ACP for 2 years, since during this period it is possible to detect 95% of relapses.
Most authors [1, 29—32] are proponents of the use of functional endoscopic sinus surgery (FESS) to remove ACP. N. Choudhury et al. [33] reported no relapses of ACP in 29 patients operated on endoscopically with an average follow-up of 22.5 months.
In cases where it is not possible to ensure complete removal of the polyp stalk endoscopically, it is advisable to use a combined method using FESS and micromaxillary sinusotomy [1, 13, 29, 31]. To ensure complete removal of ACP, it is proposed to use all possible means to improve visibility and (subsequently) ventilation of the sinus: partial removal of the uncinate process, sufficient expansion of the anastomosis, if necessary, partial endoscopic septoplasty, intervention on the nasal turbinates, adenotomy, as well as endoscopes with different viewing angles and shavers [34, 35].
Thus, the problem of ACP requires study to identify etiopathogenetically significant factors, which will ensure further progress in the treatment and prevention of this disease.
There is no conflict of interest.