Warts on the hands are a benign viral disease in which single or multiple rounded protruding papules of various sizes appear on the skin - from 1 mm to 1.5 cm (sometimes more), gray or flesh-colored. In addition to the skin of the hands, warts can appear on other parts of the body (face, anogenital area, soles of the feet, etc.), as well as on mucous membranes.
The formations tend to spread, merge into large conglomerates, rapidly grow, bleed when injured, and relapse. Self-treatment using questionable methods leads to the appearance of scars, and malignant degeneration is possible on the mucous membranes. Therefore, the problem cannot be ignored.
Sometimes warts can disappear without treatment within 2 years. However, you should not rely on this, since the pathogen still remains in the body and, against the background of a weakened immune system, the formations will make themselves felt again. And over time, they may become less sensitive to therapeutic effects. Therefore, it is important to remove them and, in some cases, undergo antiviral therapy and immunocorrection.
Why do they appear?
Like warts, papillomas are not dangerous
.
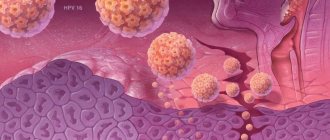
Their appearance is associated with the human papillomavirus (HPV),
which is transmitted through contact with a carrier. It is also possible to transmit HPV from an affected area of skin to a healthy one in one person. High humidity and microcracks in the skin increase susceptibility to viral particles. In this regard, you should always use personal hygiene items when visiting swimming pools, saunas and showers.
Important:
a large number of papillomas may indicate problems with the immune system.
For women in such cases, it is necessary to take a smear for HPV, since some of its types can cause cervical cancer
Depending on the clinical picture, they are usually divided into 3 types:
Benign
(atheroma, hemangioma, lymphangioma, lipoma, papilloma, mole, nevus, fibroma, neurofibroma)
They do not pose a threat to human life, but if poorly placed or large in size, they can cause disturbances in the functioning of other systems and/or organs of our body. Under external influences they can sometimes transform into malignant neoplasms.
Malignant
(basal cell carcinoma, melanoma, sarcoma, liposarcoma)
They grow quickly and aggressively, penetrating into surrounding tissues and organs, often with the formation of metastases. The prognosis of such diseases is often unfavorable, given the difficulty of curing them and the tendency for frequent relapses, and in some cases, active metastasis leads to death if vital organs are irreversibly damaged.
Borderline or precancerous skin conditions
(senile keratoma, xeroderma pigmentosum, cutaneous horn, Bowen's dermatosis)
Formations, the tissues of which, under the influence of hereditary or current causes, have changed, having the potential to degenerate into malignant tumors.
What is the best way to treat?
A large number of papillomas certainly causes inconvenience and does not look aesthetically pleasing. However, this is not a reason to use old-fashioned methods for removal with thread, pliers or a blowtorch.
For single small (1x1 mm) formations, celandine juice
- a proven folk remedy.
When there are many papillomas or they are large, this method is not suitable
, as it can last for months and lead to severe inflammation.
Removal using radio wave surgery is much more convenient and effective
The operation does not require special preparation, is practically painless, and after it you can drive a car.
Once I had the opportunity to remove about 70 papillomas from one patient at once. It is difficult to convey all the joy of a person who got rid of them, whom they tormented for several years.
What are skin tags?
the skin growth is acrochordon, which means a small benign tumor that appears on the skin in folds or in places of excessive friction (neck-collar area, groin).
Figure 3. Skin tags are benign skin tumors
In Russian literature, such skin growths are also called soft fibromas. The size of skin growths can vary widely from barely noticeable protrusions to hanging skin formations of 2-5 mm or more.
Treatment results
The photo below shows the results of removal of neck papillomas using radio wave surgery
Rarely occur again. Reappearance of papillomas is possible with high virus activity in the body. In this situation, additional treatment with immunomodulators or consultation with an immunologist may be required.
Methods for removing skin tags
There are several known ways to remove skin growths:
- Simple cutting with scissors or a scalpel;
- Removal with radio knife;
- Removal with a coagulator;
- Removal with liquid nitrogen;
- Laser removal;
- Plasma removal.
Rice. 5A. Stages of removing skin growths with a laser. Anesthesia
Rice. 5 B. Stages of removing skin growths with a laser. Laser vaporization
Rice. 5V. Stages of removing skin growths with a laser. Laser vaporization.
Rice. 5G. Stages of removing skin growths with a laser. Laser vaporization
Rice. 5D. Stages of removing skin growths with a laser. Final result
Each of them has the right to exist. However, since skin growths in most cases are removed solely for cosmetic reasons, removal methods should be chosen that will not subsequently leave a visible mark on the skin. These methods include: laser and plasma vaporization.
Diagnosis of fibroids of the upper and lower jaw
The doctor will not prescribe treatment until he is sure that the diagnosis is correct. To do this, diagnostic procedures are carried out, the results of which will confirm or refute the fears of doctors.
First, the patient is asked to describe the symptoms. The dentist examines and palpates the tumor. However, this is not enough to develop therapeutic tactics, since it is extremely important to determine the depth of tumor growth into soft tissue. For this purpose, an ultrasound examination is performed.
In difficult cases (ulcers, development of an inflammatory process in a pathological area of the gum, etc.), a biopsy is indicated. After surgical removal of the tumor, fragments are necessarily sent for histological analysis.
