Compound
The solution for intravenous administration includes the active component lidocaine hydrochloride (monohydrate form).
An additional component is water for injection. The active component included in the injection solution is also lidocaine hydrochloride (monohydrate form), additional components are sodium chloride, water.
Spray 10% for topical use contains lidocaine , as well as additional components: propylene glycol, peppermint oil, 96% ethanol.
Eye drops contain lidocaine hydrochloride , as well as benzethonium chloride, sodium chloride, and water.
The gel for external use also contains a similar active substance.
Lidocaine gel –
There are both professional lidocaine-based gels for dental clinics and those that can be bought at any pharmacy. An example of a common gel with lidocaine is the drug “Kamistad”. This gel contains lidocaine and chamomile extract as active ingredients. Created specifically for application to the oral mucosa. It has an analgesic and slight anti-inflammatory effect.
Lidocaine gel: price The cost of the drug Kamistad is about 230 rubles. If we talk about analogues for anesthesia of the mucous membrane, then the Cholisal gel has a slightly less pronounced, but longer-lasting analgesic effect. The latter also has a pronounced anti-inflammatory effect. The cost of the last drug is about 300 rubles.
Lidocaine release form
The product is available in different forms:
- The solution, which is administered intravenously, is colorless and odorless. The solution is poured into ampoules of 2 ml, 5 pcs. in blister strip packaging. Two such packages are placed in a cardboard pack.
- The solution intended for injection is odorless and colorless, it is bottled in ampoules of 2 ml, in blister packs - 5 such ampoules. A solution of 10%, 2%, 1% is available.
- Spray with lidocaine 10 percent is a colorless alcohol solution that has a menthol aroma. Contained in bottles (650 doses), it is equipped with a special pump and spray nozzle. The bottle is placed in a cardboard box.
- Eye drops 2% are colorless and odorless, but sometimes they may be slightly colored. Contained in 5 ml polyethylene bottles.
- A gel is also available.
Publications in the media
(Lidocainum) INN
Synonyms. Xycaine, Xylocaine.
Composition and release form. 1% solution of lidocaine hydrochloride in ampoules of 10 ml; 2% solution in ampoules of 2 and 10 ml; 10% solution in ampoules of 2 ml; an aerosol can containing 790 doses of lidocaine hydrochloride, 4.8 mg each.
Indications. Infiltration, conduction, epidural, spinal anesthesia; local anesthesia in dentistry, otorhinolaryngology, surgery (tracheal intubation, bronchoesophagoscopy, removal of polyps, etc.); arrhythmia, prevention of ventricular fibrillation.
Pharmachologic effect. Lidocaine has a strong local anesthetic effect and antiarrhythmic activity. Lidocaine is used in different concentrations: for infiltration anesthesia - 0.025-0.5% solution; conductor - 1-2% solution, terminal - 10% solution. Compared to novocaine, it acts faster, stronger and longer. In low concentrations (0.5%) it does not differ significantly in toxicity from novocaine; with increasing concentration to 1-2%, toxicity increases by 40-50%. The drug blocks the occurrence and conduction of nerve impulses, reducing the permeability of neuronal membranes to sodium ions, which leads to stabilization of the membrane and inhibits depolarization. The antiarrhythmic effect of the drug is due to its stabilizing effect on the cell membranes of the myocardium. It blocks the slow flow of sodium ions into myocardial cells and is therefore capable of suppressing the automaticity of ectopic foci of impulse formation. In this case, the conductivity function is not inhibited. The drug promotes the release of potassium ions from myocardial cells and accelerates the process of repolarization of cell membranes, shortens the duration of the action potential and the effective refractory period.
Pharmacokinetics. The rate of absorption is affected by the site of administration and the rate of administration of the drug. With resorptive action from the surface of the mucous membranes, the maximum concentration of lidocaine in the blood is achieved after 10-30 minutes; with intravenous administration of the drug - after 5 minutes. 50% protein bound. Metabolized in the liver to form two pharmacologically active metabolites. T 1/2 is from 1 to 3 hours. A small part of the drug undergoes enterohepatic circulation and is excreted in the feces; 10% is excreted unchanged in urine.
Side effects. Headache, dizziness, drowsiness, anxiety, euphoria, ringing in the ears; bradycardia, conduction disturbances; decrease in blood pressure; collapse.
Contraindications. Increased individual sensitivity to lidocaine, weakness of the sinus node in elderly patients, AV block of II-III degree, severe bradycardia, cardiogenic shock; severe liver dysfunction.
Adverse reactions when interacting with other drugs. When beta-blockers are used together with lidocaine, the metabolism of lidocaine slows down due to a decrease in blood flow to the liver, which leads to an increased risk of lidocaine toxicity. Antagonism was noted in the effects of antimyasthenic drugs and lidocaine due to inhibition of neuronal transmission under the influence of the latter.
Information for the patient. When using an aerosol form of lidocaine, it should be remembered that the amount of the sprayed drug depends on the surface to be anesthetized. In adults, the dose should not exceed 200 mg. The aerosol should not come into contact with the eyes. Various types of local anesthesia are administered by medical staff.
pharmachologic effect
Lidocaine - what is it?
