A problem in which the blood does not clot well is called a bleeding disorder. It is caused by the fact that blood vessels do not normally become blocked when they are damaged.
When everything is fine, when there is bleeding at the wound site, the blood begins to thicken, which prevents large losses. But sometimes this complex mechanism fails, resulting in severe or prolonged bleeding.
When blood does not clot well, this does not always lead to external loss. It can also appear as bleeding under the skin or in the brain.
General information
The blood coagulation system is a complex sequential cascade of reactions occurring in the body that is aimed at stopping bleeding. The coagulation process is an important protective reaction of the body, thanks to which a constant volume of circulating blood is maintained. homeostasis system involves many components, the main ones of which are shown in the figure below.
Clotting factors are in an inactive state in the blood. If a blood vessel is injured, the coagulation process begins and all factors are sequentially activated and ensure the formation of a clot. The direct coagulation process itself is associated with the conversion of the fibrinogen protein (factor I) into insoluble fibrin.
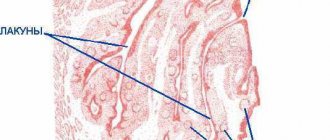
Coagulopathy is a disease, or rather a group of diseases or conditions, which are based on a blood clotting disorder. The clinical sign of coagulopathy is bleeding. Acquired coagulopathies are the most common syndromes. In this case, poor blood clotting can be caused by pathology of different parts of the coagulation system: fibrin , platelets or blood clotting factors . If any part of this system does not function or is missing, the person will have prolonged bleeding and develop a critical condition. Among coagulopathies there are congenital conditions and diseases ( hypofibrinogenemia (factor I deficiency), afibrinogenemia , hemophilia A , von Willebrand disease , hemophilia B ) and acquired syndromes that occur in various septic conditions and diseases of the kidneys and liver.
1.What is hemophilia and its causes
Hemophilia
is a blood disorder in which the blood does not clot properly. Typically, this occurs because a person with hemophilia lacks a certain clotting factor. This means it can be difficult to stop bleeding. Moreover, this can apply to both ordinary bleeding from wounds and falls, and bleeding during some operations. It also happens that some people with hemophilia begin to bleed internally for no apparent reason.
There are two main types of hemophilia:
- Hemophilia A
is caused by the absence of active blood clotting factor VIII. According to statistics, approximately 1 in 5,000 male infants are born with type A hemophilia. Blood clotting factor VIII is a plasma protein. The greater the deficiency, the more severe the symptoms of hemophilia. - Hemophilia B
(Christmas disease) is caused by a lack of active blood clotting factor IX in the body. This form of hemophilia is less common and is diagnosed in about 1 in 30,000 male infants.
Hemophilia is usually inherited and almost always affects men. In very rare cases, a person can develop hemophilia without a family history. This is called acquired hemophilia, and it occurs in both men and women.
Causes of hemophilia
Hemophilia, both type A and B, occurs due to a defect in a pair of chromosomes that affects the presence of a certain blood clotting factor in the body and how it works. In the case of acquired hemophilia, the blood clotting factor stops working as it should because it begins to be attacked by antibodies that the body itself produces.
A must read! Help with treatment and hospitalization!
Pathogenesis
The pathogenesis of hemorrhagic syndrome includes:
- damage to vascular endothelial cells by inflammatory mediators or endotoxin ;
- activation of protein C , which inhibits FV and FVIII and suppresses the synthesis of plasminogen activator inhibitor (the latter promotes the transition of plasminogen to plasmin, which breaks down the fibrin of the blood clot);
- activation of fibrinolysis, which plays a role in the development of non-stop bleeding and depletion of f I, II, V, VIII, XIII;
- accumulation in the blood of metabolites that have an anticoagulant effect.
In the pathogenesis of uremic thrombocytopathy, platelet deficiency is important, which is associated with the action of toxic plasma metabolites. In addition, patients with uremia undergo an extracorporeal circulation procedure, in which platelet dysfunction occurs due to their interaction with the tubes and membranes of the device. In this case, platelets are activated and release granules (platelet degranulation). Platelet dysfunction causes bleeding so severe that platelet transfusion is required.
