What is a cyst? Jaw cyst
A cyst is a cavity that is lined with epithelium and filled with fluid or soft material.
The formation of teeth (odontogenesis) is a complex process in which connective tissues and epithelium (enamel organ, dental follicle and dental papilla) participate.
The enamel organ refers to an epithelial structure derived from the oral ectoderm. The dental follicle and dental papilla are ectomesenchymal structures, because they are partly derived from neural crest cells.
For each tooth, odontogenesis begins with the apical (affecting the tip of the tooth root) proliferation of the epithelium of the oral mucosa, known as the dental lamina. The dental lamina gives rise to the enamel organ, a cap-shaped structure that subsequently takes on the shape of a bell. After the formation of the enamel organ, the dental lamina cord usually fragments and degenerates. However, small islands of dental lamina may remain after tooth formation. They are believed to be responsible for the development of some odontogenic cysts and tumors.
The enamel organ has four types of epithelium. The inner lining of the enamel organ is called the inner enamel epithelium and becomes the ameloblastic layer that forms tooth enamel. The second layer of cells adjacent to the inner enamel epithelium is the intermediate layer. Adjacent to this layer is the stellate reticulum, followed by the outer enamel epithelium. The enamel organ is surrounded by loose connective tissue known as the dental papilla. Contact with the epithelium of the enamel organ causes the dental papilla to produce odontoblasts, which form dentin. As odontoblasts lay down dentin, they induce ameloblasts to form enamel.
After initial crown formation, a thin layer of enamel organ epithelium, known as Hertwig's root sheath, grows at the apex of the tooth root. This epithelial expansion later becomes fragmented but leaves behind small nests of epithelial cells known as Malassez remnants in the space of the periodontal ligament. They are the source of epithelium for most periapical (radicular) cysts, but do not cause any odontogenic neoplasms, with the exception of squamous odontogenic tumor.
Keratocyst
The Center for Maxillofacial Surgery and Implantology provides treatment and removal of such a benign formation of the upper or lower jaw as a keratocyst.
What are jaw cysts, the causes of their appearance and symptoms
Prevention and treatment of dental diseases has been promoted since early childhood, so most of us approach this issue responsibly. However, few people know that other problems can arise in the oral cavity, which often require surgical intervention. We are talking about jaw cysts. According to statistics, this is not a rare phenomenon and many patients turn to dentists with this kind of problem. What is a jaw cyst and how should this pathology be treated? Types and characteristics of jaw cysts A cyst is a tissue cavity, which is lined from the inside with epithelium and filled with fluid. This neoplasm occurs as a result of degeneration of the tissue of erupting teeth or those teeth that are just developing. According to medical data, a cyst of the lower jaw is three times less common than a cyst of the upper jaw. At the same time, both a cyst of the lower jaw and a cyst of the upper jaw can lead to such unpleasant consequences as osteomyelitis, so it is necessary to treat the cyst. In dentistry, three types of jaw cysts are diagnosed: radicular jaw cyst, follicular and primordial jaw cyst (keratocyst).
We are talking about a cyst of the lower jaw that occurs at the site of the formation of a wisdom tooth. It is a soft tissue formation with thin walls, filled with a special substance - cholesteatoma. Such a cyst can be multi-chamber or single-chamber.
Its appearance is usually asymptomatic, does not cause pain or discomfort, and is most often discovered by a doctor by chance during an X-ray examination for some other reason. A cyst can develop for quite a long time, from several months to several years, without causing concern. However, if this neoplasm is detected, it is necessary to carry out appropriate treatment, otherwise the cyst may increase in size over time, multiply, become a source of infection in the oral cavity, become inflamed, and also cause destruction (resorption) of the jaw bone.
Treatment of jaw cysts
In the initial stages of keratocyst development, electrotherapy may be sufficient, and the therapist will prescribe a depophoresis procedure. If the cyst is large enough, surgical intervention is necessary, which is performed under local or general anesthesia.
To treat jaw cysts, dentists resort to surgical treatment. By performing cystostomy and cystectomy, sometimes root cysts respond well to treatment without surgical intervention. But complications of cysts and their suppuration require mandatory opening with subsequent drainage of the cavity.
The main goal of surgical treatment is to preserve the teeth located in the cyst area and restore their impaired functions. Cystectomy, in addition to opening the cyst cavity, allows for simultaneous resection of the tooth root. This procedure is carried out if the tooth root is immersed in the cyst cavity by no more than 1/3 of its entire length. If the immersion is deeper, then the teeth become unusable from a functional point of view and fall out quite early. The main disadvantage of this method is that after resection, the functionality of the teeth decreases, cases of reinfection from cut microtubules are observed, in addition, the operation is quite traumatic. The bone cavities that remain after resection reduce the strength of the jaw bones. Modern technologies can improve the cystectomy procedure. The biocomposite material used to fill the bone cavity prevents the occurrence of early complications. This is due to the absence of a blood clot, which significantly reduces infection of the cavity. Biocomposite materials, filling the cyst cavity, help restore the shape and function of the jaw by accelerating regeneration.
The prognosis after surgical treatment is favorable, however, large jaw cysts can be complicated by pathological fractures of the jaw.
At the Center for Maxillofacial Surgery and Implantology, this operation is performed by surgeons of the highest category using the most modern equipment and the latest anesthetics. In difficult cases, postoperative rehabilitation can be carried out in the Center’s own hospital. Cozy rooms, comfortable conditions and constant medical supervision will make the recovery period easy and enjoyable for the patient.
Why do jaw cysts form?
Odontogenic cysts (developing or inflammatory) get their name from the nature of their origin. Most jaw cysts are lined by epithelium, which is derived from odontogenic epithelium.
The occurrence of such cysts is usually associated with unerupted teeth (third molars of the lower or upper jaw, second premolars of the lower jaw, and canines of the upper jaw). They can also form near additional teeth and in combination with odontomas. The occurrence of odontogenic cysts is rarely associated with baby teeth.
Most often, jaw cysts are discovered between the ages of 10 and 30 years. Men, especially white-skinned men, suffer from them more often.
In most cases, dental cysts do not manifest themselves in any way and are an accidental finding obtained during an X-ray examination. But, in some cases, they can reach significant sizes, which lead to the expansion of bone tissue, but even they may not give pronounced symptoms until a secondary infection occurs.
Treatment of jaw keratocysts using demineralized bone matrix in combination with platelet-rich blood plasma
The International Histological Classification of Tumors (IGCT) WHO No. 5 (1971) among odontogenic cysts of the jaws identified a primary cyst - a keratocyst, which is a malformation of the dental epithelium and develops in the tooth-containing areas of the jaws.