Wikipedia indicates that lidocaine is a derivative of acetanilide in chemical structure. It has a pronounced antiarrhythmic and local anesthetic effect.
The pharmacological group to which the active substance belongs is local anesthetics .
Inhibits nerve conduction by blocking sodium channels in nerve fibers and nerve endings, thereby providing a local anesthetic effect.
If we compare the anesthetic effect of procaine , then lidocaine is 2-6 times superior to it. Also, its effects develop faster and last longer. How long the drug lasts depends on the interaction with other drugs. If the drug is used simultaneously with Epinephrine , then the effect lasts more than 2 hours. When applied topically, vasodilation is observed, but no local irritating effect is noted.
In the body, it stabilizes the cell membrane, blocks sodium channels, increases the level of membrane permeability for potassium ions, which determines its antiarrhythmic effect .
Under its influence, repolarization in the ventricles is accelerated, the fourth phase of depolarization in Purkinje fibers is inhibited, without affecting the electrophysiological state of the atria.
It does not have a significant effect on myocardial contractility and conductivity. The negative inotropic effect is slightly pronounced, it manifests itself for a short time and only if the drug is administered in large doses.
Pharmacokinetics and pharmacodynamics
The highest concentration in the blood after intravenous administration is observed after 5-15 minutes, if the infusion is carried out slowly without a saturating initial dose, the maximum concentration is observed after 5-6 hours, and in people with acute myocardial infarction it can be achieved after a long time - up to 10 hours. Binds to plasma proteins by 50-80%. It is quickly distributed in the body and penetrates the placental and blood-brain barriers.
Metabolism mainly occurs in the liver; microsomal enzymes , resulting in the formation of active metabolites - glycine xylidide and monoethylglycine xylidide . People with liver disease have a slower metabolism. Excretion occurs in bile and urine.
If lidocaine cream or other agents are applied topically, absorption depends on the dose and also on the site where the lidocaine cream or gel is applied. Absorption is affected by the rate of perfusion in the mucosa.
There is good absorption in the respiratory tract, so care must be taken to prevent the administration of the drug in toxic doses.
After injections of lidocaine intramuscularly, almost complete absorption is noted. It is distributed quickly and binds to proteins, depending on the concentration of the active ingredient, by 60-80%.
The half-life depends on the dose administered, it is 1-2 hours.
If an aerosol is used, its effect appears within 1 minute and lasts 1-2 minutes. There is a gradual disappearance of the achieved decrease in sensitivity over 15 minutes.
Indications for use
A number of indications for the use of different forms of the drug are determined.
Indications for use intravenously and intramuscularly:
- for carrying out infiltration, spinal, epidural, conduction anesthesia ;
- for terminal anesthesia (also used in ophthalmology);
- for ventricular arrhythmias that are associated with glycoside intoxication;
- for the relief and prevention of the development of repeated ventricular fibrillation in patients with acute coronary syndrome, as well as repeated paroxysms of ventricular tachycardia .
In dentistry, Lidocaine in ampoules is used for local anesthesia during surgical interventions in the oral cavity:
- when removing baby teeth;
- when opening superficial abscesses ;
- when removing bone fragments and suturing wounds;
- for anesthesia of the gums for the purpose of fixing a prosthesis or crown;
- in order to suppress or reduce the enhanced pharyngeal reflex during preparation for an x-ray examination;
- before removal or excision of an enlarged papilla of the tongue;
- before excision of benign superficial mucosal tumors;
- for opening salivary gland cysts and frenulectomy in children.
Application in ENT practice:
- before septectomy , electrocoagulation , resection of nasal polyps;
- for additional pain relief before opening a peritonsillar abscess ;
- as additional anesthesia before puncture of the maxillary sinus ;
- before tonsillectomy for the purpose of pain relief and reduction of the pharyngeal reflex (not used for adenectomy and tonsillectomy in children under eight years of age);
- for pain relief before washing the sinuses.
Use for examinations and endoscopy:
- for anesthesia, if necessary, insert a probe through the mouth or nose;
- for anesthesia before performing rectoscopy and if necessary, replacing catheters.
Application in obstetrics and gynecology:
- for the purpose of anesthetizing the perineum for episiotomy or treatment;
- for anesthesia of the surgical field during a number of surgical interventions;
- for anesthesia when suturing in case of abscesses ;
- for pain relief during excision and treatment of hymen rupture.
Application in dermatology:
- for anesthesia of mucous membranes before minor surgical operations.
Application in ophthalmology:
- for anesthesia, if necessary, use contact research methods;
- for pain relief during short-term interventions on the conjunctiva and cornea;
- during preparation for ophthalmological operations.
Lidocaine 10% 50ml 38g spray for topical use dosed
pharmachologic effect
Local anesthetic for superficial anesthesia.
The action is due to the blockade of voltage-dependent sodium channels, which prevents the generation of impulses at the endings of sensory nerves and the conduction of pain impulses along nerve fibers. When applied topically, it dilates blood vessels and does not have a local irritating effect. Has an analgesic effect.
The effect develops 1-5 minutes after application to mucous membranes or skin and lasts 30-60 minutes.
Composition and release form Lidocaine 10% 50ml 38g spray for topical use, dosed
Spray - 1 dose/1 bottle:
- Active substance: lidocaine 4.6 mg 3.8 g.