Drug-induced thrombocytopenia is associated with the interaction of the drug (or its metabolite) and a platelet membrane glycoprotein. As a result of this interaction, an immunogenic complex - a glycoprotein-drug . Altered platelets are removed from the bloodstream by RPE cells. With drug-induced thrombocytopenia, the level of IgG and platelet-bound antibodies to the drug increase. Idiopathic purpura based on the production of antibodies against viral antigens. Platelets are damaged by adsorbing a viral antigen or a virus-antibody immune complex on their membrane.
Regulation of the coagulation system
Figure 6. Contribution of extrinsic and intrinsic tenase to fibrin clot formation in space. We used a mathematical model to investigate how far the influence of a clotting activator (tissue factor) could extend in space. To do this, we calculated the distribution of factor Xa (which determines the distribution of thrombin, which determines the distribution of fibrin). The animation shows the distributions of factor Xa produced by extrinsic tenase (VIIa–TF complex) or intrinsic tenase (IXa–VIIIa complex), as well as the total amount of factor Xa (shaded area). (The inset shows the same thing on a larger concentration scale.) It can be seen that activator-produced factor Xa cannot travel far from the activator due to the high rate of inhibition in the plasma. On the contrary, the IXa–VIIIa complex works far from the activator (since factor IXa is inhibited more slowly and therefore has a greater effective diffusion distance from the activator), and ensures the distribution of factor Xa in space.
[9]
Let's take the next logical step and try to answer the question - how does the system described above work?
Cascade device of the coagulation system
Let's start with the cascade - a chain of enzymes that activate each other. A single enzyme operating at a constant speed produces a linear dependence of product concentration on time. For a cascade of N enzymes, this dependence will have the form tN, where t is time. For the effective operation of the system, it is important that the response is of precisely this “explosive” nature, since this minimizes the period when the fibrin clot is still fragile.
Triggering of coagulation and the role of positive feedbacks
As mentioned in the first part of the article, many clotting reactions are slow. Thus, factors IXa and Xa themselves are very poor enzymes and require cofactors (factors VIIIa and Va, respectively) to function effectively. These cofactors are activated by thrombin, a device where the enzyme activates its own production is called a positive feedback loop.
As we have shown experimentally and theoretically, the positive feedback of factor V activation by thrombin forms the activation threshold - the property of the system not to respond to small activation, but to quickly respond when a large one appears. This ability to switch seems to be very valuable for folding: it helps prevent “false positives” of the system.
The role of the intrinsic pathway in the spatial dynamics of folding
One of the intriguing mysteries that haunted biochemists for many years after the discovery of the essential coagulation proteins was the role of factor XII in hemostasis. Its deficiency was detected in simple clotting tests, increasing the time required for clot formation, but, unlike factor XI deficiency, was not accompanied by coagulation disorders.
One of the most plausible options for unraveling the role of the internal pathway was proposed by us using spatially inhomogeneous experimental systems. Positive feedbacks have been found to be important specifically for the propagation of coagulation. Effective activation of factor X by external tenase on the activator will not help form a clot away from the activator, since factor Xa is rapidly inhibited in the plasma and cannot move far from the activator. But factor IXa, which is inhibited an order of magnitude slower, is quite capable of this (and is helped by factor VIIIa, which is activated by thrombin). And where it is difficult for him to reach, factor XI, also activated by thrombin, begins to work. Thus, the presence of positive feedback loops helps create the three-dimensional structure of the clot.
Protein C pathway as a possible localization mechanism for thrombus formation
Activation of protein C by thrombin itself is slow, but accelerates sharply when thrombin binds to the transmembrane protein thrombomodulin, synthesized by endothelial cells. Activated protein C is capable of destroying factors Va and VIIIa, slowing down the coagulation system by orders of magnitude. The key to understanding the role of this reaction was spatially inhomogeneous experimental approaches. Our experiments suggested that it stops the spatial growth of the thrombus, limiting its size.
Classification
Coagulopathies are divided into hereditary and acquired.
- Hereditary forms are associated with genetically determined changes in the walls of blood vessels, abnormalities of platelets and plasma blood factors. Hereditary coagulopathies include hemophilia A , von Willebrand disease , hemophilia B , and deficiency of various clotting factors.
- Acquired forms are most often associated with vascular damage of various etiologies (immune, toxicoinfectious and dysmetabolic), platelet damage, pathology of coagulation factors and a combination of all these factors.
