The most common form of gingivitis is catarrhal gingivitis, which affects the gums, causing superficial inflammation. Most often, this disease affects children and young people under 35 years of age. In older patients, as a rule, chronic catarrhal gingivitis is diagnosed.
Teeth polishing with pastes - 1,200 rubles.
Polishing one tooth with paste - 50 rubles.
Coating with a fluoride-containing product (1 row of teeth) - RUB 1,500.
Coating with fluorine-containing varnish (1 tooth) - 250 rubles.
Retraction of hypertrophied gums in the area of 1 tooth - 600 rubles.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Causes of gingivitis
Gingivitis does not always progress as a separate disease. It often appears in the background:
- Imbalance in the hormonal system.
- Disturbances in the gastrointestinal tract.
- Diseases of the cardiovascular system.
- Infections and inflammatory processes.
Internal factors in the development of pathology are as follows:
- Fall of immunity.
- Growth of wisdom teeth.
- Lack of vitamins P and C.
- Allergy.
- Diabetes.
- Metabolic disorders.
- Chronic gastrointestinal diseases.
- Severe mental disorders.
Among the external causes of gingivitis:
- Smoking or improper breathing.
- Burns and mechanical damage to the mucous membrane.
- Incorrect installation of the seal.
- Irregular brushing of teeth.
- Infections.
In more than 50% of cases, the development of pathology occurs due to pathogens that penetrate the oral cavity with food and liquid. If you brush your teeth incorrectly and irregularly and do not use floss, a thick plaque will appear. Often inflammation begins due to a burn or mechanical damage to the gums. A lack of nutrients in the diet and serious stress can reduce immunity, which will also lead to the development of pathology.
Case history: Chronic localized catarrhal gingivitis
Passport part
1. Full name — Vasiliev Ivan Alexandrovich
2. Date of birth - 04/13/61
3. Profession - honey. entrepreneur
4. Home address - Skobelevskaya str., no.3. bldg. 1 kv. 39
Complaints upon admission
Reception date: November 11, 2004. The patient complains of bleeding gums while eating and brushing teeth with pink discoloration of the oral fluid, and an aesthetic defect: pigmented dental plaque.
Life history (Anamnesis vitae)
1. Previous diseases - chicken pox.
2. Concomitant diseases - no
3. Denies the presence of tuberculosis, hepatitis and AIDS. There are no chronic diseases.
4. Drug intolerance - no history of allergies
5. Occupational history - no occupational hazards or diseases
6. Bad habits - denies the use of alcohol, tobacco, and drugs.
7. Living conditions: lives in a 2-room apartment with his wife and 2 children. The family environment is good. I did not work in hazardous industries.
History of the development of this disease (Anamnesis morbi)
When collecting anamnesis, it was established that 2 years ago he noticed bleeding gums when brushing his teeth.
The present condition of the patient (Status praesens)
1.- General condition of the patient The general condition is satisfactory. The skin is pale pink, normally moisturized, elastic. No dryness, rash, scratching, hemorrhages, peeling or ulcers were detected on the skin.
2. External examination of the maxillofacial area. The configuration of the face is not changed, the skin is pale pink and normally moisturized. There are no skin rashes or swelling. The red border of the lips is without pathological changes; lips are normally moisturized; There is no dryness, crusts, cracks, erosions or ulcerations. Regional lymph nodes (submandibular, mental, cervical) are not enlarged, not fused with surrounding tissues, and painless on palpation.
3. Examination of the oral cavity. The mucous membrane of the lips, cheeks, hard and soft palate is pale pink, moderately moisturized, without pathological changes; no swelling is observed. .The tongue is of normal size, the mucous membrane is pale pink, moderately moist. The dorsum of the tongue is clean, there are no desquamations, cracks or ulcers. There is a slight overlap. Soreness, burning, and tongue are not observed. The palatine tonsils are not enlarged, there are no purulent plugs in the lacunae, and there is no plaque.
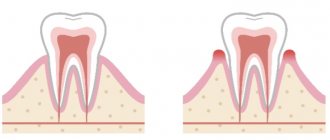
4. Examination of the gums. The marginal part of the gums and interdental papillae are swollen and slightly hyperemic. Bleeding is observed from the top of the papillae when pressing at their base and probing. The dentogingival junction is not broken. There are no pathological periodontal pockets.
