From this article you will learn:
- what to do if a child has an abscess on his gum,
- Do I need to remove a baby tooth?
- how the treatment is carried out (video),
- how to distinguish a purulent lump from a cyst on a child’s gum.
The article was written by a dentist with more than 20 years of experience.
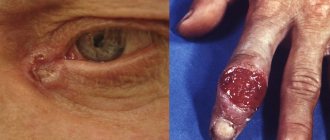
An abscess on the gum in children usually looks like a red or yellowish lump located in the projection of the root of one of the teeth, which caused the inflammation. The inside of such a lump is filled with pus, and it has a yellowish color if the mucous membrane is thin and then the pus shines through it. The appearance of such a lump on the gum above a tooth in a child is always evidence of the development of purulent inflammation at the apex of the roots of a baby or permanent tooth, and indicates the development of apical periodontitis.
Apical periodontitis of primary and permanent teeth in children is most often associated with the lack of timely treatment of caries and pulpitis, as well as with mechanical trauma to the front teeth, for example, due to a fall. Therefore, caries or an old filling can always be found on the causative tooth, and if we are talking about an injury, there may be a chip of the enamel or a fracture of the tooth crown. In cases where the traumatic impact does not lead to damage to the hard tissues of the tooth, the crown of the tooth may be stained bluish or gray.
Abscess on a child’s gum: photo
Immediately before an abscess appears on the gum, children usually complain of pain or discomfort in one of the teeth, which is associated with the formation of pus at the apex of the tooth root. But after a pus-filled lump forms on the gum, children in most cases immediately feel relief (only pressing on the lump with your fingers can remain painful). Next, the lump may spontaneously open with the formation of a fistula, from which pus will leak into the oral cavity, or this may require an incision in the gums.
Important: however, not every lump on the gum indicates the development of purulent inflammation. There are also so-called eruption cysts. For example, even 2-3 weeks before the eruption of a baby or permanent tooth, a cyst may form on the child’s gum, which will have a bluish color (Fig. 7-8). We will also talk about such cysts at the end of the article.
What does a purulent abscess on a child’s gum look like (video) –
Causes of stomatitis
Inflammation of the oral mucosa can be caused by various reasons.
- Mucosal injury6.
- Viral, bacterial or fungal infection6.
- Allergy2.
- Immunity disorders (autoallergy, that is, a reaction to one’s own altered tissues2).
- Diseases of the blood, digestive, cardiovascular, nervous and endocrine systems2.
- Hypovitaminosis - lack of vitamins C, B1, B12, E, D32.
- Common infectious processes: measles, rubella, scarlet fever and diphtheria, infectious mononucleosis, tuberculosis and others1.
Only a specialist can understand the causes of stomatitis. Therefore, if symptoms of the disease appear, you should definitely contact your dentist.
Inflammatory diseases of the oral cavity can occur in a child of any age6. Immaturity of the body is the primary factor predisposing to the occurrence of stomatitis in children under one year of age. The mucous membrane of the oral cavity during this period of a child’s life is very vulnerable, its natural protective properties are reduced. The immunity received from the mother during fetal development and which protected the baby immediately after birth weakens every day. Therefore, the infection easily penetrates the mucous membrane and causes its inflammation. Most often at this age, candidal stomatitis occurs, commonly called thrush1,6.
From the age of one to 3 years, children actively develop immune mechanisms to protect the oral mucosa (local immunity), but its permeability to viruses remains extremely high. Therefore, in a 2-3 year old child, stomatitis is more likely to be viral, in the vast majority of cases - herpetic1,3,4.
From 4 to 12 years of age, stomatitis in children is more often caused by allergic and autoimmune reactions. In particular, chronic aphthous forms of the disease occur during this period1.