The following types of acquired coagulopathy are distinguished:
- Disorders of platelet hemostasis . These include thrombocytopenia of various origins (associated with decreased platelet production, associated with increased platelet destruction, caused by non-immune causes and immune ones - idiopathic thrombocytopenic purpura), HELLP and hemolytic-uremic syndrome, thrombotic thrombocytopenic purpura, thrombocytopathies. With thrombocytopenia, the platelet germ may be primarily affected, platelets can be redistributed and accumulate in the spleen, and there will be an insufficient number of them in the blood. Also, platelets can be destroyed in large quantities (with lupus erythematosus and thrombocytopenic purpura). In addition, platelets can be consumed in large quantities during the formation of blood clots (for example, in DIC syndrome). Thrombocytopathies are characterized by the production of abnormal platelets whose function is impaired. An example of thrombocytopathy is von Willebrand disease and Glanzmann thrombasthenia .
- Types of coagulation disorders. This group includes hemostasis disorders associated with an overdose of anticoagulants ( heparin , warfarin ), hemodilution coagulopathy , vitamin K-dependent (with impaired liver function, poor absorption of vitamin K, taking certain medications).
- Coagulation-platelet (mixed) disorders that developed against the background of liver and kidney failure (hepatic and uremic coagulopathy).
- DIC syndrome is distinguished separately.
Fibrinogen plays an important role in the blood coagulation system . Normally its content is 2-4 g/l. Patients often have hypofibrinogenemia —a decrease in fibrinogen levels. This condition can be hereditary, but more often acquired, due to insufficient formation of this liver protein when it is damaged or its increased dissolution (fibrinolysis). In this condition, blood clotting slows down and as a result, a loose, disintegrating clot is formed. Hypofibrinogenemia manifests itself through the formation of bruises with minor trauma and various bleeding.
However, in most patients, decreased fibrinogen levels do not manifest themselves in any way. A decrease in the level of this protein is observed in cirrhosis , liver necrosis , bone marrow metastases leukemia , shock , anemia , eclampsia , premature placental abruption, complicated childbirth, and sepsis. The cause of acute hypofibrinogenemia is intravascular coagulation when fibrinogen is intensively consumed. Many patients with low fibrinogen levels do not require treatment. Heavy menstruation in women is prevented by hormonal agents and antifibrinolytic drugs.
Afibrinogenemia is a complete absence of fibrinogen in the blood with a normal platelet level. This is a genetically determined disease, but is very rare. In this condition, any injury leads to bleeding, hematomas, and hemorrhages in the joints. Dental manipulations and operations are accompanied by significant blood loss. Children rarely survive to adulthood. In the treatment of this pathology, replacement therapy is used: administration of fibrinogen , cryoprecipitate and fresh frozen plasma .
How to study coagulation?
To study coagulation, various models are created - experimental and mathematical. What exactly do they allow you to get?
On the one hand, it seems that the best approximation for studying an object is the object itself. In this case, a person or an animal. This allows you to take into account all factors, including blood flow through the vessels, interactions with the walls of blood vessels and much more. However, in this case the complexity of the problem exceeds reasonable limits. Convolution models make it possible to simplify the object of study without losing its essential features.
Let's try to get an idea of what requirements these models must meet in order to correctly reflect the coagulation process in vivo.
The experimental model must contain the same biochemical reactions as in the body. Not only proteins of the coagulation system must be present, but also other participants in the coagulation process - blood cells, endothelial and subendothelial cells. The system must take into account the spatial heterogeneity of coagulation in vivo: activation from a damaged area of the endothelium, the spread of active factors, the presence of blood flow.
It is natural to begin the consideration of coagulation models with methods for studying coagulation in vivo. The basis of almost all of these approaches used is to inflict controlled injury on the experimental animal in order to induce a hemostatic or thrombotic response. This reaction is studied by various methods:
- monitoring bleeding time;
- analysis of plasma taken from an animal;
- autopsy of a euthanized animal and histological examination;
- Real-time thrombus monitoring using microscopy or nuclear magnetic resonance (Figure 4).
Figure 4. In vivo thrombus formation in a laser-induced thrombosis model. This picture is reproduced from a historical work where scientists were able to observe the development of a blood clot “live” for the first time. To do this, a concentrate of fluorescently labeled antibodies to coagulation proteins and platelets was injected into the mouse’s blood, and, placing the animal under the lens of a confocal microscope (allowing for three-dimensional scanning), they selected an arteriole under the skin accessible for optical observation and damaged the endothelium with a laser. Antibodies began to attach to the growing clot, making it possible to observe it.