- Excipients: peppermint leaf oil, propylene glycol, ethanol 96%.
38 g (650 doses) - dark glass bottles with a capacity of 50 ml (1) with a dosing pump with a spray head - cardboard packs.
Description of the dosage form
Spray for topical use dosed in the form of an almost colorless alcohol solution with a characteristic menthol odor.
Characteristic
Acetanilide derivative.
Directions for use and doses
The drug is used locally, externally. The dose depends on the indications and the area of the anesthetized surface.
1 dose of spray, released by pressing the dosing valve, contains 4.8 mg of lidocaine.
To avoid high concentrations of lidocaine in blood plasma, the lowest dose that provides a satisfactory effect should be used. Usually 1-2 sprays are sufficient, although 15-20 sprays or more are used in obstetrics (maximum dose - 40 sprays/70 kg body weight).
Recommended doses for various indications:
| Application area | Dose (number of sprays) |
| Dentistry | 1-3 |
| Oral surgery | 1-4 |
| Otorhinolaryngology | 1-4 |
| Endoscopy | 2-3 |
| Obstetrics | 15-20 |
| Gynecology | 4-5 |
| Dermatology | 1-3 |
The drug can also be applied using a cotton swab soaked in it.
When performing dental procedures and surgeries in children, it is preferable to apply Lidocaine spray using a cotton swab, which avoids the fear of spraying the drug, as well as the tingling sensation (a common side effect).
Pharmacokinetics
Suction
Rapidly absorbed from mucous membranes (especially the pharynx and respiratory tract). The degree of absorption of the drug is determined by the degree of blood supply to the mucous membrane, the total dose of the drug, the localization of the site and the duration of application. After application to the mucous membrane of the upper respiratory tract, it is partially swallowed and inactivated in the gastrointestinal tract. The time to reach Cmax when applied to the mucous membrane of the oral cavity and upper respiratory tract is 10-20 minutes.
Distribution
Protein binding depends on the concentration of the drug and is 60-80% at a drug concentration of 1-4 μg/ml (4.3-17.2 μmol/l). It is distributed quickly (T1/2 phases of distribution - 6-9 minutes), first enters well-supplied tissues (heart, lungs, brain, liver, spleen), then into adipose and muscle tissue. Penetrates the BBB and placental barrier, secreted into breast milk (40% of the concentration in maternal plasma).
Metabolism and excretion
Metabolized in the liver (90-95%) with the participation of microsomal enzymes by dealkylation of the amino group and cleavage of the amide bond with the formation of metabolites that are less active compared to lidocaine (monoethylglycine xylidine and glycine xylidine), T1/2 of which is 2 hours and 10 hours, respectively.
Excreted with bile and kidneys (up to 10% unchanged).
Pharmacokinetics in special groups of patients
In liver diseases, the metabolic rate decreases and ranges from 50% to 10% of the normal value.
In chronic renal failure, accumulation of metabolites is possible.
Indications for use Lidocaine 10% 50ml 38g spray for topical use, dosed
For terminal (superficial) anesthesia of mucous membranes.
In dentistry:
- anesthesia of the injection area before local anesthesia;
- suturing the mucous membrane;
- removal of mobile baby teeth;
- removal of tartar;
- anesthesia of the gums before fixing a crown or bridge;
- in children during surgery for excision of the frenulum of the tongue and opening of salivary gland cysts.
In otorhinolaryngology:
- operations on the nasal septum;
- carrying out electrocoagulation.
In obstetrics and gynecology:
- episiotomy and incision debridement;
- removal of seams;
- interventions on the vagina and cervix.
For instrumental and endoscopic studies:
- insertion of a probe, rectoscopy, intubation, etc.;
- X-ray examination (to eliminate nausea and pharyngeal reflex).
In surgery and dermatology:
- as an analgesic drug for burns (including sunburn), small wounds (including scratches);
- superficial anesthesia of the skin during minor surgical interventions.
Contraindications
- Use for tonsillectomy and adenotomy in children under 8 years of age;
- hypersensitivity to lidocaine and other components of the drug.
The drug should be used with caution during instrumental studies (rectoscopy) in patients with hemorrhoidal bleeding, local infection in the area of application, trauma to the mucous membrane or skin in the area of application, severe somatic pathology, epilepsy, bradycardia, impaired cardiac conduction, impaired liver function, severe shock, in young children, elderly patients, during pregnancy and lactation.
Application Lidocaine 10% 50ml 38g spray for topical use dosed during pregnancy and breastfeeding
There are no results from controlled clinical studies in pregnant women. If local anesthesia is necessary and there is no safer treatment, lidocaine spray can be used during pregnancy.
Lidocaine is excreted in breast milk, but after topical use in normal therapeutic doses, the amount excreted in milk is too small to cause any harm to a nursing infant.
Use in children
In children under 2 years of age, it is preferable to use the drug by applying it with a swab, which avoids the fear that appears when spraying, as well as the burning sensation.
It should be borne in mind that in children the swallowing reflex occurs much more often than in adults.
Lidocaine in aerosol form is not recommended for local anesthesia before tonsillectomy and adenotomy in children under 8 years of age.
special instructions
It is important to prevent lidocaine from entering the respiratory tract (risk of aspiration). Application to the throat requires special attention.