5. Dental examination Dental formula: Orthognathic bite. All teeth up to the equator of the crowns are covered with a dark brown coating from strong tea. Soft plaque of a light brown color is localized in the cervical area of all teeth. There is supragingival tartar of brown color, dense consistency and subgingival tartar on all teeth. The depth of the vestibule is normal. No anomalies in the position and shape of the teeth were identified. There are no non-carious lesions on the teeth.
Additional research methods
Symptoms of catarrhal gingivitis
The sooner treatment for acute catarrhal gingivitis begins, the lower the risk of subsequent complications. Symptoms that should promptly contact your dentist include the following:
- bleeding, redness and swelling of the gums;
- itching in the gums;
- increased body temperature;
- bad breath, unpleasant taste;
- pain in the gums when eating or pressing on them;
- general malaise, fatigue.
Indications
You need to immediately begin treatment for catarrhal gingivitis if you find:
- Swelling of the gums.
- Bleeding after eating or brushing teeth.
- Acute pain and burning in the gum area.
- Bad breath.
- Putrid or bloody taste in the mouth.
- Changes in gum color and density.
Contraindications
It is not recommended to start treatment if you have:
- Psychological and nervous diseases.
- Cardiovascular pathologies.
- Problems with blood clotting.
- Chronic diseases in the acute stage.
- Allergic reactions to anesthesia.
A specialist will give you a full list of contraindications during a face-to-face consultation.
History of the disease
When collecting anamnesis, it was established that gums have been bleeding when brushing teeth or biting off hard food for several years; the patient does not observe individual oral hygiene (brushing teeth once a day). According to the patient, the last time he visited the dentist was 2 years ago. The patient himself associates severe pain in the gums with a recent flu.
Previous and concomitant diseases
Allergological anamnesis is not burdened. The patient denies the presence of hepatitis, HIV, herpes virus, cardiovascular diseases, disorders of the nervous system, digestive and respiratory systems. As a child, he suffered from acute respiratory diseases. 2 weeks ago I had the flu.
Bad habits - smoking.
Forms of catarrhal gingivitis
Depending on the nature of the lesion, there are:
- acute catarrhal gingivitis - characterized by rapid development and one-time inflammation, limited in time;
- chronic catarrhal gingivitis is a continuation of acute; in the absence of treatment, it is practically asymptomatic, but with regular exacerbations.
The scale of inflammatory processes determines two forms of gingivitis:
- localized - part of the gum is inflamed, no more than 1 - 3 teeth;
- generalized - the entire gum on one or both jaws is inflamed.
The severity of the disease is as follows:
- mild - the periodontal papillae are affected;
- medium - the free area of the gums is affected;
- severe - the alveolar region of the gum is affected.
Gingivitis
Regardless of the clinical and morphological form, characteristic differential diagnostic signs are distinguished:
- the disease is detected mainly in children and young people;
- the presence of non-mineralized dental deposits (microbial plaque, soft plaque, food debris) and tartar;
- direct relationship between the hygiene index and inflammation index;
- a frequent combination of gingivitis with focal demineralization - caries at the spot stage in the cervical area;
- the presence of certain clinical and morphological manifestations of inflammation in the gum and its deformation: with catarrhal gingivitis due to edema (acute and exacerbation of chronic) and inflammatory infiltration; with ulcerative - due to alteration and necrosis; with proliferative - as a result of proliferation;
- bleeding upon slight probing of the gingival sulcus;
- absence of a gum pocket;
- lack of clear changes in the interdental septa;
- absence of signs of destruction on the radiograph;
- the general condition of the patients is not impaired.
In acute or exacerbation of chronic catarrhal and ulcerative gingivitis, depending on the severity and extent of the process, differently expressed intoxication is observed.
The severity of gingivitis is determined by the totality of general changes in the body and the degree of involvement of the gums in the pathological process.
Catarrhal gingivitis occurs mainly in the form of chronic gingivitis or its exacerbation. Acute catarrhal gingivitis is usually a symptom of an acute respiratory infection.