[7]
The classic setup of an in vitro coagulation experiment is that blood plasma (or whole blood) is mixed in a container with an activator, after which the coagulation process is observed. According to the observation method, experimental techniques can be divided into the following types:
- monitoring the coagulation process itself;
- monitoring changes in concentrations of coagulation factors over time.
The second approach provides incomparably more information. Theoretically, knowing the concentrations of all factors at an arbitrary point in time, one can obtain complete information about the system. In practice, studying even two proteins simultaneously is expensive and involves great technical difficulties.
Finally, coagulation in the body is heterogeneous. The formation of a clot starts on the damaged wall, spreads with the participation of activated platelets in the plasma volume, and is stopped with the help of the vascular endothelium. It is impossible to adequately study these processes using classical methods. The second important factor is the presence of blood flow in the vessels.
Awareness of these problems has led to the development of a variety of in vitro flow experimental systems since the 1970s. It took a little more time to understand the spatial aspects of the problem. Only in the 1990s did methods begin to appear that take into account spatial heterogeneity and diffusion of coagulation factors, and only in the last decade have they begun to be actively used in scientific laboratories (Fig. 5).
Figure 5. Spatial growth of a fibrin clot in normal and pathological conditions. Coagulation in a thin layer of blood plasma was activated by tissue factor immobilized on the wall. In the photographs the activator is located on the left. The gray expanding stripe is a growing fibrin clot.
Along with experimental approaches, mathematical models are also used to study hemostasis and thrombosis (this research method is often called in silico [8]). Mathematical modeling in biology makes it possible to establish deep and complex relationships between biological theory and experience. Conducting an experiment has certain boundaries and is associated with a number of difficulties. In addition, some theoretically possible experiments are infeasible or prohibitively expensive due to limitations in experimental technology. Modeling simplifies experiments, since it is possible to select in advance the necessary conditions for in vitro and in vivo experiments under which the effect of interest will be observed.
Causes of poor blood clotting
Based on the above, we can name the main causes of coagulation disorders:
- Vascular wall defects are hereditary (associated with collagen abnormalities) and acquired (immune or inflammatory vascular lesions).
- Pathology of platelets. Platelet dysfunction sometimes causes significant bleeding. It includes thrombocytopenia (quantitative changes in platelets) and thrombocytopathies (changes in platelet quality). Acquired thrombocytopathies are caused by taking non-steroidal anti-inflammatory drugs, dipyridamole , antibiotics , uremia , heart valve pathology, and the use of extracorporeal circulation.
- The cause of a bleeding disorder may be a lack of factors (there are thirteen of them) of the blood coagulation system or a reduced synthesis of one or more factors. Prothrombin (factor II) is the main component of blood clotting. It is a precursor of thrombin and is involved in the formation of a clot (thrombus). Fibrinogen (factor I) is produced in the liver. In the coagulation cascade, it is converted into fibrin, which participates in clot formation. The deficiency of this factor was mentioned above.
- Deficiency of factor XI is associated with hemophilia C, factor VIII with hemophilia A , and factor IX with hemophilia B. Among hereditary coagulopathies, the most common (in 95% of cases) deficiency of factors VIII and IX. Deficiency of factors VII, X, V, XI is only 1.5%. Acquired deficiency of prothrombin complex factors (II, VII, X, V) occurs in liver diseases, jaundice , dysbacteriosis , as well as in overdose of vitamin K .
- The cause of bleeding can also be increased fibrinolysis , that is, excessive fibrinolytic activity. This may be a hereditary deficiency of alpha2-antiplasmin or increased formation of plasminogen activators and impaired excretion of these activators in liver diseases.
Questions and answers
Is it possible to be completely cured of hemophilia?
Drug therapy and blood or plasma transfusion procedures relieve acute pathology syndromes. Sometimes patients are prescribed long-term use of medications selected based on medical history. But completely eliminating the symptoms of hemophilia remains impossible.
Does hemophilia pose a threat to a child's life?
If parents seek medical advice in a timely manner, the baby will be out of danger. A quick correct diagnosis and initiation of treatment will allow the child not to limit himself in physical activity and games.
Can a boy with hemophilia pass it on to his sons?
The risk of having children with hemophilia from a father with bleeding problems is minimal. The disease will be inherited by sons only if their mother is one of the carriers of the altered gene.