Application to the buccal mucosa is associated with a risk of dysphagia and subsequent aspiration, especially in children. If the sensitivity of the tongue and mucous membrane of the cheeks is impaired, the risk of biting them increases.
Lidocaine is well absorbed through mucous membranes (especially in the trachea) and damaged skin. This should be taken into account, especially when treating large areas of tissue in children.
In cases of using the spray during surgical operations in the pharynx or nasopharynx, it should be taken into account that lidocaine, suppressing the pharyngeal reflex, enters the larynx and trachea and suppresses the cough reflex, which can lead to bronchopneumonia. This is especially important in children, as they are more likely to trigger their swallowing reflex. In this regard, the spray is not recommended for local anesthesia before tonsillectomy and adenotomy in children under 8 years of age.
Caution should be exercised when applying lidocaine to damaged mucous membranes and/or infected areas.
The drug should be used with caution in patients with epilepsy, as well as bradycardia, cardiac conduction disorders, liver dysfunction and severe shock, especially when significant amounts of the drug can be expected to be absorbed when large areas of tissue are treated with high doses.
The drug in lower doses should be used in weakened and elderly patients, in acute diseases, as well as in children - in accordance with age and general condition.
In children under 2 years of age, it is recommended to apply Lidocaine spray with a cotton swab dipped in the drug.
During application of the drug, the bottle should be kept as vertical as possible. The spray should not get into your eyes. Do not open the bottle or heat it.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Overdose
Symptoms: increased sweating, pale skin, dizziness, headache, blurred vision, ringing in the ears, diplopia, decreased blood pressure, bradycardia, arrhythmia, drowsiness, chills, numbness, tremor, anxiety, agitation, convulsions, methemoglobinemia, cardiac arrest.
Treatment: when the first signs of intoxication appear (dizziness, nausea, vomiting, euphoria), further administration is stopped and the patient is transferred to a horizontal position; oxygen inhalation is prescribed; for convulsions - 10 mg diazepam intravenously; for bradycardia - m-anticholinergic blockers (atropine), vasoconstrictors (norepinephrine, phenylephrine). Dialysis is ineffective.
Side effects Lidocaine 10% 50ml 38g spray for topical use dosed
Local reactions: a slight tingling sensation that disappears as the anesthetic effect develops (within 1 minute); Transient erythema, swelling and sensory disturbances may occur.
Allergic reactions: very rarely - urticaria, angioedema, bronchospasm; in exceptional cases - anaphylactic shock. The use of the drug should be stopped immediately if any allergic reaction occurs.
The frequency of systemic effects after topical use of the drug is extremely low, because Only a very small amount of the active substance can enter the bloodstream.
From the side of the central nervous system: very rarely - nervous excitement, systemic dizziness, insomnia, loss of consciousness and respiratory paralysis.
From the cardiovascular system: decreased blood pressure, depression of myocardial function, bradycardia, cardiac arrest.
Drug interactions
Cimetidine and propranolol reduce the hepatic clearance of lidocaine (decreased metabolism due to inhibition of microsomal oxidation and decreased hepatic blood flow) and increase the risk of toxic effects (including stunned state, drowsiness, bradycardia, paresthesia, etc.).
Barbiturates, phenytoin, rifampicin (inducers of microsomal liver enzymes) reduce effectiveness (an increase in dose may be required).
When prescribed with ajmaline, phenytoin, verapamil, quinidine, amiodarone, the negative inotropic effect may be enhanced. Co-administration with beta-blockers increases the risk of bradycardia.
Curare-like drugs enhance muscle relaxation.
Procainamide increases the risk of developing central nervous system excitation and hallucinations.
With the simultaneous administration of lidocaine and hypnotics and sedatives, their inhibitory effect on the central nervous system may be enhanced.
With intravenous administration of hexobarbital or sodium thiopental against the background of the action of lidocaine, respiratory depression is possible.
Under the influence of MAO inhibitors, the local anesthetic effect of lidocaine may be enhanced.
With the simultaneous use of lidocaine and polymyxin B, an increased inhibitory effect on neuromuscular transmission is possible, so in this case it is necessary to monitor the patient's respiratory function.
Contraindications for use
Lidocaine in ampoules should not be used by people who have the following diseases and conditions:
- severe bradycardia ;
- sick sinus syndrome;
- sinoatrial block;
- AV blockade of the second and third degree (exception - when a probe is inserted to stimulate the ventricles);
- heart failure in acute and chronic form;
- WPW syndrome;
- significant reduction in blood pressure ;
- cardiogenic shock;
- Adams-Stokes syndrome;
- retrobulbar administration (for people suffering from glaucoma );
- intraventricular conduction disorders;
- pregnancy and lactation;
- severe sensitivity to the components of the product.
Caution Lidocaine IV and for injection is prescribed for chronic heart failure , hypovolemia , arterial hypotension , sinus bradycardia , severe renal and liver failure, first-degree AV block, reduced hepatic blood flow, epileptiform convulsions .
The drug is also prescribed with caution to elderly and weakened people, adolescents and children under 18 years of age, and patients with high sensitivity to other amide drugs for local anesthesia.