Up to contents
If the causative tooth is still a baby tooth -
When writing this section, we used the “National Guide to Pediatric Therapeutic Dentistry” (edited by Professor V.K. Leontyev). Let's figure out what parents need to know... The presence of a swelling/bump on the gum, or a fistula, indicates the development of acute periodontitis, or an exacerbation of chronic periodontitis. In the vast majority of cases, baby teeth that have caused the appearance of ulcers on the gums must be subject to mandatory removal. The fact is that in most cases the roots of baby teeth will either not yet be formed or will already have signs of resorption (see photo below).
In both cases, this will not allow for high-quality obturation (filling) of the root canal lumen with filling material. Poor quality filling will certainly lead to the development of purulent inflammation, and in severe cases, sepsis, which even poses a threat to life. Injury to the permanent tooth germ is also possible, both during root canal treatment and as a result of the development of purulent inflammation in the area of the apex of the roots of a baby tooth.
Milk teeth for removal (with signs of resorption) –
But the physiological immaturity of the immune system of children also poses a problem for the treatment of such teeth, which in this situation also contributes to the development of purulent complications. Therefore, to determine the possibility of treatment, we first need a targeted Rg image, which will show the degree of resorption, as well as the presence of foci of inflammation at the apex of the roots of a baby tooth. Below we will list when such teeth require mandatory removal, and in what situations you can try endodontic root canal treatment in baby teeth.
Indications for mandatory removal:
- if there are less than 2 years left before the physiological change,
- if the tooth crown is severely damaged and cannot be restored,
- the tooth has degree II-III mobility,
- in the presence of a fistula tract,
- if the x-ray shows signs of root resorption (we are talking not only about external root resorption, but also about internal one),
- if the image shows a pronounced inflammatory focus of bone tissue destruction (at the apex of the root of a baby tooth), i.e. we are talking about an exacerbation of chronic granulating periodontitis,
- if the child belongs to health groups III, IV, V,
- if the child has caries in the area of most teeth (decompensated form of the carious process).
Possibility of endodontic treatment:
- if the root of the baby tooth is formed and does not show signs of resorption,
- in the absence of tooth mobility,
- in the absence of a fistula tract,
- if the focus of inflammatory destruction at the apex of the root of a baby tooth is very small in size, and at the same time is separated from the permanent tooth germ by a layer of unchanged bone tissue. Filling the canals of a baby tooth (before and after photos) –
Important: you should also take into account that such treatment is very complex and requires a highly qualified pediatric dentist, as well as a large amount of time per patient. Therefore, this is unlikely to be a good idea – if we are talking about public medicine. Also, endodontic treatment will require several visits, and subsequently regular follow-up with radiography (parents must be prepared for this). You also need to consider how important this tooth is in terms of preventing malocclusion.
Filling canals in a baby tooth (video):
In the video below you can see the process of filling root canals in the 1st primary molar. Please note that mechanical treatment of root canals was performed using an endodontic tip and modern rotary files (created specifically for children's teeth). The most modern paste based on calcium hydroxide and iodoform was used as a material for filling root canals in baby teeth. At the end of the video, you will be able to see an x-ray that shows the quality of root canal filling. In this case, I would like to say about the excellent work of the doctor.
A few more things parents should know:
Unfortunately, in recent years, due to the deterioration in the quality of training of doctors, you can hear that many pediatric dentists recommend not removing such teeth, citing the fact that removal will cause malocclusion. And therefore, very often children continue to walk with chronic inflammation at the roots of their baby teeth. In part, the effect of early removal of baby teeth on the bite is true (but primarily only in relation to baby molars, the removal of which can lead to a shift in the rudiments of permanent teeth). But this is not the only thing to consider.
The fact is that the purulent focus of inflammation in the area of the roots of a baby tooth is separated from the permanent tooth germ by only 1-2 mm of bone (Fig. 6). Studies have shown that disruption of the eruption of permanent teeth is caused not only by the early removal of baby teeth, but also by the influence of pyogenic bacteria and their toxins on the rudiments of permanent teeth. For example, you did not remove a child’s baby tooth with inflammation at the apex of the root, and this will also delay the eruption of a permanent tooth. In addition, inflammation at the root of a baby tooth can even lead to the death of a permanent tooth germ (this happens especially often if inflammation occurs before the start of mineralization processes in the permanent tooth germ).