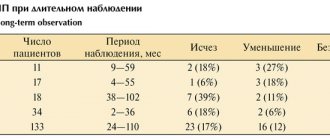
In the latest histological classification of odontogenic tumors WHO (2005) - Pathology and Genetics, Head and Neck Tumors - keratocysts are classified as tumors and are called “benign keratocystic odontogenic tumor”. It is of non-inflammatory origin and is a malformation of the residual elements of the dental plate [10,13]. Keratocysts develop in tooth-containing areas of the jaws: on the upper jaw, it is more common in the frontal region, especially in the canine area, and on the lower jaw, in the posterior part or behind the third molar of the lower jaw, spreading to the ramus [1,15]. Odontogenic keratocystic tumors (OCT) of the jaw bones, according to various authors, account for from 5.4 to 17.4% of all odontogenic cysts [6,11]. In some cases, keratocysts are included in the symptom complex of congenital pathologies (Gorlin syndrome, Marfan syndrome, etc.). They can mimic other lesions, complicating diagnosis based only on clinical and radiological examination [3]. Radiologically, odontogenic keratocysts can be unilocular or multilocular [8]. Odontogenic keratocyst is of great interest, mainly due to its tendency to recur [5,16]. According to the literature, the percentage of relapses varies from 0 to 62.5% depending on the chosen method of surgical treatment [14,19]. After cystotomy, this figure can be 40% [18], after cystectomy - 17.79-54.5% [14], while after enucleation with peripheral ostectomy and block resection of the jaw it ranges from 0-2% [14,18,19 ]. Different authors see different reasons for relapse. According to some [8], a possible explanation for relapses is the aggressiveness of the cyst, due to the activity of collagenase in the cyst wall and high fibrinolytic activity. Other authors pay special attention to the infiltration of soft tissues, growth into the periosteum, proliferation of the epithelial lining [2,13], residual elements of the dental plate that can form new cysts, the type of keratinization (parakeratinized cysts are more aggressive and prone to relapse) [7, 12.17].
A variety of surgical techniques have been proposed for the treatment of keratocysts. T. Buge and J. Zakrzewska [7], having reviewed the treatment methods described by various authors, proposed their classification: 1. cystectomy: with primary closure, with filling of the defect area, with chemical treatment, with cryodestruction; 2. cystotomy: isolated, two-stage followed by cystectomy; 3. resection of the jaw. R. Brasley [4] developed indications for various surgical methods: small single-chamber cysts should be removed entirely from intraoral access; for large cysts in hard-to-reach areas, decompression through cystotomy with secondary cystectomy is recommended; Large multi-chamber cysts have been proposed to be treated by resection with primary bone grafting.
For the period 2003-2009. We observed 16 patients with 16 odontogenic keratocystic tumors (OKT). The age of the patients ranged from 16 to 62 years. Of the total number of patients, 10 (62.5%) were men and 6 (37.5%) were women. The male to female ratio was 1.67:1. Of all 16 ACOs, 15 (93.75%) were observed in the lower jaw and 1 (6.25%) in the upper jaw. Of the 15 patients with ACO of the lower jaw, in 10 they were localized in the area of the angle and ramus, in 4 in the molar area and in 2 in the chin. In one patient, the OCO was located on the upper jaw interradicularly, between the 23rd and 24th teeth.
The cyst was more often discovered by chance - in 9 patients during an X-ray examination for other diseases of the maxillofacial region, two patients were referred by the attending dentist with an erroneous diagnosis of “follicular cyst in the area of the angle of the lower jaw with an impacted wisdom tooth,” 4 were referred with complaints of facial asymmetry due to slight bulging of the cortical plate of the lower jaw, and one patient complained of painless swelling of the gums, measuring about 1 cm in diameter, in the upper jaw area on the left. The X-ray picture of the disease was characterized by the presence of a cyst-like formation, often extensive, with clear, often polycyclic contours, multi-chamber. Radiographs revealed the periodontal gap of the tooth roots projecting onto the area of the cyst. Despite the extensive intraosseous lesion, no pronounced deformation of the jaw was noted, which is explained by the spread of the process along the length of the bone in the form of a single cavity. The diagnosis of ACO was based on clinical and radiological data and was confirmed by pathohistological examination of the surgical material.
Fig.1. Orthopantomogram of patient S. before treatment
In 9 patients with extensive keratocysts of the lower jaw, the operation was performed under general endotracheal anesthesia, and in 7 patients with small cysts up to 2 cm, under local anesthesia on an outpatient basis. In 9 patients with extensive keratocysts, with invasion into the surrounding soft tissue, a segmental resection of the lower jaw was performed without breaking the continuity of the bone, moving 1 cm from the edges of the cystic lesion. Macroscopically, upon opening the CTO, a single cavity was found, filled with a grayish-dirty keratin mass, which is a product of desquamation and the vital activity of the keratinizing epithelium of the cyst shell. The resulting bone defect was restored in all cases simultaneously with DCM in the form of blocks and in crushed form in combination with PRP. To prevent bone fractures in these patients, teeth were splinted with intermaxillary fixation. Patients with small cysts underwent cystectomy with mandatory peripheral osteoectomy to avoid relapses. The cyst shell was thin and easily ruptured during enucleation. When ACOs grew into soft tissues, they were excised. In two cases, in addition to the use of osteoplastic material, a beeswax membrane was used for targeted tissue regeneration. A morphological study was carried out in all patients. The OCO shell was represented by fibrous connective tissue with a predominance of collagen fibers and was lined with multilayered epithelium. In multilayered epithelium, phenomena of keratinization such as parakeratosis and orthokeratosis were observed. The postoperative period in 14 patients proceeded smoothly, without complications. In 1 patient, suppuration of a bone wound with suture dehiscence was observed. After adequate conservative therapy, the inflammatory process was stopped. Long-term postoperative observations from 3 to 9 years showed no relapses in any case. In all cases, the bone defect was restored with the formation of organotypic bone within a period of 3 to 12 months. depending on the size of the latter.
For example, here is a clinical case
Fig.2. Orthopantomogram of the patient two years after surgery.