It is also important to consider that the patient may have contraindications to a certain type of anesthesia.
It should be noted that the aerosol is contraindicated for use in plaster dentistry as an impression material, as there is a risk of aspiration .
Side effects
When used, the following side effects may develop:
- Central nervous system: headache, euphoria , drowsiness , dizziness , disturbances of consciousness, weakness, convulsions, disorientation , paresthesia , nystagmus , tremor , neurotic reactions, photophobia , tinnitus, etc.
- Blood vessels and heart: decreased pressure, chest pain, collapse, bradycardia (possible cardiac arrest), peripheral vasodilation.
- Allergy symptoms: rash , itching , urticaria , angioedema , anaphylactic manifestations.
- Gastrointestinal tract: vomiting , nausea .
- Other manifestations: feeling of cold or heat, persistent anesthesia , hypothermia , methemoglobinemia , erectile dysfunction .
- Local manifestations: a slight burning sensation that disappears within 1 minute.
Instructions for use of Lidocaine (Method and dosage)
Lidocaine injections, instructions for use
Lidocaine hydrochloride can be used for infiltration anesthesia intramuscularly, intradermally, subcutaneously. A lidocaine solution of 5 mg/ml is used (the maximum allowable dose is 400 mg).
For the purpose of blocking the nerve plexuses and peripheral nerves, it is administered perineurally, 10-20 ml of solution is used. 10 mg/ml or 5-10 ml solution. 20 mg/ml.
- Conduction anesthesia involves the use of 10 mg/ml and 20 mg/ml perineurally.
- Epidural anesthesia involves the use of epidural 10 mg/ml or 20 mg/ml.
- Spinal anesthesia involves the use of subarachnoid 3-4 ml of a solution. 20 mg/ml.
To lengthen the effect of lidocaine, it is practiced to add a 0.1% solution of Adrenaline .
It is administered intravenously as an antiarrhythmic drug.
A solution of 100 mg/ml is used intravenously only after it is diluted with saline.
25 ml sol. 100 mg/ml is diluted with 100 ml of saline to obtain a concentration of 20 mg/ml. This solution is administered to the patient as a loading dose. Initially, it is 1 mg per kg of weight (injected over 2-4 minutes, the rate is 25-50 mg per minute). Next, a constant infusion is started, the rate of which is 1-4 mg/min. Next, the doctor adjusts the administration individually.
As a rule, the intravenous infusion lasts 12-24 hours, while ECG monitoring is carried out continuously.
Lidocaine spray, instructions for use
The spray must be sprayed onto the mucous membranes. The dosage depends on how large the surface area needs to be numbed. With a single spray, 4.8 mg of the active component is released. The minimum dose that provides the desired effect should be used. As a rule, the expected effect appears after 1-3 sprays. A larger number of sprays are used in obstetrics - 15-20 each, with the maximum permissible dose being 40 sprays for a patient weighing 70 kg.
The bottle should be held vertically while spraying the aerosol.
Some drugs ( Categel with lidocaine , Lidocaine Asept ) should only be administered by specialists.
If it is necessary to use an aerosol for children, it is applied with a cotton swab, as this avoids the burning sensation.
Ointment with lidocaine is applied to the surface in an amount that is determined individually.
Eye drops are used before interventions in ophthalmology; 20 mg/ml solution is instilled into the conjunctival sac. 2 drops each 2-3 times.
Lidocaine injection solution 20 mg/ml 2 ml ampoules 10 pcs. in Moscow
The administration of lidocaine should be carried out by experienced specialists in an appropriately equipped room with the availability of ready-to-use equipment and drugs necessary for cardiac monitoring and resuscitation measures. Personnel administering lidocaine must be qualified and trained in anesthesia techniques and must be familiar with the diagnosis and treatment of systemic toxic reactions, adverse events and reactions, and other complications.
Lidocaine should be used with caution in patients with myasthenia gravis, epilepsy, including a history of chronic heart failure (functional class I-II), bradycardia and respiratory depression, as well as in combination with drugs that interact with lidocaine and lead to an increase in its bioavailability and potentiation of effects (for example, phenytoin ) or prolongation of excretion (for example, in case of hepatic or end-stage renal failure in which lidocaine metabolites can accumulate) during pregnancy and during breastfeeding.
Lidocaine has been shown to cause porphyria in animals and its use should be avoided in persons with porphyria.
Patients receiving class III antiarrhythmic drugs (eg amiodarone) should be closely monitored and ECG monitoring since the effect on the heart may be potentiated.
There have been post-marketing reports of chondrolysis in patients receiving prolonged intra-articular infusion of local anesthetics after surgery. In most cases, chondrolysis was observed in the shoulder joint. Due to the many contributing factors and the inconsistency in the scientific literature regarding the mechanism by which the effect is realized, a cause-and-effect relationship has not been identified. Long-term intra-articular infusion is not an approved indication for the use of lidocaine.
Intramuscular administration of lidocaine may increase the activity of creatine phosphokinase, which may complicate the diagnosis of acute myocardial infarction.
When injected into inflamed or infected tissues, the effect of lidocaine may be reduced.
Before starting intravenous lidocaine, it is necessary to eliminate hypokalemia, hypoxia and acid-base imbalance.
