Patients with chronic periodontitis often encounter a situation where a cyst forms at the apex of the root - a cavity in the bone tissue filled with pus. Most often, a cyst develops due to infection in the root canals; sometimes the cause of a cyst is trauma, inflammatory processes in the periodontium (gums) and adjacent areas. It can also occur due to undetected caries, pulpitis or periodontitis, as well as due to poorly filled root canals.
Such a neoplasm may not bother a person for a long time. As a rule, a cyst makes itself felt during periods of weakened immunity, against the background of a cold. In such cases, the infectious process in the cyst cavity worsens, which leads to abundant pus formation. The patient feels acute pain, swelling and swelling of the gums appears, and a fever may appear. The main thing is to seek dental care on time. In these cases, resection of the apex of the tooth root and dental surgery to remove the cyst are used. However, you can often get by with therapeutic treatment.
Why does a dental cyst form?
The cause of cyst formation is an untreated root canal infection.
The reasons for infection in the root of a tooth can be different:
- As a complication of insufficiently treated or completely neglected
- caries/pulpitis,
- periodontitis,
- periodontal diseases,
- inflammation under the dental crown,
- Error and infection during endodontic treatment (root canal treatment).
- Tooth injury.
- Immune disorders in the body.
- Chronic diseases of the ENT organs: runny nose, sinusitis, tonsillitis.
Children in primary and mixed dentition can also suffer from dental cysts. Even newborns may experience teething with a purulent cyst - the so-called. Bona knots.
Quality criteria for dental cyst removal
Despite the fact that cystectomy is a surgical intervention, the main indicator of the quality of treatment will be the sanitation of the root canals, including retrograde filling. Currently, in addition to eliminating the cyst shell itself, the unspoken rule has become the filling of its cavity with one or another osteoplastic materials, because this completely eliminates the possibility of blood clot suppuration, promotes rapid healing of the bone defect and improves the mechanical stability of the tooth.
What are dental cysts?
Types of cysts
Root cyst
Develops from granuloma as a continuation of pulpal necrosis (death of pulp tissue) and as a result of periapical inflammation. It is located in the apical (apical) third of the tooth root and sometimes has a transverse orientation due to additional canals, the initial paths for the spread of pulpous necrosis.
Root cysts are radiolucent capsules with well-defined boundaries. They can vary greatly in size from 2-3 mm to 2-3 cm. In the absence of secondary inflammation, the roots develop asymptomatically. Even the largest neoplasms do not displace teeth or expand bone tissue.
Once diagnosed, treatment requires eliminating the underlying cause. The most common treatment for pulp necrosis is endodontic treatment. If it is unsuccessful, a decision is made on surgical curettage or enucleation.
Residual
Remains after removal of the pathology. It can form in the granuloma left after tooth extraction or around the left apex of the root.
The residual cyst is clearly visible on x-ray. Its dimensions range from a few millimeters to several centimeters.
Follicular cyst on the gum
A cyst in the gum develops from a follicular sac that encloses each unerupted tooth. This is a capsule clearly visible on an x-ray, most often surrounding the crown of an unerupted tooth. May cause extensive tooth damage. It has a rapid growth rate, can move to adjacent teeth and lead to expansion of the cortical plate.
Clinically, a follicular cyst always occurs in the area where the enamel meets the cementum of the tooth (the place of attachment of the follicle). Due to its growth, adjacent teeth may tilt, and in rare cases, resorption (destruction) of tooth roots occurs. Unerupted teeth can also become displaced due to aggressive growth. If a follicular neoplasm has been identified, its treatment may include surgical curettage (curettage).
Eruption cyst
This is a fluid-filled follicular sac that usually occurs during teething. It covers the erupting tooth and often contains blood. Outwardly it looks like pronounced swelling of soft tissues of a bluish color (due to the presence of blood). Most often it occurs due to slow tooth eruption and can rupture spontaneously. However, in some cases where it is found, treatment may include surgical resection to help the tooth erupt faster.
Primordial (keratocyst)
Develops from the tooth germ as a result of degeneration of the stellate reticulum during tooth development before the onset of calcification of its tissues. Keratocysts can arise from any developing tooth germ, but most often they are localized in the area of premolars and the third molar of the mandible.
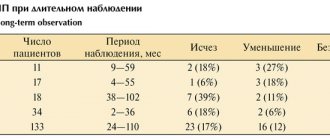
Clinically very prone to relapse. If the patient is diagnosed, treatment consists of careful curettage and close follow-up to ensure early detection of recurrence of pathology.