Important: you also need to take into account the effect of a pyogenic infection on the general health of the child. For example, the fact that infection from the source of inflammation will constantly enter the submandibular lymph nodes, causing the development of lymphadenitis. In addition, once in the blood, waste products of pyogenic bacteria affect the entire body as a whole - they increase the risk of developing allergies, bronchial asthma, diabetes, heart and joint diseases.
If purulent inflammation is accompanied by the formation of a fistula, then you must understand that pus will constantly enter the oral cavity through the fistula, the child will swallow it, and this will lead to the colonization of the tonsils with a pyogenic infection and the development of chronic tonsillitis. And in this case, the development of a sore throat or constant regular exacerbations of chronic tonsillitis is guaranteed for the child.
Traumatic stomatitis
Inflammation of the mucous membrane in the mouth can be preceded by trauma: mechanical, thermal, chemical, radiation1,6.
Small children who put everything in their mouths can injure the mucous membranes with the sharp edges of toys or household items. Injuries often occur due to inept use of cutlery as a result of falls. In older children, stomatitis may be associated with a thermal burn, blows to the teeth, or the bad habit of chewing a pencil or pen. Sometimes the cause of inflammation is dental diseases and their treatment: sharp edges of damaged teeth and fillings, braces and aligners1.
When stomatitis develops in a child on the gum, on the inner surface of the cheek or in another place, the mucous membrane becomes red and swollen, and a painful erosion or ulcer may appear in the area of damage. Since there are many microorganisms in the mouth, there is always a risk of a bacterial or fungal infection1.
If the mucous membrane is constantly injured, painless whitish or whitish-gray layers may form on it.
In children under 1 year of age, stomatitis can be the result of using the wrong nipples: long, tight, irregularly shaped. The resulting Bednar aphthae are located in the area of the transition of the soft palate to the hard palate and are round erosions or ulcers1.
Treatment of traumatic stomatitis in children includes:
- elimination of traumatic factors;
- rinsing the mouth, irrigating the mucous membranes and treating wounds with drugs with an analgesic and antiseptic effect1.
Up to contents
Causes of purulent-inflammatory pathologies
Gingivitis
Gingivitis in children occurs due to regular poor oral hygiene, accumulation of plaque, and deposition of stones. The situation is aggravated by factors such as crowded teeth, malocclusion, installed braces and other orthodontic structures.
Ulcers are formed due to untreated caries and improper oral care.
A fistula is the result of neglected infectious processes, a consequence of improper treatment of dental diseases.
What symptoms should parents be wary of?
The first signs of unhealthy gums are bad breath and bleeding when brushing your teeth.
Upon examination, you can see reddened areas above the teeth. Pus does not always provoke a rise in overall body temperature. Swelling of the face or pain in the initial stages is mild or absent.
Abscess
An abscess on the gum of a child is distinguished by the specificity of its symptoms - a feeling of local distension, pain, the formation of a tubercle, where decay products gradually accumulate in the form of a foul-smelling liquid. As the disease progresses, physical activity decreases and appetite disappears.
Treatment methods
Important! Self-treatment of a fistula on the gum of a child, or other diseases in the form of rinses, lotions, and ointments is unacceptable. This is dangerous due to such consequences as gumboil, loosening and loss of permanent teeth, and periodontal disease. In severe cases - transition to a chronic condition, decreased immunity, frequent viral infections of the body, partial or complete paralysis of the facial nerve.
Fistula
At the dental clinic "Podmoskovye" we take a professional approach to treatment, which includes the following stages:
- detailed diagnostics - examination, instrumental examination;
- drawing up a treatment plan in a clinical setting;
- Recommendations for caring for your oral cavity at home.
Only an integrated approach will preserve the health of the oral cavity until the dental system is fully formed.