Symptoms
Whatever the cause of coagulopathy, the main symptom is bleeding of varying severity - from small bruises to severe bleeding during injuries (including minor ones). On the skin side, patients experience small petechiae , hematomas , bruises at injection sites, nasal and gingival bruises, heavy uterine bleeding in women, and often gastrointestinal bleeding.
Thrombocytopathies , both congenital and acquired, are not accompanied by severe hemorrhages . Bleeding in such patients can develop only during operations, injuries and tooth extraction. The most common manifestations are bruising and periodic nosebleeds and gum bleeding.
Thrombocytopenic purpura is a very common disease, especially among women 20-30 years old. Patients develop petechiae , bloody blisters that rise above the skin, bleeding gums and heavy uterine bleeding. The disease begins either gradually or acutely with hemorrhagic syndrome. According to its manifestations, there are two types of purpura: “wet”, when hemorrhages are combined with bleeding, and “dry”, if the patient has only skin hemorrhages. Hemorrhagic syndrome on the skin is observed in 100% of patients.
The number of hemorrhages can be single or multiple. Cutaneous hemorrhagic syndrome is characterized by:
- Various hemorrhagic rashes - petechiae and large hemorrhages.
- Inconsistency of hemorrhages with the degree of injury.
- Spontaneous appearance at night.
- Different colors of skin hemorrhages depending on the age.
- Painless.
- Asymmetry of elements.
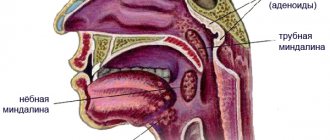
- Hemorrhages in the soft palate and tonsils, sclera, fundus. Scleral hemorrhage sometimes precedes severe cerebral hemorrhage, which occurs quickly and progresses.
- Manifested by dizziness , headache , convulsions .
With von Willebrand disease, there is a tendency to intradermal hemorrhages, effusions of blood into the mucous membranes and severe bleeding after injury.
Tests and diagnostics
Coagulological screening includes:
- prothrombin index;
- activated partial thromboplastin time;
- amount of fibrinogen;
- platelet count;
- bleeding time.
In case of isolated prolongation of activated partial thromboplastin time, proceed to the second stage of examination:
- do a correction test;
- activity of factors VIII, IX, XI, XII.
If the activity of factor VIII decreases, they proceed to the third stage of examination:
- lupus anticoagulant;
- specific inhibitor of factor VIII.
In children
Poor blood clotting in a child is often associated with immune thrombocytopenic purpura . Acute purpura develops between the ages of 2 and 9 years. This is an immune-related disease characterized by a constant (or periodic) decrease in platelets of less than 100 thousand. The disorder in children occurs 1-3 weeks after a viral infection. Such pathological reactivity can start not only under the influence of a viral infection, but also after taking medications, vaccination, exposure to temperatures (both low and high), surgical interventions or emotional stress. Against the background of normal health, the child develops a petechial rash (on the mucous membranes and skin), bruises, repeated nosebleeds and bleeding gums. In severe cases, there may be brain hemorrhages and stomach bleeding. Since antigens gradually leave the blood, in most people the disease goes away on its own after 2 months.
Vitamin K deficiency coagulopathy occurs in children in the first months of life and newborns . With Vit-K deficiency, the activity of several factors decreases: prothrombin , proconvertin , Christmas factor and Prower factor . hypocoagulation develops , accompanied by hemorrhagic syndrome.
Causes of Vit-K deficiency in a newborn:
- taking anticoagulants during pregnancy;
- antibiotics;
- anticonvulsants;
- severe damage to the pregnant woman’s liver and intestines;
- the presence of fetoplacental insufficiency;
- gestosis and preeclampsia .
The manifestations of this coagulopathy in newborns are not very specific - skin syndrome, increased bleeding during blood sampling and bleeding from the umbilical wound. With a lack of Vit-K, the duration of bleeding and platelet levels are within normal limits. Many authors recommend prophylactic administration of Vit K to all children immediately after birth - 2-3 administrations for the first 1.5 months, and in some cases weekly administration continues up to 3 months.
In later life, Vit-K deficiency coagulopathy is caused by breastfeeding only. At the same time, 78% of children develop massive intracranial hemorrhages. Much less frequently, the cause of decreased coagulability in children is disseminated intravascular coagulation syndrome in severe sepsis, congenital metabolic changes and hereditary coagulopathies.