Patient S. 49 years old. entered the department of maxillofacial surgery med. 03/30/2009 with complaints of numbness of the lower lip and chin on the right for the last 3-4 months. I contacted the dentist about planned sanitation of the oral cavity, and an orthopantomogram taken at the stoma. clinic, cystic formations were discovered in the area of the body and branches of the lower jaw. The patient was sent for inpatient examination and treatment. During external examination, no facial asymmetry was noted. The skin color is not changed, the mouth opens freely. There were no visible pathological changes in the oral cavity. An orthopantomogram showed a clearing in the area of the angle and ramus of the lower jaw with clear polycyclic contours, surrounded by a sclerotic rim. The heterogeneity of the shades of clearing created a picture of a multi-chamber cystic formation. On the left side, in the area of the body of the lower jaw, a cystic formation was observed with clearer contours, rounded shape and uniformity. The dimensions of the cystic cavity on the right are about 7x5 cm, on the left about 4.5 cm in diameter (Fig. 1).
The operation was performed on April 2, 2009. under general endotracheal anesthesia through external access. An arcuate incision was made in the area of the angle and body of the lower jaw on the right, 2.5 cm below the lower edge, 6-6.5 cm long (Fig. 3a). Soft tissues are dissected layer by layer down to the bone. After separating the periosteum, a tuberous, slightly swollen outer cortical plate of the lower jaw ramus was visible (Fig. 3b). Under cooling saline solution, the outer cortical plate was drilled and removed (Fig. 3v). Macroscopically, the cyst cavity was filled with a grayish-dirty keratin mass (Fig. 3d). After careful enucleation of the cyst, resection of the lower jaw was performed, retreating 0.5-1 cm from the tumor boundaries, maintaining the continuity of the lower jaw in the area of its posterior edge (Fig. H). The resulting defect was filled with crushed allogeneic DCM in combination with PRP and covered on top and isolated from the surrounding soft tissues with a beeswax membrane for the purpose of directed bone regeneration (Fig. 3, g, h). From the side of the oral cavity was removed
Fig.3. Stages of the operation: a) the incision line is marked, b) the outer surface of the bone is exposed, c) drilling of the cortical plate d) the keratocyst shell is visible, e) resection of the lower jaw is performed, f) filling the defect with crushed DCM with PRP, g, h) application of a membrane from beeswax over osteoplastic material, i) the wound is sutured in layers, leaving a rubber graduate, j) the body of the lower jaw is exposed on the left, k) the cystic cavity is filled with DCM with PRP, m) a wax membrane is applied.
46 periodontitis tooth. The wound was sutured in layers, leaving a rubber graduate (Fig.Zi). A similar operation was performed on the left side using an extraoral approach, with the only difference being that when the outer cortical plate was removed, the shell of a radicular cyst with cystic contents was revealed. A cystectomy with apecectomy of the 35th tooth was performed. The residual bone cavity was filled with allogeneic DCM with PRP and isolated from the periosteum with a beeswax membrane (Fig. 3 j, l, l).
Two years (Fig. 2, 4) after the operation the patient had no complaints. There was no external facial asymmetry observed. An orthopantomogram showed restoration of bone tissue in the area of the defect, although in the central parts of the defect the density of the newly formed bone was inferior to that of the mother.
Rice. 4 Appearance of the patient two years after surgery
Thus, our data coincide with the literature, indicating the absence of relapses during surgical treatment with resection of the jaw bone, or cystectomy with peripheral osteoectomy. Despite the traumatic nature of this method of intervention, with the possibility of intraoperative damage to anatomical structures (nerve damage, bone fracture), today it is the most reliable in terms of preventing relapses and malignancy, as also evidenced by a number of authors [2,7, 19, 20]. And restoration of the resulting defect with allogeneic or xenogeneic DCM, in combination with PRP, promotes rapid wound healing, acceleration of the processes of reparative regeneration of bone tissue, which shortens the period of postoperative rehabilitation of patients.
Bibliography
- Gubaidulina E.Ya., Tsegelnik L.N., Bashilova R.A., Komnova Z.D. Odontogenic primary cyst (keratocyst) of the jaws. Dentistry. 1986; No. 1: pp. 41-45.
- Chernigovskaya V.N. Keratocysts of the jaw bones in children. Auto. Candidate of Medical Sciences M., 2009.18 p.
- Ali M, Baughman RA. Maxillary odontogenic keratocyst: a common and serious clinical misdiagnosis. J Am Dent Assoc. 2003;134(7):877-83.
- Bramley PA The odontogenic keratocyst: an approach to treatment. J Oral Surg 1974;3:337-41.
- Brannon RB. The odontogenic keratocyst. Part I. Oral Surg Oral Med Oral Pathol. 1976;42:54-72.
- Cawson RA, Binhie WH, Speight PM, Barrett AW, Weight JM Lucas pathology of tumors of the oral tissues. 5th ed. London Churchill Livingstone.1998, p. 25-44.
- Chemli H, Dhouib M, Karray F, Abdelmoula M. Risk factors for recurrence of maxillary odontogenic keratocysts. Rev Stomatol Chir Maxillofac. 2010 Sep;l 11(4): 189-92.
- Donath K. Cysts and tumors of the jaw bone. Verh Dtsch Ges Pathol. 1992;76:360-5.
- Eyre J., Zakrzewska YM British J Oral Maxillofac Surg. 1985. vol.23, 3; p.195-203.
- Kramer IR, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumors. Cancer.1992;70(12):2988-94.
- Kreidler J., Raubenheimer E., van Heerden W. A retro spective analysis of 367 cystic lesions of the jaws of the Ulm experience. J. Craniomaxillofac Surg. 1993.21:339-41.
- Lam KY, Chan AC. Odontogenic keratocyst: a clinico-pathological study in Hong Kong Chinese. Laryngoscope, 2000; 110:1328-32.
- Li TJ. The odontogenic keratocyst: a cyst, or a cystic neo-plasm? J Dent Res. 2011 Feb;90(2): 133-42.
- Morgan TA, Burton CC, Qian T. A retrospective review of treatment of the odontogenic keratocyst J Oral and Maxillofac Surg. 2005; vol.63(5): p.635-639.
- O'Neill R, Al-Hezaimi K. Identification of an odontogenic keratocyst and treatment with guided tissue regeneration. J Can Dent Assoc. 2011;77:b6.
- Shear M. Developmental odontogenic cysts: an update. J Oral Pathol Med. 1994;23:1-11.
- Wright JM. The odontogenic keratocyst: orthokeratinized variant. Oral Surg. 1981;51:609-18.
- Zecha JA, Mendes RA, Lindeboom VB, van der Waal I. Recurrence rate of keratocystic odontogenic tumor after conservative surgical treatment without adjunctive thera-pies. Oral Oncol. 2010 Oct;46(10): 740-2.