Read more about our pediatric dentistry in the Pediatric Dentistry section
Viral stomatitis
About 80% of all stomatitis in children is caused by herpes viruses3,5. In approximately 70% of cases, the disease develops in children aged 1 to 3 years3,4.
The disease can occur in mild, moderate and severe forms.
With mild herpetic stomatitis, the general condition is practically not disturbed. Body temperature does not exceed 37-37.50 C. Symptoms of inflammation are limited to swelling of the gums and usually the simultaneous appearance of single painful herpetic blisters and erosions on the mucous membrane (no more than 6). After 1-2 days, the contours of the lesions are blurred, the rashes turn pale, and the erosions heal without scarring3.
With moderate stomatitis, the child’s temperature reaches 38-390 C and lasts until rashes continue to appear. General intoxication manifests itself in the form of weakness, headache, nausea. The child becomes capricious, lethargic, refuses to eat and play3.
As the temperature rises, the oral mucosa becomes red and swollen, and the gums begin to bleed. The number of herpetic elements reaches 20-25, repeated rashes are accompanied by fever3.
Severe stomatitis in children looks like a common acute infectious disease and is accompanied by severe intoxication: fever 39-400 C, chills, headache, aching muscles and joints, heart rhythm disturbances, nosebleeds, nausea and vomiting. The number of herpetic elements can reach 100; they are located not only in the mouth, but also on the skin of the face, on the eyelids and conjunctiva of the eyes, and earlobes. In addition, upper respiratory tract symptoms may be present.3
Treatment includes treating the affected area with painkillers and antiseptic drugs, antiviral therapy, drinking plenty of fluids, a balanced diet and proper nutrition3,5.
Up to contents
Symptoms of stomatitis in infants
The characteristic symptoms of stomatitis in infants depend primarily on the form of the disease.
General signs of the disease:
- The appearance of sores or blistering rashes on the gums, tongue, and inner cheeks
- Heat
- Signs of intoxication, muscle pain
- Induration of the lymph nodes, their local soreness
- Bad dream
- General malaise, refusal of food and water
- Possible vomiting and severe headache3
Infants most often experience viral and candidal stomatitis - lesions of the mucous membrane caused by Candida viruses or fungi. But the newborn may also experience other forms of the disease, including bacterial and aphthous stomatitis.
Among viral stomatitis, the herpetic form of the disease is more common. The main symptom of stomatitis due to the herpes virus is a blistering rash on the tongue and lips. The blisters break open and form ulcerative defects, which are very painful. The mucous membrane of the gums of the tongue and lips has a bright red tint.
The candidal form of stomatitis is manifested by a specific white or dirty-gray coating on the back of the tongue, cheek area and gums. With this disease, children’s appetite disappears, the baby may completely refuse a bottle, become very capricious and sleep poorly. The oral mucosa becomes dry, a burning sensation occurs, and bad breath may appear.
Bacterial stomatitis is accompanied by redness of the oral mucosa, the formation of ulcers, and yellow crusts that stick together the lips. Salivation increases and bad breath appears.
With aphthous stomatitis, the child becomes passive, lethargic, painful round ulcers appear on the mucous membrane of the buccal area and lips, which have a characteristic white coating on top4.
Candidal stomatitis
In 80% of healthy children, Candida fungi can be found in the oral cavity. They get there during childbirth, from nipples and pacifiers, from care products, in contact with the mother's skin, with food during eating and usually do not cause any problems. Candidal stomatitis, or thrush, occurs when immunity decreases1.
Predispose to the disease:
- prematurity and postmaturity;
- developmental defects and concomitant diseases;
- treatment with antibiotics and hormones;
- artificial feeding;
- poor care and poor feeding hygiene;
- Using the wrong nipples1.
What does candidal stomatitis look like? In children's mouths, whitish or whitish-gray dotted formations appear on the reddened mucous membrane. They merge into films of a cheesy nature; when the films are rejected, bright red painful erosions are formed. Because of the pain, the baby becomes restless, cries often, sleeps poorly, and refuses to eat1.