Lateral periodontal
The exact reasons for their occurrence are not fully known. They are rarely large. They are clearly visible on an x-ray and are most often closely associated with the lateral surface of the tooth root. Typically, teeth associated with these cysts have normal pulp. When a lateral periodontal neoplasm (cyst) is detected on the root of a tooth, treatment consists of surgical curettage without compromising the integrity of the tooth. It is important that the removed tissue is sent for histological analysis to rule out more serious pathologies such as early adamantinoma.
Calcifying odontogenic
Their etiology is also completely unknown. They can be found in any area of the supporting surface of the jaws, most often in the lower part. Morphologically they are quite diverse. Clearly visible on x-ray and may contain various opacities depending on the degree of calcification of the tumor. Once diagnosed, treatment consists of surgical curettage or resection.
Why do you need to remove the cyst?
If a dental cyst is not removed in time, even with an asymptomatic course of the disease, the consequences can be very serious - this is a real “time bomb”.
- The main danger of a cyst is that sooner or later it will destroy the affected tooth, and then “get” to the neighboring teeth.
- Cysts are reborn. Slowly but surely, so in 15-20 years it may already be a malignant formation.
- An infection is raging in the cavity of the cyst, so with a general illness, hypothermia, or a decrease in immunity as a result of simple stress, acute purulent inflammation is possible - flux, abscess, phlegmon.
- The infection can spread to adjacent lymph nodes and cause inflammation - lymphadenitis.
- Gradual thinning of the jaw bone in the affected area, due to purulent melting, turns into osteomyelitis. Even a spontaneous fracture of the jaw is possible.
- The cyst enlarges and can grow into the nasal cavity or maxillary sinus.
- Infection in the cyst can cause sepsis, a blood poisoning.
If treatment is not started on time, the tooth will have to be removed. And this is the minimum “evil”.
What are the symptoms of a dental cyst?
For a long time, the cyst may not manifest itself in any way until it becomes large enough in size, so it is very rare that a cyst is diagnosed at an early stage of the disease. This mostly occurs accidentally when the patient is having an x-ray for another reason.
At a later stage, the patient begins to worry about:
- Aching pain that gets worse over time. Such pain is difficult to relieve with regular painkillers.
- Pain when biting.
- Swelling of the gums and/or cheeks.
- An abscess, gumboil, or fistula may form on the gum.
- General malaise, fever.
Symptoms of anterior tooth cyst
This disease is especially dangerous due to its practically asymptomatic course at the initial stage - few people will worry if they notice a slight change in the color of the enamel or a slight displacement of the tooth. But a front tooth cyst is much more likely to be noticed than other types, since the frontal units have to “work” more often, because they are located only on one side of the jaw. However, other types of formations can go unnoticed for years, for example, if the patient is used to chewing on only one side. A cyst on the front upper or lower tooth is noticed much earlier, because pain is immediately felt.
Dangerous symptoms!
When the size of the granule with pus begins to exceed 10 mm, pronounced symptoms of a front tooth cyst arise:
- constant nagging pain with a feeling of fullness
- high fever and painful condition, which sometimes continue after the procedure for removing the cyst of the front tooth has already been completed
- swelling of the gingival tissue at the location of the granule, in severe pathologies it spreads to the face
- protrusion of a tubercle in the affected area
- enlarged lymph nodes - occurs if bacteria from the granule with pus begin to spread through the blood
How is a dental cyst treated?
The first thing that should be said is that today a dental cyst is successfully treated with a high percentage of preservation of the affected tooth, although in the past the diagnosis of a “cyst” meant 100% removal.
There are 2 main approaches to treatment:
- Therapeutic. Therapeutic treatment of dental cysts is used when
- There is access to the dental canal through the dental crown
- The canals are not sealed or can be opened
This method of treatment is very similar to the treatment of periodontitis, with the only difference being that the doctor additionally removes pus from the cyst cavity and injects special medicinal preparations into the root canal.
This treatment takes at least 1-2 visits, is carried out under sterile conditions, using a rubber dam and a dental microscope, because requires special care from the doctor to prevent relapses.
Treatment of cysts with laser with access through the coronal part of the tooth is another type of therapeutic treatment. Its main difference is that the laser immediately completely disinfects the area of the removed cyst, the treatment is quick and bloodless, the disadvantages include the risk of burns.