- Zhao YF, Jin-Xiong W, Wang SP. Treatment of odonto-genic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:151-6.
- Zhou JL, Jiao SL, Chen XH, Wang YL Treatment of recurrent odontogenic keratocyst with enucleation and cryosurgery. Shanghai Kou Qiang Yi Xue. 2005Oct;14(5):476-8.
How do jaw cysts appear?
In most cases, the cyst does not cause significant symptoms. Its development can be provoked by incorrect treatment of dental diseases or caries.
Odontogenic cysts are usually distinguished by type of origin:
· dentofacial cysts – their occurrence is associated with the crown of a tooth that could not erupt;
· keratocysts – are a consequence of Nevoid basal cell carcinoma syndrome;
radicular or radicular cysts – are of inflammatory origin and most often result from a reaction to necrosis of the dental pulp;
· bifurcation buccal cyst – typical for children 5-10 years old, it is formed in the area of buccal bifurcation of the first molars of the lower jaw;
· primary cyst – in most cases it is a keratocystic odontogenic tumor;
· orthokeratinized cyst – also refers to a subtype of keratocystic odontogenic tumor;
· eruption cyst – usually formed from a degenerating dental follicle and forms in the gum when the tooth erupts;
· newborn gum cyst – formed from the remains of the dental plate on the gum of a newborn;
· adult gingival cyst – is a variant of the lateral periodontal cyst;
· lateral periodontal – a non-inflammatory cyst on the side of the tooth, formed from the remains of the dental plate;
· calcifying cyst is a rather rare pathology, which is characterized by cystic and neoplastic signs;
· glandular cyst is a formation with a respiratory epithelial lining and potential relapse; in its manifestations it is similar to the central variant of poorly differentiated mucoepidermoid carcinoma.
Odontogenic cysts are difficult to detect at an early stage. It gives virtually no symptoms. The patient may be alarmed by tooth displacement or a change in the color of the diseased tooth. If the cyst has reached a significant size, the patient may notice protrusion of the bone structures.
A long asymptomatic course can lead to the formation of inflammatory processes, which are dangerous due to the development of suppuration and can provoke pathological fractures of the jaw bones.
If a cyst has formed in the upper jaw, it can cause nosebleeds, headaches and impaired nasal breathing.
The main symptoms associated with the presence of an odontogenic cyst (pain, fever, inflammatory changes in the oral cavity) usually appear in the later stages of the disease.
Differential three-dimensional diagnosis of keratocysts of the jaws
M. A. Chibisova
Doctor of Medicine, Professor, Rector, Head of the Department of Radiology in Dentistry, Private Educational Institution "SPbINSTOM" (St. Petersburg), Chairman of the StAR section "Radiation diagnostics in dentistry"
A. A. Zubareva
Doctor of Medicine, Professor of the Department of Otorhinolaryngology with the clinic of PSPbSMU named after. acad. I. P. Pavlova, Professor of the Department of Radiology in Dentistry SPbINSTOM (St. Petersburg)
A. L. Dudarev
Doctor of Medical Sciences, Professor of the Department of Radiology in Dentistry SpbINSTOM (St. Petersburg)
A. V. Kholin
Doctor of Medical Sciences, Professor, Head of the Department of Radiation Diagnostics of North-Western State Medical University named after. I. I. Mechnikova (St. Petersburg)
E. V. Kaizerov
Assistant at the Department of Radiation Diagnostics of North-Western State Medical University named after. I. I. Mechnikova (St. Petersburg)
R. Kh. Charyev
postgraduate student of the Department of Maxillofacial Surgery and Surgical Dentistry of PSPbSMU named after. acad. I. P. Pavlova (St. Petersburg)
Summary
The use of modern methods of radiation diagnostics is also justified in the postoperative period for dynamic analysis of the recovery period of patients with keratocysts of the jaws. The use of modern high-tech methods of radiation diagnostics, such as digital orthopantomography (OPT, OPTG), spiral (MSCT) and cone-beam computed tomography with dynamic densitometry (CBCT, 3DCT, 3DCT), along with a detailed analysis of clinical and histological data, can significantly improve the quality assessment of the state of the dental system in normal conditions and in the detection of pathological processes. Three-dimensional tomography (MSCT and CBCT) allows for differential diagnosis between types of cystic formations, analysis of the extent of spread of the pathological process to surrounding tissues and determination of the most appropriate method of surgical intervention, including in patients with jaw kertocysts.
Keywords:
keratocyst, odontogenic cysts of the jaws, cone beam computed tomography (CBCT, 3DCT, 3DCT), multispiral X-ray computed tomography (MSCT).
Introduction
Keratocysts of the jaws, according to various authors, make up from 5.4 to 17.4% of all odontogenic cysts [2, 5, 11]. Up to 10% of patients are treated in specialized dental institutions for treatment of keratocysts of the jaws. Keratocysts are prone to recurrence, which occurs as a result of incomplete removal of the epithelial lining of the cyst. The cause of relapses is also the high activity of collagenase in the cyst wall and high fibrinolytic activity [1, 2].
Keratocyst belongs to the group of odontogenic dysembryogenetic cysts (international histological classification of odontogenic tumors, cysts and other tumor-like formations of the jaw bones WHO, Geneva, 1972), is a malformation of the maxillofacial region, is formed as a result of impaired differentiation of the epithelium of the enamel organ during ontogenesis, histologically represents It is a bone cavity lined with keratinized multilayer epithelium [2, 6, 7, 11].
Despite the rapid development of radiological diagnostic methods in recent decades, the emergence of spiral CT, as well as cone-beam dental volumetric tomography, there are no clear differential diagnostic criteria for determining the nature of cystic formation of the jaws [8, 9]. The main routine method of radiology diagnostics in dentistry is still orthopantomography and its digital improvement, which, of course, allows one to obtain a lot of useful information on the state of the dental system, including for the assessment of cystic formations [10]. However, despite the advantages of OPTG as a widespread, economically feasible and fairly informative method of radiological diagnostics in dentistry, there are a number of limitations and errors of this method that do not allow reliable interpretation of all possible radiological signs of a cystic formation [1-5].
Rice. 1. Keratocyst of the angle and ramus of the lower jaw on the left. MSCT. Rice. 2. Keratocyst of the body, angle and ramus of the mandible. Clear uneven external contour, lobular structure, pseudosepta. 3DCT. Rice. 3. Keratocyst of the body, angle and ramus of the mandible with extension to the condylar and coronoid processes. Size 63 mm. MSCT.