The examination is necessary not only to establish a diagnosis, but also to identify the factors that provoked the disease. A full dental examination is carried out to confirm the presence of inflammation. In addition, one cannot do without radiography, orthopantomogram and other images in different projections.
If a person has dentures, a consultation with an orthopedic dentist may be necessary. This is necessary to eliminate the possible traumatic effects of artificial elements on the mucous membranes.
Differential diagnosis
Biopsy remains one of the most informative methods for distinguishing fibroids from other benign neoplasms. The study is indicated for suspected papilloma, lipoma, epulis of various structures, neurofibroma, cyst, squamous cell carcinoma, wart, etc.
If the growth is localized on the tongue or sublingual part, it is extremely important to differentiate it from all existing seals. Timely diagnostic measures make it possible to detect cancer at the earliest stages and provide high-quality therapy with a short recovery period.
Symptoms
The tumor grows and develops quite slowly, so for a long time the patient may not even be aware of its presence in the mouth. Fibroma of the oral mucosa looks like a hemispherical growth rising above the plane, covered with pinkish tissue. If you press it, pain or other discomfort does not appear. The surface is smooth, there are no irregularities or roughness on it.
The appearance of ulcers with such a diagnosis is very rare. In such cases, an infection is usually associated with the subsequent development of the inflammatory process. Swelling, redness, erosion occur, and pain is felt. The pain persists even if you do not touch the pathological area.
If you do not injure the formation, it may not change its size for quite a long time and remain in a stable state. If it is exposed to constant traumatic effects, there is a high risk of malignant degeneration, which is dangerous to the life and health of the patient.
Treatment of oral fibroids
Surgery remains the most effective and most common therapeutic method. The seal is excised using a laser or radio waves. This procedure lasts about half an hour. If the tumor is very large, after its removal the wound is covered with a flap, which is formed by the doctor from the surrounding tissue.
When pathology is caused by taking certain medications, they should be completely eliminated and replaced with alternatives with similar properties. After discontinuation of drugs in such cases, the appearance of the mucous membranes is often restored without outside help, and the likelihood of relapse approaches zero. However, this does not apply to situations where the disease is advanced.
Surgery can also be avoided in case of traumatic effects of orthopedic structures. For example, when a crown, filling, or prosthesis puts pressure on the tissue. Elimination of the provoking factor often leads to a decrease or complete disappearance of a benign formation. Most likely, it will be necessary to dismantle the old structures and replace them with new ones.
On the Internet you can find stories of healing using home remedies. It is worth remembering that the disease cannot be treated with the help of folk recipes. Herbal decoctions and infusions, and other compositions are used only as an auxiliary element of complex therapy.
Chalazion
Cones of this type are quite common. They develop from a sebaceous gland whose duct is blocked. This formation is also called a “grading lump” or “cold barley.” The continued production of sebaceous gland secretion leads to the accumulation of a viscous mass in the capsule, which stretches and thickens, taking the form of a dense lump. On palpation, the contents under the skin feel like a moving ball.
Cold barley develops at a slow pace, so it does not cause pain. Only a formed hard capsule can cause pain when squeezed. If a chalazion is not treated, it can develop into a cyst. As the lump develops, the risk of complications increases: inflammation, formation of a purulent fistula, granulation.
Video from our specialist about the disease and its treatment
There are cases where chalazion spontaneously resolved without medical intervention. However, most often this formation does not develop back and requires prompt and conservative help. Treatment for such a lump on the eyelid is prescribed by an ophthalmologist. If the chalazion is small and not old, you can limit yourself to UHF therapy, ointments and eye drops. More severe cases are treated by injecting corticosteroids into the capsule cavity. Local drugs (ofloxacin, dexamethasone, sodium sulfacyl, hadrocortisone, levofloxacin, tetracycline ointment) can also be used as an addition to the injection.
If drug therapy is ineffective, the doctor decides on surgical treatment. The operation to remove a chalazion is performed under local anesthesia and lasts no longer than 15 minutes.
Barley
Styes are more common than chalazions. This type of lump on the lower or upper eyelid is caused by inflammation of the follicle (bulb) of the eyelash. This also clogs the sebaceous gland duct. Styes develop over several days or even hours and can occur in both adults and children. More often, the systematic appearance of barley is observed in people with weakened immune systems or who have changed their place of residence to an area with a more severe climate, as well as in people exposed to constant stress factors.
Based on their origin, there are two types of barley. Inflammation can be external (when the sebaceous gland suppurates) and internal (when the source of inflammation is located in the membolic gland).
The development of external styes is characterized by subjective sensations similar to a foreign body entering the eye. The initial stage may also be accompanied by stabbing pain. External stye visually manifests itself as redness and swelling of the eyelid. The internal one is usually not so noticeable, but it causes even more discomfort and pain.
Without treatment, barley develops within a few days into an abscess, which opens with the release of purulent contents. This brings relief, but an open wound is dangerous due to the possibility of re-infection.
It is better to start treating barley without waiting for the abscess to spontaneously break through. This allows you to get rid of the painful lump faster and with less risk of complications. If you still don’t have the courage or time to visit an ophthalmologist, you should remember that prolonged suppuration of the eyelid is very dangerous. If the stye does not open for more than two weeks, surgical treatment is necessary. An ophthalmic surgeon will remove the abscess under local anesthesia and give recommendations for further treatment of the eyelid. Most often, therapy for developing or already opened barley includes drops and ointments that contain antibiotics (albucid, gentamicin, erythromycin, tetracycline ointment).