Some local anesthetic procedures may cause serious adverse reactions, regardless of the local anesthetic used.
Conduction anesthesia of the spinal nerves can lead to depression of the cardiovascular system, especially against the background of hypovolemia; therefore, caution should be exercised when administering epidural anesthesia to patients with cardiovascular disorders.
Epidural anesthesia can lead to hypotension and bradycardia. The risk can be reduced by pre-administration of crystalloid or colloid solutions. Arterial hypotension must be stopped immediately.
In some cases, paracervical blockade during pregnancy can lead to bradycardia or tachycardia in the fetus, which requires careful monitoring of the fetal heart rate (see section “Use during pregnancy and breastfeeding”).
Administration to the head and neck area may result in unintentional arterial entry with the development of cerebral symptoms, even at low doses.
Retrobulbar administration may, in rare cases, result in entry into the subarachnoid space of the skull resulting in serious/severe reactions including cardiovascular insufficiency, seizure apnea, and temporary blindness. Retro- and peribulbar administration of local anesthetics carries a low risk of persistent oculomotor dysfunction. The main causes include injury and/or local toxicity to muscles and/or nerves.
The severity of such reactions depends on the degree of injury, the concentration of the local anesthetic and the duration of its exposure in the tissues. In this regard, any local anesthetic must be used in the lowest effective concentration and dose.
Lidocaine injection solution is not recommended for use in newborns. The optimal serum concentration of lidocaine to avoid toxicity such as seizures and arrhythmias in newborns has not been established.
Intravascular administration should be avoided unless directly indicated. Particular care should be taken when administering local anesthesia to organs rich in blood vessels. When injecting into vascularized tissues, an aspiration test is recommended.
Prophylactic administration to all patients with acute myocardial infarction without exception is not recommended (routine prophylactic administration of lidocaine may increase the risk of death by increasing the incidence of asystole).
If lidocaine is ineffective as an antiarrhythmic agent, it is necessary to first exclude hypokalemia. In emergency situations, it is possible to: carefully increase the dose until side effects from the central nervous system appear (lethargy, difficulty speaking); or prescribing class IA drugs (procainamide) transition to class III drugs (amiodarone bretylium tosylate).
With rapid intravenous administration, a sharp decrease in blood pressure can occur and collapse may develop. In these cases, mezaton ephedrine and other vasoconstrictors are used.
Use with caution:
- in patients with coagulopathy. Therapy with anticoagulants (eg heparin), NSAIDs or plasma expanders increases the tendency to bleeding. Accidental damage to blood vessels can lead to severe bleeding. If necessary, check the bleeding time, activated partial thromboplastin time and platelet count;
- patients with complete and incomplete block of intracardiac conduction since local anesthetics can inhibit AV conduction;
- Patients with seizure disorders should be closely monitored for CNS symptoms. Low doses of lidocaine may also increase seizure activity. Patients with Melkersson-Rosenthal syndrome may more often develop allergic and toxic reactions from the central nervous system in response to the administration of local anesthetics.
Lidocaine injection solution 10 mg/ml and 20 mg/ml is not approved for intrathecal administration (subarachnoid anesthesia).
Impact on the ability to drive vehicles. Wed and fur.:
Depending on the dose and route of administration, lidocaine may have a temporary effect on motor ability and coordination. During the treatment period, it is not recommended to drive vehicles or engage in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Overdose
If an overdose is noted, the patient’s first signs of intoxication may be nausea , dizziness , vomiting , a feeling of euphoria , asthenia , and decreased blood pressure. Later, spasms of facial muscles develop, turning into spasms of skeletal muscles. The patient also has bradycardia , psychomotor agitation, collapse, and asystole . If an overdose occurs during childbirth, the newborn may develop bradycardia , apnea , and depression of the respiratory center .
In case of overdose, it is necessary to stop administering the drug and inhale oxygen. Next, symptomatic breathing is carried out. If seizures develop, 10 mg of diazepam should be administered. In case of bradycardia, the administration of m-anticholinergic blockers (atropine) and vasoconstrictors . Hemodialysis will be ineffective.
Interaction
When used with other drugs, a number of interaction reactions may develop:
- When taking Cimetidine and beta-blockers, the risk of toxic effects increases.
- With simultaneous use, the cardiotonic effect of digitoxin .
- Enhances muscle relaxation of curare-like drugs .
- The negative inotropic effect is enhanced by concomitant administration of Verapamil , ajmaline , quinidine and amiodarone .
- The effectiveness of lidocaine is reduced by inducers of microsomal liver enzymes.
- When taking vasoconstrictors ( methoxamine , epinephrine , phenylephrine ) simultaneously, the local anesthetic effect of lidocaine may increase, and blood pressure may also increase and tachycardia .
- Lidocaine reduces the effect of antimyasthenic drugs .
- When used simultaneously with procainamide hallucinations may occur .
- Extends and enhances the effect of muscle relaxants .
- When taking mecamylamine , guanethidine , trimethaphan and guanadrel , the risk of a marked decrease in blood pressure and bradycardia increases.
- When phenytoin and lidocaine are used together, the resorptive effect of lidocaine is likely to decrease, and an undesirable cardiodepressive effect may also develop.