Histologically, there are two variants of the structure of keratocysts: parakeratotic and orthokeratotic. The parakeratotic variant is the most common, the most aggressive in terms of the rate of growth and destruction of bone tissue, as well as the frequency of relapses, and is represented by 5-7 layers of epithelium with a characteristic basal layer, the cells of which are cubic or cylindrical in shape with a vertical arrangement of hyperchromic nuclei. The cyst wall is represented by loose connective tissue with swelling of the subepithelial parts without inflammatory infiltration. In the orthokeratosis variant, the epithelium is more thickened, without a clearly defined basal layer, with a large area of the superficial part in a state of true keratosis [11].
Purpose of the study
The purpose of our study was to develop differential diagnostic clinical and radiological criteria for diagnosing “keratocyst” using clinical data from a dental examination of the patient, as well as the capabilities of computed tomography methods, such as densitometry of the contents of the cystic cavity, surrounding bone tissue and soft tissues of the jaw area in the perifocal zone, the degree of destruction of the spongy bone substance of the jaws, cortical plates, metric indicators of the cystic cavity in three dimensions, the direction of cyst growth, connection with the teeth, neurovascular structures of the jaws. The data obtained can be used for the optimal choice of treatment method, the extent of surgical intervention in order to preserve the jaw bone, temporomandibular joint, teeth as much as possible, and prevent damage to the neurovascular formations of the jaws.
Rice. 4. Keratocyst contents: soft tissue component + air. Extensive defect of the vestibular cortical plate of the body of the lower jaw. MSCT. Rice. 5. Immersion of intact roots into the cyst. MSCT.
Materials and methods
The results of clinical and computed tomographic examination (digital OPTG, MSCT and dental volumetric tomography) of 46 patients with keratocysts of the jaws, confirmed by cytohistological examination data, were analyzed. The analysis was carried out using three formalized charts: clinical (complaints, anamnesis, objective examination data), 3D-CT cystogram (x-ray semiotics of keratocysts), local densitometry in various zones (using HU units for MSCT and UE for dental volumetric tomography). This group of patients was assessed according to the following clinical and radiological criteria: frequency distribution of keratocysts in different age groups, gender distribution, disease history (duration of the cyst, its growth rate, connection with carious teeth, pain), localization in various parts of the lower jaws, jaw deformation, condition of the mucous membrane, gum pockets, presence of teeth in the projection of the cyst and the condition of their roots, metric characteristics of keratocysts in three dimensions, densitometric characteristics of the contents of the cyst, capsule and surrounding bone structures and soft tissues, condition of the surrounding bone tissue, presence of defects cortical plates, impact on the mandibular canal, temporomandibular joint.
Results and discussion
Table No. 1. Distribution of keratocysts by age in men
| Age | Abs. (n-25) | % |
| 10—20 | 4 | 16 |
| 21—30 | 3 | 12 |
| 31—40 | 6 | 24 |
| 41—50 | 3 | 12 |
| 51—60 | 6 | 24 |
| 61—70 | 2 | 8 |
| 71—80 | 1 | 4 |
Table No. 2. Distribution of keratocysts by age in women
| Age | Abs. (n-21) | % |
| 10—20 | 1 | 4.8 |
| 21—30 | 6 | 28.6 |
| 31—40 | 6 | 28.6 |
| 41—50 | 1 | 4.8 |
| 51—60 | 1 | 4.8 |
| 61—70 | 4 | 19 |
| 71—80 | 2 | 9.5 |
Data from tables No. 1 and 2 demonstrate that keratocysts were diagnosed in men aged 11 to 74 years (25 cases) and women aged 13 to 76 years (21 cases). The highest incidence of keratocysts in men is between the ages of 30 and 60 years - 15 (60%), in women - from 20 to 40 years - 12 (57.2%).
Table No. 3.
Clinical symptoms of keratocysts
| Symptoms | Number of observations | ||
| Abs. (n-46) | % | ||
| Complaints | No complaints, the cystic cavity was detected during a routine radiation examination | 16 | 34.8 |
| Complaints of swelling and deformation of the lower jaw | 30 | 65.2 | |
| Pain when opening mouth | 6 | 13 | |
| Objective dental examination data | Swelling of the jaw along the transitional fold | 30 | 65.2 |
| Scanty purulent discharge from the gum pockets. | 6 | 13 | |
| Adentia in the keratocyst projection | 23 | 50 | |
| Pathological mobility of teeth in the projection of the cyst | 20 | 43.5 | |
| On palpation, thinning of the cortical plates of the lower jaw, their crepitus | 19 | 41.3 | |
| On palpation, defects in the cortical plates of the lower jaw | 9 | 19.6 | |
| Electroodontometry of teeth in the projection of the cyst corresponded to intact teeth (2-6 μA) | 42 | 91.3 | |
| Electroodontometry indicators deviated from the norm (6-20 µA) | 4 | 8.7 | |
| Concomitant inflammatory pathology | Gingivitis | 1 | 2.2 |
| Trigeminal neuralgia | 3 | 6.5 | |
As the data in Table No. 3
, in a third of cases, 16 (34.8%), there were no complaints. The diagnosis was made by X-ray examination. Complaints of swelling and deformation of the jaw were typical - 30 (65.2%). Only 6 (13%) patients complained of pain. Characteristic signs during the dental examination were swelling of the jaw along the transitional fold - 30 (65.2%), adentia in the projection of the cyst - 23 (50%), pathological mobility of teeth in the projection of the cyst - 20 (43.5%), crepitus - 19 (41.3%) and defects of cortical plates - 9 (19.6%) upon palpation. Electroodontometry data in 42 (91.3%) cases corresponded to standard values. Not a single case of deep dental caries in the projection of the cyst has been recorded.
At the stage of radiological diagnostics using digital OPTG, spiral CT and dental volumetric tomography, the following data were obtained.