Poor blood clotting during pregnancy
A normal pregnancy is always accompanied by important biochemical changes, including in the hemostatic . However, there are pathological conditions that lead to blood clotting disorders. Coagulopathy in pregnancy, what is it? This is a pathological condition that occurs with impaired coagulation and an increased risk of bleeding.
Pathological bleeding in pregnant women can be caused by:
- Congenital disorders in the coagulation system.
- Werlhof's disease.
- Moschkowitz disease.
- Antithrombin deficiency , which often occurs during pregnancy.
- Preeclampsia.
- Eclampsia.
- DIC syndrome associated with preeclampsia. At the first stage, intravascular coagulation occurs, and then the coagulation system is depleted.
- HELLP syndrome, which is also associated with preeclampsia (hemolysis, elevated liver enzymes and thrombocytopenia). Disseminated intravascular coagulation syndrome, a combination of thrombosis and bleeding.
- HELLP syndrome combines a triad of manifestations: hemolysis , decreased platelet levels and increased liver enzymes. During pregnancy with severe preeclampsia, the frequency of this syndrome reaches 20%.
- It develops during full-term pregnancy, premature birth and even after childbirth. HELLP syndrome is considered a subtype of preeclampsia. Diagnostic criteria for this syndrome: platelets less than 100×10 in 9/l, transaminases 2-3 times higher than normal, hemolysis of erythrocytes, bilirubin more than 20.5 µmol/l.
Women experience nausea , swelling and pain in the right hypochondrium. Pregnant women with HELLP syndrome are prescribed magnesium sulfate before and after birth for two days. Platelet transfusion is indicated when platelets are less than 20 × 10 in 9/L if a natural birth is expected and when platelets are less than 50 × 10 in 9/L if a cesarean section . Thromboconcentrate is administered before delivery. Corticosteroids increase platelet levels, so their use is reasonable. In the postpartum period, plasma exchange is used.
In DIC syndrome, a short phase of hypercoagulation is replaced by hypocoagulation. Such changes occur if a woman loses 15-20% of her blood volume. In case of bleeding, a platelet concentrate is infused.
In case of bleeding and if the prothrombin time and activated thromboplastin time are increased, an infusion of fresh frozen plasma is performed. If it is not possible to administer plasma, clotting factor concentrates are administered. Severe hypofibrinogenemia , which is not corrected by plasma transfusion, is then transfused with cryoprecipitate . For hyperfibrinolysis and bleeding, tranexamic acid . Hemolytic-uremic syndrome in women is accompanied by thrombocytopenia , kidney damage and microangiopathy . This condition most often develops after childbirth. Plasma exchange in this pathology is not very effective - the woman requires hemodialysis .
Hemostasis is the process that stops bleeding
Why does blood clot? Few people think about this crucial mechanism. It’s only after cutting yourself that the thought sometimes slips into your mind: “Why doesn’t the bleeding stop for so long?” The basics of this process are quite a complex topic. But you still need to know the minimum.
In many developed countries, starting from school, classes are held that teach children how to act in emergency situations. Such situations include sudden cardiac arrest, drowning, and trauma, which are often accompanied by external bleeding. For an unprepared person, the sight of human blood can prevent him from taking the right actions. Moreover, it can put a person into panic and stupor. In this case, wasting time is an unaffordable luxury. In the case of bleeding from large arteries, the outcome can be determined in seconds.
What happens in the body when there is bleeding?
The physiology of hemostasis, the process aimed at protecting life during bleeding, is complex. One can only marvel at how thoughtfully nature created man. Hemostasis mechanisms are activated instantly as soon as a blood vessel is damaged. When the inner layer of the vessel or endothelium is damaged, substances are released that signal bleeding. These are serotonin and thromboxane. Pain and these substances cause spasm of the smooth muscles of the damaged vessel, which leads to a decrease in blood flow and blood loss. Thromboplastin, a substance also released during injury, causes activation of platelets and a cascade of reactions leading to the formation of a blood clot. Thrombus is a blood clot that acts as a “plug”. It prevents bleeding.
How does a blood clot form?