In severe cases of candidiasis, a cheesy coating may appear on the palate and on the lateral surfaces of the tongue, on the tonsils and the back wall of the pharynx - candidal tonsillitis and pharyngitis develop1.
If your child has a fungal infection, you should always consult a doctor; he will tell you how and what to treat the mucous membrane with candidal stomatitis, so that the child does not have complications and recovers faster. Treatment, as a rule, involves treating the oral cavity with drugs with antifungal activity (chlorhexidine, hexethidine). In severe cases of the disease, antifungal agents, probiotics and immunomodulators are prescribed1.
Up to contents
Gingivitis in children: what are the causes and symptoms
Gingivitis, or inflammation of the mucous membrane around the teeth in children, is a fairly common phenomenon. Most often, gingivitis can be detected in a child aged 1–3 years, as well as in adolescence - in both cases, the “trigger” of the disease can be active growth of the body, hormonal changes and features of the formation of the immune system
Gingivitis in children develops quite quickly. If inflammation develops in a child’s mouth, the number of bacteria increases significantly compared to the norm. Within 72 hours, the process of stone formation from soft plaque begins, and the first signs of gum erosion appear. If the situation is neglected, this can lead to the loss of teeth in children - both milk and permanent.
Symptoms of gingivitis in children
How does gingivitis manifest itself in children? The symptoms are:
- bad breath
- discomfort, pain in the mouth
- bleeding gums
At the same time, the temperature with gingivitis in children does not always rise. Therefore, it is quite easy to miss the onset of the disease. A child may tolerate discomfort without attaching any importance to it, or endure it, fearing a visit to the dentist (especially if he has already had a bad experience with dental treatment). That is why it is necessary to unobtrusively check the oral health of your son or daughter from time to time. For kids this can be done during play, but for a teenager you will have to find a psychological approach. Perhaps it would be easier (and more correct!) to “introduce” your offspring to a professional dentist whom he can trust, and periodically take him for preventive examinations.
Types of gingivitis in children
Only a competent doctor can determine what form of gingivitis a child is suffering from and, accordingly, prescribe effective treatment that quickly relieves discomfort. The disease can manifest itself in different ways:
- Catarrhal gingivitis. Children aged 3–7 years are most often affected. It is accompanied by swelling of the tissues around the tooth, unpleasant taste in the mouth, pain when pressure is applied to the gums, the appearance of pink saliva, general malaise and tearfulness. This type of disease easily becomes chronic, when gingivitis occurs approximately twice a year, causes temporary inconvenience to the child and seems to go away on its own. In fact, each time the inflammatory process becomes more and more severe, hard dental deposits are formed, which can ultimately “develop” into periodontitis - a disease in which the bonds of the tooth with the surrounding tissues are destroyed, which leads to its loss.
- Hypertrophic gingivitis. Painful sensations in a child do not appear immediately. The area of the front teeth is most often affected - the gums swell, changing their color (up to purple-blue). Over time, the tissues grow, covering a significant part of the tooth area, gum pockets appear, pus begins to be released, and severe pain appears.
- Atrophic ginivitis. This form of gingivitis is characterized by “recession” of the gums: the neck (and sometimes even the root) of the tooth is exposed, the child feels discomfort from eating cold and hot food. In this case, the gums become pale and bleed slightly. This is not only unpleasant and unsightly, but also quite dangerous and difficult to treat: you will most likely have to restore the shape of the gums using mini-plastic surgery.
- Ulcerative gingivitis. This is one of the options for the development of catarrhal gingivitis: the inflammatory process does not become chronic, but intensifies. Bleeding ulcers appear in the child's mouth, covered with a gray film - this is dead gum tissue. The child cannot eat and sleep normally, experiences severe pain, his body temperature rises to 39 °C... This development of the disease can be avoided by consulting a doctor at the first signs of gingivitis in the child.