Clinical manifestations of catarrhal gingivitis are caused by morphological changes in the epithelium and underlying connective tissue. In the epithelium, areas of desquamation, edema, signs of parakeratosis and acanthosis are detected, the level of acid glycosaminoglycans and glycogen is increased. In the spinous layer of the epithelium, the amount of protein is reduced and the RNA content is sharply reduced; in the connective tissue there is chronic inflammation: edema, hyperemia, stasis, accumulation of lymphocytes and plasma cells.
There is pronounced cellular infiltration of the gums. Initially, infiltrates in the stroma are focal in nature, located predominantly perivascularly, and consist mainly of lymphocytes and macrophages. As inflammation progresses, the composition of the infiltrate changes, and plasma cells and mast cells begin to predominate. Newly formed vessels and fibroblasts appear, and collagen formation is noted.
With exacerbation of chronic gingivitis, leukocyte infiltration increases. The phenomena of phlebectasia and reduction of the capillary bed are observed. The phenomena of edema are more often found in the area of epithelial attachment and subepithelial, absent in the deep parts of the stroma.
Reflection of pronounced vascular-stromal disorders are dystrophic changes in the epithelium (vacuolar, balloon dystrophy), and the phenomenon of acanthosis.
The results of a histoenzymatic study of the gums indicate significant metabolic disorders in the form of increased permeability of capillary vessels, decreased activity of aerobic oxidation processes and increased glycolysis in epithelial and stromal cells.
Thus, with catarrhal gingivitis, a picture of chronic nonspecific inflammation and exacerbation phenomena are observed. There are biochemical changes in the structure of the main substance, indicating a decrease in the activity of redox enzymes.
The epithelial attachment is not disrupted.
The clinical picture of catarrhal gingivitis largely depends on its severity, associated with the degree of involvement of the gums in the pathological process.
Mild gingivitis is characterized by damage to the gingival papillae; moderate severity - gingival papillae and marginal (marginal) gums; for severe - damage to the entire gum.
With chronic catarrhal gingivitis , patients do not go to the doctor, since there is usually no pain in the gums, but periodically there is a feeling of discomfort in the gums, bad breath, and bleeding gums when brushing teeth and eating. The interdental gingival papillae may acquire a bluish color, and the marginal gum may acquire a roll-like shape while the attached gum remains unchanged. During an exacerbation, patients complain of increased bleeding of the gums when brushing their teeth and eating hard food, a burning sensation, and swelling in the gums; the general condition is not disturbed. During the examination, hyperemia and swelling of the gums and a smoothed contour of the gingival margin are detected.
With exacerbation of chronic generalized catarrhal gingivitis, mild intoxication (malaise, weakness, palpitations, low-grade fever) is sometimes observed. This is usually associated with an exacerbation of a general disease, which is often the cause of exacerbation of gum disease.
Chronic hypertrophic gingivitis is a chronic inflammatory process of gum tissue with a predominance of proliferation processes. According to clinical and morphological characteristics, edematous and fibrous forms are distinguished; the edematous form is more common. Hypertrophic gingivitis is usually preceded by catarrhal inflammation, which can be combined with catarrhal gingivitis and does not have an acute course. Favorite localization is the area of the front teeth of the upper and lower jaws.
Morphologically, the edematous form of hypertrophic gingivitis , in addition to swelling of the epithelium and the underlying substance of the connective tissue and an increase in the level of acidic glycosamonoglycans, is characterized by dilation and proliferation of capillaries, which creates an increase in gingival mass. Abundant and varied cellular infiltration is observed (leukocytes, plasma and mast cells, lymphocytes).
With the edematous form of hypertrophic gingivitis, patients, in addition to complaints of bleeding gums when eating or brushing their teeth, complain of an aesthetic defect associated with an increase in the volume of the gums. Hypertrophic gingivitis, in which gum hypertrophy does not exceed the length of the tooth crown, is called mild; with more pronounced deformation of the gums - up to At the crown of the tooth - moderate severity; if the gum covers the entire crown of the tooth, this is severe hypertrophic gingivitis.
Objectively, the edematous form of hypertrophic gingivitis is characterized by enlarged gums, a glossy bluish surface, bleeding when probing the periodontal sulcus, sometimes when touched, and the formation of false periodontal pockets. The epithelial attachment is not broken. Dental and subgingival dental deposits may be detected.