Primary, or vascular-platelet, hemostasis is caused by vascular spasm and platelet aggregation. Platelets are small blood cells that have the ability to form a lump when activated. They stick to the edges of the damaged area and to each other. In this case, platelets are a source of biologically active substances that trigger the cascade of the coagulation system or coagulation hemostasis. Under the influence of these substances, as a result of a complex reaction at the site of injury, long threads of protein - fibrin - are formed in the blood. Fibrin strengthens the platelet clot and helps to reliably stop bleeding. Fibrin is constantly present in blood plasma in the form of inactive fibrinogen. Special proteins that regulate the process of fibrin formation, or coagulation factors, are also found in the blood plasma. This is why coagulation hemostasis is also known as plasma hemostasis.
A detailed diagram of hemostasis in the specialized literature takes up more than one page. It is important to conclude: to quickly stop bleeding, it is necessary to create conditions that facilitate the work of the hemostatic system. For example:
- if the wound is on a limb, use a tourniquet, this will slow down or stop blood circulation and bleeding;
- the wound must be squeezed or clamped tightly to reduce the lumen of the vessel;
- if possible, put cold on the wound (snow, ice, cold water in a bottle) to cause vasospasm;
- if a limb is injured, raise it high to slow down the blood flow;
- When applying a pressure bandage or covering the wound with a bandage or other dressing material, the bandage must not be removed or changed, even if bleeding continues. This can destroy an already formed but still weak blood clot, and the bleeding may increase. You should increase the pressure on the wound and use more bandages to get the person to the hospital faster.
Pathologies of the hemostatic system
Impaired hemostasis is a serious pathology. There are diseases in which the formation of a blood clot is impaired and (or) there is a risk of uncontrolled bleeding. Diseases of the hemostatic system:
1. Plasma hemostasis:
- violations of the synthesis of coagulation factors VIII and IX (hemophilia);
- von Willebrand disease;
- disseminated intravascular coagulation syndrome;
2. Platelet hemostasis:
- thrombocytopenia (decreased platelet count);
- Werlhof's disease;
- von Willebrand disease (platelet form);
- thrombasthenia and other diseases.
If a patient with these diseases bleeds, hemostasis will not be initiated properly. The extent of the damage is of great importance. Contrary to popular and erroneous belief, minor cuts and scratches usually do not pose a danger, but any pathology of hemostasis can lead to serious complications during surgical interventions and injuries.
Vascular-platelet hemostasis in people with hemophilia is the only mechanism that can stop bleeding.
Assessment of the state of the hemostasis system
The study of hemostasis is a mandatory item when preparing for surgery, during pregnancy and childbirth. Various analyzes and tests are carried out. Hemostasis and its condition can be assessed using a special analysis - a coagulogram or hemostasiogram. To carry out the analysis, blood must be taken from a vein. The study is carried out in vitro. Hemostasis can be examined by doing the following tests:
- blood clotting time or UCT;
- thromboelastography;
- prothrombin time;
- prothrombin test;
- activated partial thromboplastin time;
- level of fibrin degradation products (d-dimer, RFMK);
- thrombodynamic test, etc.
Based on the test results, it is possible to assess the state of the entire hemostatic system as a whole, or separately plasma and platelet hemostasis. An analysis for complete hemostasis is carried out in case of suspected coagulopathy (for example, hemophilia), to diagnose pathologies of the hemostatic system, in many diseases accompanied by disorders of the hemostatic system (oncological diseases, coronary heart disease, emergency conditions). The hemostasis laboratory is a special department in hospitals that performs these complex tests.
Molecular medicine methods have recently begun to be used to diagnose hereditary pathologies. Modern science allows us to look into a person’s genes and find out what features of the hemostatic system he has, what mutations have occurred, whether there is a disease or a risk of developing coagulation system disorders. The analysis is called polymorphism of hemostasis genes.
The Hemostasis Pathology Center is a leading medical institution that performs all types of necessary tests and provides medical care to patients with hemostasis pathologies. In the regions, this function is performed by the hemostasis center. Chelyabinsk, for example, on the basis of city clinical hospital No. 11, created such a center that serves the entire Southern Urals.
Hereditary diseases of the hemostatic system are a serious problem. Hemophilia is diagnosed in thousands of newborns around the world every year. Treatment of these pathologies is expensive and requires huge expenses. Most patients do not receive proper care.
Hemostasis disorders that occur in other diseases are of great importance in treatment. For example, with atherosclerosis, myocardial infarction, stroke, cancer, varicose veins of the lower extremities.
coagulogram, hemostasis
Prevention
It is impossible to influence congenital pathologies of the coagulation system, but people with such pathologies can take a more careful approach to their health, choice of profession and physical activity. Secondary prevention includes the following:
- Avoid physical activity associated with the possibility of getting bruised (sports, football, wrestling, figure skating, etc.).