Causes of gingivitis in children
Of course, parents want to believe that they will not have to treat gingivitis in children, knowing the causes of its occurrence. It’s really important to know them - they can be:
- Systemic diseases of the body (failure of the endocrine, cardiovascular, digestive, hormonal systems, the influence of infection)
- Dental pathologies, bite defects and errors in their correction
- Incorrect installation of fillings or their deformation
- Advanced caries, careless attitude of parents towards the health of the child’s teeth
- Weakened immunity, lack of vitamin C, poor appetite
But the main and main reason for the development of gingivitis in both children and adults still remains poor oral hygiene. Remember this the next time you allow your baby to “so be it, don’t brush his teeth just once”!
Expert opinion
There are many reasons for the development of gingivitis in a child, and not all of them are directly related to the condition of the oral cavity.
However, treatment should begin with a visit to the dentist: he will determine the form of the disease and prescribe the correct treatment, which will effectively relieve the symptoms - that is, quickly improve the child’s well-being. After all, sometimes inflammation of the gums causes real suffering to the baby, and he cannot even explain what is bothering him! A professional dentist will immediately understand what’s going on when he sees the clinical picture of the disease, and will definitely find an approach to the most capricious young patient. After this, parents (who will also immediately feel better after their child stops experiencing pain) should fully examine the child, starting with a clinical blood test.
Perhaps the inflammation is associated with teething, the formation of roots and the formation of a bite - this is the best option, it can be conditionally classified as normal. Otherwise, you will need to consult specialists from other medical specialties - you will need to look for and treat the cause of gingivitis.
Allergic stomatitis
Allergic damage to the mucous membrane most often occurs in the form of contact stomatitis and chronic aphthous form of the disease1.
Allergens can include medications, food products, varnishes and paints that coat toys, toothpastes, mouth rinses, chewing gum, and dental metals included in braces1,2.
With allergic stomatitis in children, erosions and ulcers may appear in the mouth, but more often the matter is limited to redness and swelling of the mucous membrane1.
Treatment is avoiding contact with the allergen, rinsing or irrigating the mouth with antiseptic solutions to prevent infection. If necessary, doctors recommend taking antihistamines1,2.
Chronic recurrent aphthous stomatitis often occurs in schoolchildren and adolescents due to allergies2. In addition, its development can be provoked by diseases of the gastrointestinal tract, upper respiratory tract infections, disorders of the nervous system, and hypovitaminosis1,2.
With aphthous stomatitis in children, itching and burning first appear in the oral cavity. The mucous membrane at the site of the lesion becomes red and swollen, then an aphtha forms on it - a round or oval erosion 0.5-1 cm in diameter rising above the surrounding tissues with a red rim along the periphery and a bottom covered with a grayish-white coating. Aphthae are extremely painful, and if many of them form, they cause significant distress to the child1,2.
How many days does aphthous stomatitis last in children? With a mild course of the disease, the elements of inflammation persist for up to 5-7 days, then they heal without scar formation2 and do not appear for quite a long time. However, in severe cases, aphthae can occur constantly, and then many elements of inflammation can be found on the mucosa at different stages of development1,2.
To treat aphthous stomatitis, doctors use:
- antihistamines;
- immunomodulatory drugs;
- vitamins;
- probiotics2.
As a local therapy, it is recommended to treat the mucous membrane with drugs with analgesic, antiseptic, proteolytic (protein-breaking), anti-inflammatory and regenerating effects2.
Up to contents
Ulcers on the gums: symptoms
Upon careful examination of the oral cavity, it is not difficult to detect characteristic lesions on the gums. In the first stages, there may be only slight redness of the area on the mucous membrane, which over time acquires a whitish tint. At the site of the ulcer, inflammation and swelling of the soft tissues may occur.
Important! The fact that the baby’s oral mucosa is inflamed will be indicated by accompanying symptoms. The child becomes capricious, refuses to eat, and there may also be a slight increase in temperature.
A better idea of what an ulcer on a child's gum looks like can be obtained by taking photos of the damaged areas.