There are several methods for surgical removal of cysts, but cystectomy - complete removal of the cyst with all its contents - is the most modern and most effective of them.
Cystectomy is indicated for:
- A sealed root canal that is difficult to open.
- The affected tooth is replaced with a crown
- Pain, swelling of the cheeks/gums.
Many scientific and practical articles have been published about cysts of the maxillary sinuses. To date, there is no reliably established cause of cysts. They are often discovered by chance during examination of patients with headaches.
The main treatment method for maxillary sinus cysts is surgery. Various surgical approaches have been developed to remove cysts. But, unfortunately, we have to admit that in practice, the classic Caldwell-Luc method of maxillary sinus surgery is often used to remove paranasal sinus cysts.
It is worth noting that we are talking about rhinogenic sinus cysts, not odontogenic. Odontogenic cysts are an independent nosological form and their removal has its own characteristics.
There are false and true rhinogenic cysts. The difference lies in the presence of an epithelial lining in true cysts [1]. More often we deal with false cysts, which are considered as an accumulation of fluid under the epithelium of the sinus mucosa. The location of cysts varies greatly, but most often they are found on the lower wall of the maxillary sinus. The size of the cysts also varies.
If a cyst is detected, regardless of the reason for examining the patient, he should be carefully questioned and the condition of the intranasal structures examined. In these cases, many predisposing factors can be detected: the presence of allergies, a history of frequent respiratory diseases, constant disturbance of nasal breathing, etc.
During examination, you can most often see a curvature of the nasal septum and other disorders of the intranasal structures, which would require more than one page to list. If a cyst is detected on an X-ray or computer image, special attention should be paid to the condition of the nasal cavity.
The rhinogenic origin of most pathological processes in the paranasal sinuses is well proven and this should not be forgotten. Detected changes in the nasal cavity must be eliminated. Since such a patient usually gets used to certain symptoms or diseases, the data from endoscopy, computed tomography of the nasal cavity and paranasal sinuses should be adequately assessed, with an explanation of the prospects for the further development of the identified changes and their impact on the patient’s quality of life and health.
There are several surgical approaches for removing cysts, in particular the maxillary sinus. Considering the excessive trauma of radical surgery on the maxillary sinus, we will focus on modern endoscopic methods.
Such methods as microsinusrotomy and cyst removal through the middle nasal meatus are known [2, 3]. These methods have proven themselves well [4]. But with microsinusrotomy, 31.25% of patients experience dysfunction of the trigeminal nerve [4]. What if this cyst is small in size, located in the anteromedial corner of the maxillary sinus, and removing it through the middle nasal meatus poses a problem? There is a need to significantly expand the sinus anastomosis, and this is an unwanted injury. We understand quite well when to intervene using a minimally invasive method and when to intervene using a radical technique in the area of the ostiomeatal complex. We try to preserve the uncinate process. A method of balloon dilatation of the anastomosis has appeared, which makes it possible to minimally injure the structures of the ostiomeatal complex.
Microsinusrotomy can be used. Which trocar should I use? The point is not in the original version of the instrument, but in its shape and diameter.
Only an endoscope can be inserted through a standard trocar and the sinus can be examined, but removal must be done blindly if there is no special tool (Fig. 1). Special forceps have a working part with a controlled change in the angle of the working part (Fig. 2). These forceps are inserted into a standard trocar, the sinus cavity is examined through a 1.7 mm endoscope, and by changing the angle of the working part, the cyst shell is grasped and removed. The disadvantage of the tool is its rapid wear and high price.
Rice. 1. Trocar V.S. Kozlova. Rice. 2. Forceps combined with an endoscope for removing cysts.
A wide trocar in the form of an ear funnel makes it possible to visually remove the cyst, but the bone wall is more injured, and with it often the second branch of the trigeminal nerve. You can open the sinus through the front wall by making a hole with a bur. During microsinusrotomy with a trocar in the shape of an ear funnel, the bone structures of the anterior wall of the maxillary sinus break and penetrate into the sinus cavity. Therefore, a more gentle method is to open the front wall with a bur [4, 5].
The well-known access to the maxillary sinus through the lower nasal passage was left without due attention. It is well described in the classic manuals on intranasal surgery and in the book by F.S. Bokshtein [6]. But this method also has its own characteristics. We are talking about injury to the nasolacrimal duct during puncture of the maxillary sinus, and when opening the sinus through the lower nasal passage, the likelihood of injury to the nasolacrimal duct is more likely. So what to choose, what approach?