- When taking MAO inhibitors , the local anesthetic effect of lidocaine may be enhanced, and a decrease in blood pressure may also be observed. Parenteral lidocaine should not be prescribed to patients taking MAO inhibitors.
- polymyxin B are coadministered , it is important to monitor the patient's respiratory function.
- The inhibitory effect on respiration and the central nervous system may be enhanced if lidocaine is taken together with sedatives and hypnotics, as well as with hexenal , sodium thiopental , and opioid analgesics .
- If lidocaine is administered intravenously to people taking cimetidine, a number of negative effects may occur - drowsiness , drowsiness , paresthesia , bradycardia . If there is a need to combine these agents, it is necessary to reduce the dose of lidocaine.
- If the areas where lidocaine was injected were treated with disinfection solutions that contain heavy metals, the likelihood of local reactions increases.
special instructions
It is necessary to carry out anesthesia of highly vascularized to avoid injection into the vessels; it is recommended to conduct an aspiration test.
During treatment, it is important to drive carefully and perform other actions that require precision.
Preparations with lidocaine ( Lidocaine Asept , Kategel with Lidocaine, etc.) should be used very carefully if injuries to the mucous membranes are noted, as well as for people with mental retardation, elderly and debilitated patients.
When using the spray, it is necessary to avoid contact with the eyes and respiratory tract. Very carefully you need to apply the product to the back of the throat.
All precautions should be taken when using the spray for bikini hair removal, and also take into account contraindications when using lidocaine for toothache, lidocaine patch, etc. Experts categorically do not recommend using the spray to prolong sexual intercourse: in this case, you should use only prolongators prescribed by a doctor . It can be used for hair removal only if there is no individual intolerance to the drug.
Patients should note that this remedy cannot be used independently, without a doctor’s prescription. Ointment with lidocaine or anesthesin should also be used only as directed.
The drug should be used only at the required concentration. So, if the content of the solution is determined as 20 mg/ml, what percentage is determined simply: this is a 2% solution.
Lidocaine spray 10% –
This is a metered spray for topical use. In dentistry, it is used to relieve pain in the oral mucosa (24stoma.ru). One press sprays exactly 4.8 mg of lidocaine. The canister contains 38 grams of lidocaine, which is enough for 650 doses. The spray also contains excipients such as: 96% alcohol, peppermint oil and propylene glycol. Pleasant to the taste.
Lidocaine spray begins to act within 1 minute after spraying onto the mucous membrane, and the effect itself continues for 5-6 minutes. The drug can also be used in children under 2 years of age.
Lidocaine spray: reviews instructions lidocaine spray includes the following areas of application of the drug in dentistry -
- reduction of the gag reflex during dental treatment (spraying on the root of the tongue),
- for superficial anesthesia of the oral mucosa before local anesthesia (in this case, the injection will not be so painful).
Lidocaine spray: price You can buy lidocaine spray in almost any pharmacy with a prescription for about 350 rubles. However, as a rule, you will never be asked for a recipe.
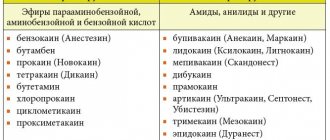
Lidocaine analogues
Level 4 ATX code matches:
Markain
Scandonest
Emla
Naropin
Versatis
Ubistezin
Ultracaine D-S Forte
Ultracaine D-S
Ultracaine
Artikain
A number of drugs are produced whose active substance is lidocaine. These products include Lidocaine-Asept spray , Lidocaine Bufus , Lidocaine-Vial , Helicaine , Xylocaine , Dinexan , Versatis , Lycaine , Strepsils Plus , etc.
A number of products are also produced with a similar effect, but with different active substances: Novocaine , Ultracaine , Tolperisone (tablets).
Lidocaine or Novocaine - which is better?
Novocaine is a medicine that demonstrates moderate analgesic activity, while Lidocaine is an effective anesthetic. However, Novocain is a less toxic drug.
Which is better: Lidocaine or Ultracaine?
Ultracaine is a less toxic drug. It provides longer-lasting anesthesia, but also has a number of contraindications for use.
Reviews of Lidocaine
Most often you can find reviews on the Internet about Lidocaine spray, they are mostly positive. Users write that the aerosol really effectively relieves pain immediately after application.
Especially often there are positive reviews about the use of hair removal . But experts do not recommend using the drug at your own discretion, for example, applying it to the head of the penis to prolong sexual contact.
There are also reviews about the effectiveness of the drug Kategel with lidocaine , which users are still advised to use under the supervision of a doctor.
Lidocaine in carpules -
All modern anesthetics have not been produced in ampoules for a very long time; they are produced in disposable capsules. The carpule already contains a dose of anesthetic; it is inserted into the carpule syringe (Fig. 1), then a disposable very thin needle is screwed on, and the syringe is ready for anesthesia.
Lidocaine carpule and carpule syringe:
An example of lidocaine anesthesia in carpules is the drug Xylonor, produced by the French company Septadont. But carpules with lidocaine are also produced by other companies. To increase the duration and depth of anesthesia, in addition to lidocaine itself, the anesthetic carpules also contain special additives (epinephrine, adrenaline or norepinephrine), which constrict the blood vessels at the site of anesthesia, thereby preventing the rapid leaching of the anesthetic.