Table No. 4. Syndromic and symptomatic X-ray computed tomographic characteristics of jaw keratocysts
| RCT symptoms | Number of observations | ||
| Abs. (n-46) | % | ||
| Localization | Body of the mandible at the level of the premolars | 4 | 8.7 |
| Body of the mandible at the level of the molars | 6 | 13 | |
| Mandibular angle | 8 | 17.4 | |
| Branch of the mandible | 5 | 10.9 | |
| Body, angle and ramus of the mandible | 9 | 19.6 | |
| Body and angle of the mandible | 7 | 15.2 | |
| Angle and ramus of the mandible | 6 | 13 | |
| Form | single-chamber | 15 | 32.6 |
| multi-chamber | 5 | 10.9 | |
| lobular | 26 | 56.5 | |
| Dimensions | <10 mm | 5 | 10.9 |
| 10—30 mm | 12 | 26.1 | |
| >30 mm | 29 | 63 | |
| Outlines | Internal: | ||
| Smooth | 17 | 37 | |
| Uneven | 29 | 63 | |
| Clear | 39 | 84.8 | |
| Fuzzy | 7 | 15.2 | |
| External: | 7 | 17 | |
| Smooth | 19 | 41.3 | |
| Uneven | 27 | 58.7 | |
| Clear | 39 | 84.8 | |
| Fuzzy | 7 | 15.2 | |
| Sclerotic | 7 | 15.2 | |
| Structure | Homogeneous: | 21 | 45.7 |
| Fat-like tissue | 4 | 8.7 | |
| Liquid | 5 | 10.9 | |
| Soft fabrics | 12 | 26.1 | |
| Heterogeneous: | 25 | 54.3 | |
| Fat-like tissue + air | 6 | 13 | |
| Fibrous tissue + air | 2 | 4.3 | |
| Soft fabrics + air | 8 | 17.4 | |
| Liquid + air | 4 | 8.7 | |
| Soft tissue + fibrous tissue + air | 5 | 10.9 | |
| Condition of surrounding tissues | Displacement of the mandibular canal | 19 | 41.3 |
| Defect of the wall of the mandibular canal | 13 | 28.3 | |
| Consolidation of surrounding soft tissues | 5 | 10.9 | |
| Presence of fibrous capsule | 25 | 54.3 | |
| Adentia in the projection of the cyst | 23 | 50 | |
| Immersion of the root into the cystic cavity | 12 | 26.1 | |
| Lysis of tooth roots in the projection of the cyst | 5 | 10.9 | |
| Divergence of tooth roots in the projection of the cyst | 7 | 15.2 | |
| Bloating of the jaw | 30 | 65.2 | |
| Thinning of the cortical plates | 46 | 100 | |
| Cortical plate defect | 37 | 80.4 | |
| Direction of cyst growth | Along the long axis of the jaw, extending over 1 tooth | 5 | 10.9 |
| Along the long axis of the jaw, extending over 2 teeth | 12 | 26.1 | |
| Along the long axis of the jaw, extending to 3 or more teeth | 29 | 63 | |
| Along the long axis of the jaw, extending to the coronoid and condylar processes | 3 | 6.5 | |
The data in Table No. 4 demonstrate that the typical localization of keratocysts was the body of the lower jaw at the level of premolars and molars, the angle and ramus of the lower jaw, and due to the large size of the keratocyst, it spread to two - 13 (28.3%) - or three sections of the lower jaw - 9 ( 19.6%), and in three cases reached the condylar and coronoid processes (6.5%).
Keratocysts are characterized by a lobulated structure of the cystic cavity - 26 (56.5%) with pseudosepta, which are formed by keratin masses (Fig. 1-2). A single-chamber structure was observed with small sizes of the cystic cavity (with sizes less than 10 mm in 100% of cases, with sizes of 10-30 mm in 30% of cases).
In the observations, keratocysts measuring more than 30 mm predominated - 29 (63%), keratocysts measuring 10-30 mm - 12 (26.1%). A cystic cavity less than 10 mm in size occurred in 5 cases (10.9%).
The internal contours of the cyst are clear in most cases - 39 (84.8%), uneven - 29 (63%). The external contours of the cyst were also clear in most cases - 39 (84.8%), uneven - 27 (58.7%).
In more than half of the observations, heterogeneous contents of keratocysts were revealed - 25 (54.3%). Among keratocysts with homogeneous contents, the soft tissue component predominated - 12 (26.1%) (Fig. 3
-
4).
Characteristic was swelling of the lower jaw, which was observed in 2/3 of the subjects - 30 (65.2%) with thinning - 46 (100%) and defects - 37 (80.4%) of the cortical plates ( Fig. 5
). A common sign of keratocyst of the mandible was pushback (19 (41.3%)) or partial destruction (13 (28.3%)) of the wall of the mandibular canal.
The characteristic direction of growth of keratocysts is along the long axis of the lower jaw, spreading to 3 or more teeth - 29 (63%). Immersion of the root into the cystic cavity was observed in 12 (26.1%) patients (Fig. 5). In 5 (10.9%) cases, partial lysis of the root embedded in the cyst was observed. In the keratocyst area, half of the patients—23 (50%)—had secondary adentia.
Table No. 5. Densitometric characteristics of the contents of keratocysts
| Structure | X-ray density | Number of observations | ||
| HU | u. e. | abs. (n-46) | % | |
| Homogeneous | 21 | 45.7 | ||
| Fat-like tissue | -30 to -180 | 1350—1450 | 4 | 8.7 |
| Liquid | From 13 to 17 | 1300—1400 | 5 | 10.9 |
| Soft fabrics | From 25 to 40 | 1350—1500 | 12 | 26.1 |
| Heterogeneous: | 25 | 54.3 | ||
| Fat-like tissue + air | From -30 to -180, -1000 | 1350—1450, 650—950 | 6 | 13 |
| Fibrous tissue + air | From 56 to 69, -1000 | 650—950 | 2 | 4.3 |
| Soft fabrics + air | From 25 to 40, -1000 | 1350—1500, 650—950 | 8 | 17.4 |
| Liquid + air | From 13 to 17, -1000 | 1300—1400, 650—950 | 4 | 8.7 |
| Soft tissue + fibrous tissue + air | From 25 to 40, from 56 to 69, -1000 | 1350—1500, 1400—1550 650—950 | 5 | 10.9 |
Along with studying the features of 3D X-ray CT images of keratocysts, we studied quantitative densitometric parameters. In table No. 5
it is demonstrated that, according to local densitometry, the contents of keratocysts were represented by a fat-like component - 4 (8.7%), liquid - 5 (10.9%) and a soft tissue component - 12 (26.1%). In more than half of the cases, the contents were heterogeneous, with an admixture of air - 25 (54.3%).