The fibrous form of hypertrophic gingivitis is morphologically manifested by keratinization of the epithelium like parakeratosis, its thickening and proliferation into the depths of the connective tissue. In the stroma there is proliferation of fibroblasts and collagen structures, thickening of vessel walls, rare foci of inflammatory infiltration. The epithelial attachment is not broken. At first, this form of gingivitis usually does not bother patients. As the process develops (moderate and severe), patients notice gum growth and cosmetic defects. Objectively, deformation of the gums is detected, which is pale pink in color, dense, with a bumpy surface. There is no bleeding, false periodontal pockets, supragingival and subgingival dental deposits are identified.
Ulcerative gingivitis is a destructive form of inflammation of the gums, in the etiopathogenesis of which a significant role is played by a change in the reactivity of the body and, consequently, a decrease in the resistance of the gums to autoinfection of the oral cavity (especially to gram-negative bacteria, fusospirochetes).
This condition may be preceded by an acute respiratory disease, stressful situations, or hypothermia. Ulcerative gingivitis most often occurs in young people during or after general illnesses (flu, acute respiratory infections, tonsillitis), malnutrition (especially vitamin deficiency), poisoning with toxic substances, heavy metal salts due to radiation. Stress can be of great importance in the development of this pathology, since it causes a blockade of the mononuclear macrophage system and stimulates the production of glucocorticoids. Provoking factors may be poor oral hygiene, the presence of multiple caries cavities and dental plaque, and difficult eruption of third molars (wisdom teeth).
Morphologically, acute necrotizing ulcerative gingivitis is characterized by ulceration of the gum epithelium, swelling and destruction of collagen fibers, pronounced leukemia, lymph and plasmacytic infiltration.
Ulcerative gingivitis usually begins acutely: pain and bleeding gums, difficulty eating, general malaise, putrid breath, increased body temperature. Upon examination, the gums have a grayish color, the gingival papillae are necrotic, and there is an abundance of soft plaque. The gums of the upper and lower jaws are affected; rarely the disease is localized on one jaw.
The severity of ulcerative gingivitis is determined not only by the degree of gum damage, but also by the severity of general intoxication: increased body temperature, changes in peripheral blood: leukocytosis, increased ESR, shift to the left; Regional lymph nodes may enlarge and become painful.
When diagnosing ulcerative gingivitis, it is necessary to exclude blood diseases (leukemia, agranulocytosis), which are also characterized by necrotic ulcerative lesions of the gums.
Mild ulcerative gingivitis, like catarrhal gingivitis, is a reversible process. In case of moderate and severe ulcerative gingivitis, defects of the connective epithelium and post-necrotic defects of the gums are irreversible: violations of the gingival contour are possible (the apices of the gingival papillae are cut off) and exposure of the necks of the teeth.
Diagnosis of the disease
Diagnosis of catarrhal gingivitis involves examination by a doctor and laboratory tests.
The latter allow you to determine indicators such as:
- bleeding gums;
- degree of inflammation;
- amount of microbial plaque.
When conducting an examination, the dentist pays special attention to the following factors:
- how full the blood vessels of the gums are;
- red gums;
- integrity of the periodontal junction;
- the presence and amount of plaque and tartar;
- presence of signs of destruction of the interalveolar septa.
Catarrhal stages
For this form there are stages:
- acute - characterized by the rapid onset and development of the disease, significant bleeding and pain, bright red color of the mucous membranes near the tooth root;
- chronic - the color acquires a bluish tint, symptoms appear slowly, and there is no pain during brushing, and exacerbation is associated with decreased immunity.
Due to the low level of symptoms and the widespread sluggish form, the patient does not attach sufficient importance and does not increase the level of sanitation. Until the symptoms turn into significant problems.
Treatment of catarrhal
Effective treatment of catarrhal gingivitis begins with professional hygienic cleaning using ultrasound technology in a dental clinic by a specialist.
At the same time, preventive cleansing must be carried out every six months for each patient, regardless of the presence of gingivitis. This is due to the fact that food and bacteria can get into the invisible part of the tooth under the gum, causing the formation of hard stone that cannot be removed with an ordinary toothbrush, floss or brushes.