- Oral hygiene that helps reduce the need for dental procedures and surgeries.
- Normalize weight, which puts stress on the joints and increases the risk of bleeding into the joint cavity.
- Avoid the use of medications that affect clotting. Among such drugs are acetylsalicylic acid , Clopidogrel , Caffeine , Ibuprofen , Naproxen , nitrofurans , barbiturates , carbenicillin .
- Women with congenital factor deficiencies should consult and be examined by a geneticist and find out the risks of having a child with a congenital blood clotting disorder.
Similarly, there is no primary prevention of thrombocytopenic purpura , and secondary prevention is limited to preventing exacerbations. Patients should not be exposed to the sun; they are contraindicated from working in conditions of elevated temperature (hot shop, food shop near the stove). Children are exempt from physical education. After each case of ARVI, it is mandatory to test the blood.
Consequences and complications
With coagulopathies, the following complications may occur with varying probability and severity:
- Anemia.
- Hematuria (blood in the urine).
- Heavy and prolonged periods.
- Brain hemorrhage
- Gastrointestinal bleeding.
- Hemorrhage into the structures of the eye, pleurisy, compression of the larynx and trachea by hematomas.
- Hemorrhage into the joints and, as a consequence, the development of arthritis , arthrosis , osteoporosis and posthemorrhagic bursitis .
- Intravertebral hemorrhages.
- In rare cases, death due to massive bleeding.
Forecast
Acute forms of idiopathic purpura disappear within a few months and it often happens that the disease does not recur. In the chronic form, it is possible to induce remission, but the disease often recurs.
When using modern medications and following all recommendations for lifestyle changes and employment, thrombocytopenic purpura has a favorable prognosis.
Untreated hemophilia Lack of treatment often leads to joint pathology ( hemophilic arthropathy ), which then requires the use of crutches and wheelchairs or special orthopedic treatment. During treatment, life expectancy is practically no different from healthy individuals.
List of sources
- Fatkullin I.F., Zubairov D.M. Hereditary and acquired defects of the hemostatic system in obstetric and gynecological practice. M., 2002. P. 64.
- Galstyan G.M., Sukhanova G.A. Introduction to hemostasis, modern blood products and their effect on coagulation // Medical Council. 2013. from 11-13.
- Barkagan Z.S. Diagnosis and controlled therapy of hemostasis disorders / Z.S. Barkagan, A.P. Momot. – M.: Newdiamed, 2001. – 296 p.
- Barinov S.V., Dolgikh V.T., Medyannikova I.V. Hemocoagulation disorders in pregnant women with gestosis. Journal of Obstetrics and Women's Diseases. – 2013; 62 (6): 5–12.
- Degtyarev D.N., Karpova A.L., Mebelova I.I. and others. Draft clinical recommendations for the diagnosis and treatment of hemorrhagic disease of newborns // Neonatology. 2015. No. 2. P. 75–86.
Summarizing
In recent years, the complexity of the coagulation system has gradually become less mysterious. The discovery of all essential components of the system, the development of mathematical models and the use of new experimental approaches made it possible to lift the veil of secrecy. The structure of the coagulation cascade is being deciphered, and now, as we saw above, for almost every significant part of the system, the role it plays in the regulation of the entire process has been identified or proposed.
Figure 7 shows the most recent attempt to reconsider the structure of the coagulation system. This is the same diagram as in Fig. 1, where parts of the system responsible for different tasks are highlighted with multi-colored shading, as discussed above. Not everything in this scheme is securely established. For example, our theoretical prediction that activation of factor VII by factor Xa allows clotting to respond in a threshold manner to flow rate remains as yet untested experimentally.
Figure 7. Modular structure of the coagulation system: the role of individual coagulation reactions in the functioning of the system.
[1]
It is quite possible that this picture is not yet completely complete. However, progress in this field in recent years gives hope that in the foreseeable future, the remaining unsolved regions of the coagulation circuitry will gain meaningful physiological function. And then it will be possible to talk about the birth of a new concept of blood coagulation, which replaced the old cascade model, which faithfully served medicine for many decades.
The article was written with the participation of A.N. Balandina and F.I. Ataullakhanova and was originally published in Priroda [10].