The use of carpule syringes and carpules greatly simplifies the administration of anesthesia for the doctor, and thanks to very thin needles, it reduces pain for the patient. Read all the most detailed information on modern anesthesia in our article: “Everything about anesthesia in dental practice”
Lidocaine price, where to buy
How much ampoules cost depends on the packaging and manufacturer.
The price of Lidocaine in 10% ampoules is 40-80 rubles per 10 pieces.
You can buy Lidocaine spray 10% for a price starting from 200 rubles. A numbing spray that contains lidocaine may be more expensive. The price of Lidocaine spray in Ukrainian pharmacies is on average 200 UAH. per package.
The price of Lidocaine gel is from 200 rubles per tube.
You can buy an aerosol, cream or ointment with lidocaine at any pharmacy.
A cathegel with lidocaine costs from 145 rubles.
buy a patch with lidocaine Versatis at a price of 530 rubles.
The price of lidocaine tablets depends on the drug and its manufacturer.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Lidocaine spray for local use.
approx. 10% 650 doses 38g JSC Pharmaceutical Plant EGIS RUB 317 order - Lidocaine solution for injection. 20 mg/ml 2 ml 10 pcs. Grotex LLC
127 RUR order
- Lidocaine Bufus solution for injection. 2% 2ml 10 pcs. AO Renewal of PFC
106 rub. order
- Lidocaine Bufus solution for injection. 10% 2ml 10 pcs. AO Renewal of PFC
135 rub. order
- Lidocaine spray for topical use 10% 650 doses 38g Pharmstandard-Leksredstva OJSC
RUB 282 order
Pharmacy Dialogue
- Lidocaine Bufus (amp. 2% 2ml No. 10)Update of PFC JSC
100 rub. order
- Lidocaine (amp. 2% 2ml No. 10)Grotex LLC
115 rub. order
- Lidocaine (amp. 2% 2ml No. 10) Organics (Novokuznetsk Autonomous Okrug)
41 rub. order
- Lidocaine 2% ampoules 2ml No. 10Biosintez JSC
39 RUR order
- Katedzhel gel (tube 12.5 g with lidocaine No. 1 syringe tube) Montavit Fabrik
RUB 187 order
show more
Pharmacy24
- Lidocaine 2% 2 ml No. 100 ampoules solution ZAT FZ Egis, Ugorshchina
661 UAH.order - Cathegel with lidocaine 12.5g N1 syringe tube urethral gel Pharmaceuticalutische Factory Montavit GmbH, Austria
72 UAH order
- Lidocaine-Darnitsa 2% 2 ml No. 10 solution
13 UAH order
- Cathegel with lidocaine 12.5 g No. 5 gel Pharmaceuticals Factory Montavit GmbH, Austria
410 UAH. order
- Lidocaine hydrochloride 2% 2 ml No. 10 solution
11 UAH order
PaniPharmacy
- Lidocaine ampoule Lidocaine 20 mg/ml amp. 2ml No. 10 Ukraine, Lubnyfarm PJSC
14 UAH order
- LIDOCAINE ampoule Lidocaine solution d/in. 2% amp. 2ml No. 100 Hungary, Egis
740 UAH. order
- LIDOCAINE ampoule Lidocaine solution d/in. 2% amp. 2ml No. 10 Ukraine, Health LLC
10 UAH.order
- Katedzhel with lidocaine gel Katedzhel with lidocaine gel urethra. spr-tube 12.5 g N 1 Austria, Montavit
93 UAH order
- LIDOCAINE liquid Lidocaine spray 10% 38g Ukraine, Zdorovye LLC
199 UAH order
show more
Lidocaine in ampoules -
Available in ampoules of 2 ml. Composition of the drug: 1 ml of solution contains 20 mg of lidocaine hydrochloride (this corresponds to a 2% solution), as well as excipients - 6 mg of sodium chloride and sodium hydroxide solution, + water for injection.
Lidocaine: reviews This anesthetic once replaced novocaine, and was several times stronger than it. You need to understand that novocaine has practically no effect in inflamed tissues during suppuration. The effect of lidocaine does not depend on the presence or absence of inflammation.
Typically, a dose of 4-5 ml of lidocaine is used for anesthesia in dentistry (if lidocaine is used without the addition of adrenaline). The duration of action from the moment of injection is from 30 to 90 minutes, which depends on numerous factors: the speed of blood flow, which washes the anesthetic out of the tissues, the type of anesthesia (in the upper jaw, anesthesia lasts significantly less than in the lower jaw with conduction anesthesia).
However, now we can safely say that lidocaine, like novocaine, are anesthetics of the past. Now it has been replaced by longer-lasting and deeper-acting anesthetics based on Articaine. These anesthetics include, for example, Ultracain, Septanest, Ubistezin and others. These anesthetics are several times stronger than lidocaine, and their duration of action is also several times longer.
The undoubted advantages of lidocaine include:
- low cost, which makes it a good free anesthetic in government clinics (10 ampoules cost about 40 rubles in a pharmacy),
- antiarrhythmic effect on the heart, which makes it the drug of choice for the treatment and removal of teeth in patients with cardiac arrhythmias.