As always, the question of approach is decided individually. In this work, I express my opinion in favor of the surgical approach, guided by the following considerations.
First of all, should there be an operation or not? If the patient has recently suffered acute rhinitis of various etiologies and slight swelling of the mucous membrane and the presence of a small cyst are found in the sinus, there is no need to rush into surgery. All these changes may disappear. Headache should be considered an indication for surgery in the presence of a cyst. A larger cyst can often cause discomfort and facial pain. Any headache in the presence of a cyst of any size in the sinus dictates the need for its removal.
Let's consider three options. If a large cyst is present, a thorough examination of the nasal cavity through an endoscope is necessary (Fig. 3). During the operation, detected violations of the intranasal structures are eliminated. The necessary correction of the septum and nasal turbinates is performed. The structures of the ostiomeatal complex of the affected side are examined. If there is a block, it must be eliminated with the minimum possible resection of the uncinate process. Resection is performed with a reverse bite in the lower part of the process. The anastomosis with the sinus is restored. An inspection is being carried out. A large cyst is clearly visualized, grasped with forceps and removed (Fig. 4).
Rice. 3. 4mm 45 degree endoscope. Middle nasal passage. Large diameter maxillary sinus cyst. Rice. 4. 4mm 45 degree endoscope. Large diameter maxillary sinus cyst. Removing the cyst using Blakesley forceps.
As a rule, only part of the shell can be removed at first. Fluid pours out of the cyst, its shell shrinks. Using suction, the membrane is drawn to the anastomosis and its remainder is removed. The sinus is examined through a 45-degree endoscope or through an endoscope with a variable angle of view from 30 to 90 degrees. The remainder of the membrane can be removed using Binner forceps (Fig. 5). On the second day after surgery, the sinus is washed with saline, and the patient can be released for outpatient observation.
Rice. 5. Binner forceps.
If the cyst is small in size in the zygomatic recess or on the lateral wall of the sinus, it is more convenient to remove it using the microsinusrotomy method. A standard trocar causes minor surgical trauma, but, as already noted, only an endoscope can be passed through it. You can aim the trocar tube at the cyst, bring the shaver to it and remove the membrane. Then check the result. This procedure can be quite successful, but removal occurs without visual control. A small hole made with a bur in the anterior wall of the maxillary sinus after a small incision in the mucous membrane makes it possible to visually remove the cyst located at the bottom of the sinus cavity and in the zygomatic recess.
Trocars in the shape of an ear funnel allow removal of the cyst under visual control, but the trauma to the soft tissue and bone wall that occurs in this case is significantly greater. When approaching through the anterior wall, the branches of the trigeminal nerve are always injured, which, at best, is accompanied by a short-term decrease in the sensitivity of the upper lip. In rare cases, serious trigeminal neuralgia occurs.
The approach through the lower nasal meatus is indicated when the cyst is localized in the anteromedial corner of the sinus. Such a cyst can be removed through the middle nasal passage only with a significant expansion of the anastomosis and the use of endoscopes with variable viewing angles. The approach through the lower nasal meatus eliminates injury to the branches of the trigeminal nerve and is performed as follows.
Using a nasal speculum or raspator, the inferior nasal concha is shifted medially, opening the inferior nasal passage (Fig. 6). A grooved chisel 5-6 mm wide is installed on the lateral wall of the lower nasal meatus behind the edge of the pyriform opening. It is necessary to carefully study the computer image and determine the thickness of the bone of the edge of the piriform foramen, since by placing the chisel too anteriorly, the surgeon may penetrate the soft tissue of the cheek, which is unacceptable. It is necessary to take into account the height of the bottom of the maxillary sinus. The chisel is pressed at the level of the bottom of the nasal cavity below the puncture point of the maxillary sinus. With a light blow, the chisel pierces the lateral wall of the lower nasal meatus, which is displaced in the medial direction by the same chisel. An overview of the bottom and lateral wall of the sinus opens (Fig. 7). A sufficiently wide opening is created for visual removal of a cyst or foreign body or polypous tissue. You can work as a shaver. Through this approach, the entire sinus can be clearly examined using variable-angle optics (Fig. 8).