After cleaning, the doctor will recommend rinsing the mouth with a chlorhexidine solution (has an antiseptic effect) or special liquids for the oral cavity, as well as using an antibacterial gel twice a day (for example, Cholisal).
Important! Before applying the gel, to ensure absorption, dry the gums with a cotton swab or pad. In this case, the gel will better adhere to the gums. During application, saliva will form, no need to spit, swallow, because the gel is harmless to the stomach. After Cholisal, do not eat for 2 hours and do not drink liquids for 30 minutes.
During treatment, experts recommend using a soft brush to avoid additional injury to the inflamed gums. In normal times, medium hardness is recommended to ensure sufficient removal of contaminants.
Hypertrophic gingivitis
Refers to forms of the disease when the cause lies not only in violation of hygiene procedures, but in concomitant diseases or changes affecting the body.
Characteristic signs are an increase in gum volume, which is associated with a chronic form or fibrosis of connective tissues. The teeth in the front row are most susceptible.
Causes:
- hormonal changes in the body - pregnancy, menopause, hormonal changes in adolescents;
- disruptions of the endocrine system or other hormonal imbalances;
- malocclusion;
- poorly installed fillings (overhanging edges).
Attention! Hypertrophic gingivitis is associated with chronic processes that occur asymptomatically, aggravated by exacerbation of other diseases.
Hypertrophic forms
Stages:
- edematous - the peculiarity lies in the structure of the gum papillae, which increase not due to inflammation caused by plaque, but due to loose swelling (occurs with hormonal changes);
- fibrous - a change in the size of the gum occurs due to the growth of fibrous tissue due to the influence of traumatic factors (overhanging filling, crown or malocclusion), in this case the gum becomes dense.
Treatment of hypertrophic
Actions to combat this form are aimed at eliminating the causes that caused the disease as a consequence - normalizing or maintaining hormonal levels, high-quality dental fillings, installing suitable implants and correcting the bite.
However, regardless of the strength of the symptoms, hygienic sanitation in the dental clinic is mandatory. Further, if necessary, anti-inflammatory therapy is prescribed to reduce pain and relieve swelling from the gums:
- a course of sclerosing injections into the gums;
- pads with heparin ointment for healing;
- tissue excision.
In the absence of the necessary timely treatment, the edematous form will transition to fibrous.
Ulcerative gingivitis
Vincent's gingivitis is a severe form, accompanied by the accumulation of a critical mass of microbes under the gums and on the gingival surface and necrotic tissue death with the formation of ulcers against the background of a general decrease in oral immunity.
This disease is caused by:
- poor hygiene;
- decreased immunity;
- exacerbation of chronic diseases.
Diabetes mellitus, AIDS, vitamin deficiency, leukemia - a list of some diseases that cause the ulcerative form of gingivitis.
Treatment of the disease
Treatment of chronic catarrhal gingivitis involves a set of measures aimed at eliminating the already emerging consequences of the disease, as well as the causes that caused it. Typically, it begins with a professional teeth cleaning at the dentist's office.
The course of treatment is selected individually and depends on the form, severity and nature of the disease. Often the patient is prescribed mouth rinsing with antiseptic solutions and the oral cavity is sanitized. It involves treating caries, filling teeth, and replacing incorrectly installed fillings. This approach eliminates the possibility of relapse of the disease in the future.
Drug therapy consists of treating the oral cavity with antiseptic solutions and applications of special ointments. When treating the chronic form, it is possible to massage the gums.
It is worth noting that treatment is often carried out in combination with a diet that excludes foods that irritate the gums and is rich in vitamins A, B, E.
Treatment of chronic catarrhal gingivitis of any severity has been successfully carried out by dentists at the CELT clinic for several years now.
Gingivitis in adults: causes of the disease
The disease, which affects all categories of people (children, adults, pregnant women), occurs primarily due to weakened immunity and poor oral hygiene.
The development of the inflammatory process occurs at a low speed, so the disease is often not noticeable for a long time to an ordinary person who is far from dentistry. However, if you do not consult a doctor in a timely manner, serious complications may develop, which can lead to a more painful course of the disease and lengthy treatment.