Conclusion
Spiral computed tomography and dental volumetric tomography (CBCT), taking into account the clinical features of the development of keratocysts, provide more complete information about the cystic formation of the jaws due to the possibility of three-dimensional visualization, assessment of size and localization without errors associated with patient positioning and projection distortions, more accurate assessing the condition of cortical plates at different levels in different projections in order to accurately determine cortical defects. These methods make it possible to obtain detailed information about the relationship between the cystic cavity and such important anatomical structures as the mandibular canal and condylar process. The use of local densitometry makes it possible to quantitatively assess the contents of the cystic cavity, the condition of the capsule, surrounding bone tissue and soft tissues, signs of the presence of osteoreparative processes, as well as the condition of the roots of the teeth involved in the pathological process.
conclusions
The result of our study was the development of detailed clinical and radiological semiotics of mandibular keratocysts using radiological symptoms, densitometric data and clinical examination data.
As a result of the study, it can be concluded that keratocysts are more common at a young age, are localized mainly in the body, angle and ramus of the lower jaw at the level of the molars, do not have significant clinical manifestations, with the exception of gradually increasing deformation of the jaw, are large in size, have irregular form due to distribution along the long axis of the jaw and high osteolytic activity, are not associated with carious teeth, although they can cause lysis of tooth roots, lead to the formation of extensive defects in the cortical plates, and are prone to pushing back and lysis of the walls of the mandibular canal.
How are odontogenic cysts diagnosed?
The leading method for identifying odontogenic cysts is radiography, which is capable of visualizing jaw cysts at an early stage of their development. On an x-ray image, the cyst is distinguished by the presence of clear boundaries, and the formation itself gives a characteristic shadow of a round or oval shape, immersed in the sinus of the tooth root.
Ultrasound examination also helps to recognize odontogenic cysts.
As already mentioned, pronounced symptoms are characteristic of the late stage of development of a pathological formation, therefore it is difficult to diagnose a cyst at the initial stage, relying only on symptoms.
The final diagnosis is made on the basis of histological examination. It is important to differentiate an odontogenic cyst from other pathologies (adenomatoid odontogenic tumor, ameloblastic fibroodontoma and calcifying epithelial odontogenic tumor).
The CT scan method is widely used in the diagnosis of jaw cysts to confirm the presence of calcifications along the wall of the cyst, as well as tiny spots that are usually not found on x-rays. In addition, computed tomography is necessary during the surgical planning stage.
Multiple jaw cysts: Gorlin-Goltz syndrome
Gorlin-Goltz syndrome, also known as Nevoid Basal Cell Carcinoma Syndrome (NBCS), is a multisystem disorder first described by Gorlin and Goltz. The incidence of this disease is estimated at 1 case per 50,000-150,000 people and depends on the specific region. This rare autosomal dominant disease is characterized by disruption of several organs and systems, which affects the skeleton, eyes, skin, reproductive and nervous systems. However, all of the above symptoms are rarely observed simultaneously in one patient. The pathogenesis of the syndrome is associated with a violation of the long arm of chromosome 9 (q22.3-Q31) of the pTCH1 gene, the clinical symptoms of which do not appear in a heterogeneous ratio. The main clinical signs appear in the form of multiple odontogenic keratocysts, basal cell nevi and skeletal abnormalities. This article presents a case of a 16-year-old patient who sought treatment for multiple odontogenic keratocysts, which was subsequently diagnosed as Gorlin-Goltz syndrome. This example highlights the need and importance of a thorough clinical and radiographic examination of patients with jaw cysts.
Clinical case
A 16-year-old patient presented to the Department of Oral Medicine and Radiology, Institute of Dental Sciences, Belgaum, with the chief complaint of swelling in the left posterior region of the mandible for the last 15 days. It turned out that the swelling appeared suddenly, without accompanying attacks of pain or any discharge. The patient's medical history, family history and available dental data did not reveal any facts that could provoke or be associated with this pathology. During a general somatic examination, it was found that the patient was of average build, normally well-nourished, with a normal gait; kyphosis was also diagnosed. Extraoral examination revealed facial asymmetry, prognathism of the lower jaw, hypertelorism and strabismus of the left eye (Figure 1). During the intraoral examination, a swelling measuring 3 cm × 1 cm was discovered, occupying the vestibular area from the 34th to the 36th tooth (the 33rd tooth is missing). On palpation, the swelling has a hard consistency, is painless, expands the buccal cortical plate in the area of 34-36 teeth. Based on the history and clinical picture, a preliminary diagnosis of an odontogenic cyst was made, with the need for differential diagnosis with an odontogenic keratocyst. The panoramic radiograph showed four multilocular areas of radiolucency and one single-locular radiolucency with jagged edges. Areas of multilocular defects covered the body of the lower jaw, extending to the right and left to the ramus and left joint. The single-chamber area of clearing was located in the area of the tuberosity of the upper jaw on the left (photo 3). Fine needle aspiration biopsy of the swelling area was performed using a 24-gauge needle. The aspirated composition was creamy white in color with a protein concentration of 3.3 g/100 ml. Considering the possibility of Gorlin-Goltz syndrome, the patient also underwent chest radiography, computed tomography (CT), and lateral cephalography. A chest x-ray revealed cleft ribs 2, 3 and 4 on the right, and a similar pattern on the 3rd and 4th ribs on the left (Figure 4). A CT scan diagnosed a bilateral expanding lytic lesion of the mandible (photo 5), and a lateral cephalogram revealed overlap of the sella turcica (photo 6).
Photo 1. Extraoral examination revealed asymmetry, hypertelorism and strabismus.
Photo 2. Intraoral swelling in the buccal vestibule of the oral cavity.
Photo 3. The orthopantomogram revealed several multilocular radiolucencies with jagged edges.
Figure 4: Split ribs on chest x-ray.
Figure 5: Computed tomography revealed a bilateral expanding lytic lesion of the mandible.
Photo 6. On the lateral cephalogram, the overlap of the sella turcica is visualized.
After an incisive biopsy, histopathological examination of the sample revealed a cystic epithelium consisting of darkly stained basal cells arranged in a palisading pattern. The superficial layer revealed parakeratosis and a corrugated appearance, which could confirm the diagnosis of keratocyst (Figure 7).
Photo 7. Hyperchromatic palisade-like basal layer and corrugated parakeratotic surface (hematoxylin-eosin, × 10).
Discussion
Gorlin-Goltz syndrome occurs with equal frequency in both men and women of almost all ethnic groups. The disease is diagnosed in young patients, in most cases in people aged 17 to 35 years. This pathological condition is very difficult to diagnose in early childhood, since its symptoms appear gradually during growth, but a good prognosis for treatment is characteristic primarily for cases diagnosed in the early stages. The main and secondary symptoms of this pathology, summarized by Evans and colleagues in 1993, will help diagnose Gorlin-Goltz syndrome.