Rice. 6. The lower sink is shifted towards the partition. The lower nasal passage is open. Rice. 7. An approach to the sinus has been created. Rice. 8. Endoscopy of the left maxillary sinus. A 4-mm 45-degree endoscope is inserted into the maxillary sinus through an opening in the lateral wall of the inferior nasal meatus. A cyst is visible in the anteromedial corner of the maxillary sinus.
Then the lateral wall of the lower nasal meatus is shifted laterally to its original location. As a rule, the edges of the mucous membrane touch. The lower sink is also installed in its original place. It is imperative to monitor the condition of the ostiomeatal complex. If there is a block of it, it needs to be eliminated. The natural anastomosis can be expanded with a spoon to open the frontal sinus using the type of balloon dilatation. Every other day, the sinus should be rinsed. Rinsing can be done through the lower nasal passage by inserting a needle through the surgical approach site or through the middle nasal passage.
The issue of nasal tamponade is decided individually, but, as a rule, it is not required for all of the above methods. The patient can be released for outpatient observation the next day after surgery.
How is surgery to remove a cyst (cystectomy) performed?
Removal of the cyst is carried out by a dental surgeon in a surgical office, on an outpatient basis, the operation usually lasts about half an hour, an hour after the manipulation the patient can go home. Improvement in the patient's condition should occur 6-8 hours after the operation. A sick leave certificate is issued for the recovery period - until the stitches are removed.
To relieve all pain, the patient is given local conduction or infiltration anesthesia; we also numb the injection site with an application gel. After surgery, painkillers in tablets are prescribed for the first time.
I Preparatory stage
- The patient is diagnosed by a surgeon, and a consultation with the attending dentist-therapist is required.
- It is advisable, if the operation is not urgent, to provide the patient with professional hygiene and sanitation of the oral cavity before surgery - this reduces the presence of infection in the oral cavity and healing proceeds faster.
II Carrying out the operation
- The patient is given anesthesia.
- The surgical field is treated with an antiseptic.
- The dentist-surgeon separates the mucoperiosteal flap from the bone.
- Access to the affected area is provided, the cyst along with the affected part of the apex of the tooth is removed.
- The cavity is thoroughly cleaned and washed with an antiseptic.
- An antiseptic is injected into the cavity and the wound is sutured.
- During the recovery process, the cavity heals on its own and the bone tissue is restored.
III Postoperative period
- After the operation, you should not eat for 4 hours, then the food should not be hot, liquid and gentle.
- The patient is prescribed antibiotics to fight the infection and painkillers.
- Hygiene can be carried out according to the standard scheme one day after surgery, according to the recommendations of your doctor.
- Antiseptic rinses and healing gels are prescribed.
- Swelling of the gums and face may occur for several days.
- NOT RECOMMENDED:
- Warm the surgical site, because re-development of the infection is possible.
- Take medications without a doctor's prescription.
How is tooth root apex resection and cyst removal performed?
Typically, the entire procedure takes about an hour. In this case, the position of the tooth is important: surgery on distant teeth requires more skill and time.
During the operation, which is performed under local anesthesia, an incision is made in the gum near the diseased tooth to peel it away to expose the bone tissue. A small hole is then made in the bone using a special bur. Through it, the doctor should see the apex of the tooth root and the cyst attached to it.
Using a drill, the tip of the root is cut off and then removed from the wound along with the cyst attached to it. After the cyst is removed, synthetic bone is placed into the empty space to restore jaw bone tissue. At the end of the procedure, the mucous membrane of the gums at the incision site is sutured, sometimes a drainage is inserted between the sutures to drain the ichor from the operation site for several days.
When performing a tooth resection, only the inflamed and infected part of the root is removed, healthy tissue is not affected.
Prevention of dental cysts
Taking standard care of your dental and general health will help prevent the development of cysts.
To prevent dental cysts from bothering you, you must:
- Undergo regular preventive examinations with your dentist every 6 months and a professional hygiene procedure. Do not refuse if the doctor offers you an X-ray examination - he has reasons for this.
- Treat caries and pulpitis in a timely manner.
- To identify hidden caries at an early stage of the disease, for this in our clinic we use digital (not x-ray) diagnostics using the Diagnocam apparatus. We recommend undergoing such diagnostics at least once every six months.
- Brush your teeth well yourself using dental floss, irrigator, and mouthwash. Pay attention to cleaning your tongue.
- Strengthen immunity.