There are three stages of development of gingivitis:
- mild (the disease affects only the spaces between the teeth);
- medium (the disease affects the edge of the gum);
- heavy.
The more time passes without treatment, the further the lesion spreads, eventually covering the oral mucosa.
The causes of the disease are divided into internal and external.
External ones include:
- injuries;
- burns of the oral cavity;
- influence of radiation;
- effects of heavy metals on the human body.
The internal reasons are as follows:
- development of molars (often during their growth, soft tissues are injured, which causes bleeding);
- lack of vitamins and minerals in the diet, which leads to decreased immunity;
- gastrointestinal diseases;
- various infections;
- neglected carious formations.
Recommendations after treatment
To avoid the occurrence of catarrhal gingivitis after treatment, you need to follow 7 rules:
- Lead a healthy lifestyle and support your immune system. Consume a vitamin-mineral complex and a sufficient amount of proteins, carbohydrates and fats.
- Prevent the transition of chronic diseases to the acute stage. Treat chronic diseases of the cardiovascular and hormonal systems, gastrointestinal tract.
- At least 2 times a year, carry out professional cleaning of the oral cavity to remove soft and hard plaque and prevent the formation of tartar.
- Use a toothbrush with medium hardness. Too soft does not sufficiently clean teeth from plaque, and hard ones can injure the enamel and cause pain with high sensitivity.
- Properly clean the oral cavity and the space between the teeth using floss and irrigator.
- Visit the dentist regularly in order to promptly detect inflammatory processes and eliminate them at an early stage.
- Choose the right toothpaste with sodium, fluoride, potassium nitrogen and other components. Entrust this task to your doctor.
If you follow these recommendations after treatment, you will confidently avoid a recurrence of catarrhal gingivitis.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
How and with what to treat catarrhal gingivitis?
Diagnosis of catarrhal gingivitis is not difficult; chronic gingivitis is clearly visible to the naked eye. To be sure, you can do a number of specific tests - and when they confirm the diagnosis, prescribe treatment. It will consist of the following stages.
- Eliminating the cause of gingivitis. This could be cleaning teeth from plaque and tartar, removing an incorrect filling, reinstalling a denture, taking a course of vitamins, etc. Very often, signs of gingivitis begin to disappear without a trace immediately after the removal of tartar.
- If recovery is slow, rinsing with a disinfectant solution is prescribed - usually a 0.06% chlorhexidine solution, but there may be other antiseptics - at the discretion of the doctor. Gargles with medicinal herbs and medicinal applications to the gums of chlorophyllipt, propolis, and special ointments can also be prescribed.
- If this is not enough, treatment is carried out with antibiotics, non-steroidal anti-inflammatory drugs, as well as gum massage, electrophoresis, etc.
There are also folk methods for treating chronic catarrhal gingivitis - rinsing with natural antiseptics brewed in milk - chamomile, sage, oak bark infusion. But you need to keep in mind that these medications alone will not eliminate the cause of gingivitis, so it will start again and again until you see a dentist. However, such remedies are excellent for consolidating the resulting therapeutic effect and preventing relapses of the disease.
There is another method of treating chronic gingivitis - injections of autoplasma containing platelets. So far, this method is rarely used as research into its effectiveness continues.
How to treat gingivitis in each specific case, and how long the treatment process will last, should be determined by the dentist. After all, the patient can be content with the disappearance of external signs of gingivitis, while the inflammatory process will continue, threatening complications.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Types of gingivitis
Based on how the disease progresses, the following types of gingivitis are distinguished:
- Acute - when it appears suddenly and its course sharply intensifies.
- Chronic - the inflammatory process proceeds slowly and the condition worsens gradually.
- Aggravated gingivitis - an increase in symptoms of chronic inflammation.
- Gingivitis in remission is a state of subsidence of symptoms.
According to the form, it is customary to distinguish the following types of gingivitis:
- catarrhal, manifested by swelling and redness of the gums;
- ulcerative, when dead areas of gum appear;
- hypertrophic, characterized by a sharp increase in gums and bleeding;
- atrophic, manifested in thinning of the gums;
- desquamative, characterized by redness and severe detachment of the upper layer of the mucosa.
According to the degree of prevalence in the oral cavity, gingivitis is divided into local (partial) and generalized (extensive).