Main criteria:
- more than two basal cell carcinomas or one in patients younger than 20 years of age;
- odontogenic keratocysts of the jaws;
- three or more palmar or plantar recesses;
- bilayered areas of calcification of the falx cerebellum and cerebellum;
- splitting, fusion, or noticeable protrusion of ribs;
- direct relatives with inherent Gorlin-Goltz syndrome.
Secondary criteria:
- macrocephaly;
- congenital anomalies (cleft lip or palate, prominent frontal ridges, large face, moderate to severe hypertelorism);
- other skeletal anomalies (Sprengel deformities, extensive chest deformities, syndactyly of the fingers);
- X-ray abnormalities such as sella occlusion, spinal abnormalities, defects of the arms and legs, or fire-like lesions on the arms and legs;
- ovarian fibroma or myeloblastoma.
Two main criteria or one main and two minor ones are sufficient to make a diagnosis of Gorlin-Goltz syndrome. In our case, the diagnosis was confirmed by the presence of two main criteria (odontogenic keratoxitis of the jaws and cleft ribs) and two minor ones (congenital anomalies: prominent frontal tuberosities and hypertelorism; radiological abnormalities: kyphosis and sella turcica overlap).
Odontogenic keratocysts may be the first symptom of the syndrome. They are usually discovered incidentally on an x-ray. Cysts may appear clinically when infected as swelling. In our case, the diagnosed cysts were the first symptom of the later verified syndrome. Odontogenic keratocysts in Gorlin-Goltz syndrome usually present in the form of single-chamber or multi-chamber areas of radiolucency of the body, angle or ramus.
Various conservative approaches to the treatment of large cysts in young patients have been proposed, aimed at preserving soft and hard tissues, including teeth. These include techniques such as marsupialization, decompression, enucleation with Carnoy's solution, peripheral osteoectomy with or without Carnoy's solution, jaw resection, or surgical removal of the keratocyst followed by cryotherapy with Carnoy's solution. Genetic consultation is mandatory for all patients, since 50% of patients can transmit the disease to a child. Prenatal diagnosis during pregnancy can be carried out in cases of identified mutations in a family with a history of the syndrome.
In our case, the patient was referred to the Department of Oral and Maxillofacial Surgery, where he underwent enucleation and curettage of the cystic lesions (Figure 8). The patient was informed about the features of the syndrome with recommendations to avoid prolonged exposure to sunlight. Six months later, an x-ray revealed good progress in the healing of the cystic cavities with the formation of bone tissue. The patient is still under observation (Figure 9).
Photo 8. View after surgical enucleation of the cyst.
Photo 9. Visualization of the bone healing process 6 months after surgery.
conclusions
Patients with Gorlin-Goltz syndrome require a special multidisciplinary medical and dental approach during treatment. Early diagnosis ensures the prevention of complications and the selection of the correct treatment algorithm. Young patients without a history of basal cell carcinoma can simply take precautions and avoid radiation exposure. Diagnosed and treated patients should be closely monitored, as the recurrence rate of the syndrome reaches 63%.
Authors: S. Manjima, Zameera Naik, Vaishali Keluskar, Anjana Bagewadi
What is the prognosis for the disease?
How successfully the situation in a patient with an odontogenic cyst will be resolved depends on at what stage the cyst was discovered, how severe the symptoms were and how it was treated.
As a rule, the use of surgical treatment gives a positive prognosis. Therapeutic treatment provides a positive prognosis only if it is started at the initial stage of the disease.
A negative prognosis may be associated with detection of the disease at a late stage: odontogenic cysts can provoke the development of serious pathologies that cause deformation of the maxillofacial tissues.
What treatment methods for jaw cysts exist?
The choice of treatment method for an odontogenic cyst directly depends on the symptoms it causes, as well as the results obtained during instrumental and laboratory diagnostics.
If surgical treatment is chosen (cystotomy or cystectomy), the maxillofacial surgeon performs complete removal of the cyst. In some cases, it is necessary to remove the cyst along with the affected parts of the tooth root. Treatment is carried out in a hospital setting.
If the choice falls on therapeutic treatment, the doctor will carry out procedures aimed at reducing inflammation. This is a long process, taking at least six months.
The first step is to drain the contents of the cyst using a special drainage tube, which is inserted into a small incision in the tumor. As the contents drain out and the tumor shrinks, the size of the tube is adjusted downward.
After removing the contents of the cyst, the dentist cleans the root canals and administers medications that destroy the tumor tissue. At the end of all procedures, the doctor uses a special solution aimed at accelerating healing.
Treatment is monitored radiographically.
Both after surgical and therapeutic treatment, the patient requires preventive measures that will help avoid the re-formation of an odontogenic cyst.
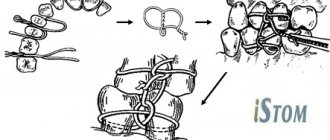
How is a dental cyst treated using cystotomy?
As noted earlier, before choosing a treatment method, the dental surgeon sends the patient for an x-ray. If, after studying the image, the surgeon chooses the cystotomy method, then local anesthesia is first performed. The anesthetic does not act immediately, so the dentist waits for some time (usually 5-10 minutes) and proceeds directly to surgical procedures.
If surgery is performed on the lower jaw with a very thin base, the jaw is preliminarily splinted to prevent a postoperative fracture.
The first thing that is done is an incision of the mucous membrane along with the periosteum. The incision is made with a surgical scalpel and has the shape of an arc. After the incision, the detachment of the mucoperiosteal flap begins. Detachment of the flap is done bluntly, using a special tool - a rasp. After detachment, the anterior wall of the jawbone opens, under which a cystic formation is located. There are clinical cases when, after detachment of the flap, the bone wall is either completely absent or thinned to such an extent that the pathological focus can be felt through it. This is due to the enormous size of the odontogenic cyst, which puts chronic stress on the bone, leading to its deformation.
If the bone wall is still preserved, it must be opened. This is done using a dental handpiece and a ball-shaped bur or cutter. The bone opens to the diameter that corresponds to the cystic formation. After opening, the anterior shell of the cyst opens, and it is this that is removed during cystotomy, all other shells are preserved. The tops of the dental roots that are in the cyst must be removed, i.e. Root resection and retrograde filling are performed.
After all the manipulations, the defect formed in the bone is covered with a mucoperiosteal flap and filled with gauze turunda soaked in Iodoform solution.