An ulcer on a child's gum. Photo.
Hexoral in the treatment of stomatitis
For local treatment of stomatitis in children, drugs from the HEXORAL® line can be used.
For irrigation of the oral cavity, the doctor may recommend aerosol HEXORAL® based on hexethidine, which has antiseptic properties7. Thanks to the fine spray, the drug is evenly distributed over the entire surface of the mucosa7. A solution of HEXORAL®8, similar in composition, is intended for rinsing the mouth. Both medications can be used to treat children 3 years of age and older.
Mint-flavored lozenges HEXORAL® TABS based on chlorhexidine and benzocaine may be suitable for boys and girls over 4 years of age9.
For patients with stomatitis over 6 years of age - HEXORAL® TABS CLASSIC based on the antiseptic amylmetacresol. The assortment includes tablets with lemon, orange, black currant, lemon and honey flavors10.
HEXORAL® TABS EXTRA may be suitable for adolescents aged 12 years and older. The lidocaine it contains can relieve even severe pain11.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Up to contents
How to treat stomatitis in children at home
As you already understood, in order to cure childhood stomatitis, antiseptics are mainly prescribed.
- Decoctions of chamomile and calendula (1 tablespoon of herbs per glass of boiling water) are well suited as natural antiseptics. The child should rinse his mouth with this solution twice a day.
- To deal with a single pustule, apply a piece of aloe leaf to it. If there are several abscesses, let the child chew a whole leaf.
- Mouth ulcers are lubricated with a one percent solution of brilliant green. This way they heal faster.
- To speed up the treatment of stomatitis in infants, it is recommended to wipe the gums with gauze soaked in a soda solution. The structure of gauze is very convenient for cleaning gums, removing harmful plaque from them.
We treat stomatitis correctly so that the disease does not return
Prevention is the best tactic to prevent disease.
To prevent stomatitis from returning in children and for the treatment to be effective, you and your baby will need to follow simple but important rules.
- The most stringent condition for the prevention of stomatitis remains personal hygiene. Stomatitis is popularly known as the “disease of dirty hands,” and for good reason. It is truly contagious: transmitted through household items and saliva.
- If your child has stomatitis, rinse his dishes with boiling water, try to reduce his contact with other children.
- It is necessary to instill in your child an understanding of how important hygiene is from an early age. To do this, first of all, set your example. Wash your hands and brush your teeth together, gradually teaching your child to do this without your reminder. Make it a tradition to come to the doctor for a checkup with the whole family.
- To prevent stomatitis in infants, it is necessary, along with bathing, to regularly wipe the mouth and rinse.
- It is also important to strengthen the child's immunity. Food full of vitamins and walks in the fresh air are indispensable helpers in this. This is also important because the child is developing: his body requires a nutritious diet and physical activity.
- React to signs of stomatitis in children in a timely manner and without panic. If you suspect that your child has stomatitis in his mouth, take him to the doctor for an examination. This way you can protect your nerves and the health of your child.
Let your children learn about stomatitis only from the article!
Literature
- Khomenko L. A. Therapeutic dentistry of children. Textbook for university / ed. 2007 – pp. 643-722.
- Ismailova G. T. Chronic recurrent aphthous stomatitis // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. — P. 124-125.
- Drobotko L.N., Strakhova S.Yu. Acute stomatitis in children // Issues of modern pediatrics. - 2010. - T. 9. - No. 2. - P. 146-149.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Toktosunova S. A., Tsepeleva A. S., Sooronbaev A. A. Prevalence and structure of the incidence of stomatitis in children // Bulletin of Science and Practice. 2022. T. 4. No. 11. — P. 91-96.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Zhumashova N. K., Yuldasheva G. I. Complex therapy of inflammatory diseases of the oral mucosa in children // Bulletin of Science and Practice. 2022. T. 5. No. 5. — P. 96-104.
- Pankrusheva T.A., Maravina I.N., Chekmareva M.S. Research on the development of the composition and technology of tablets for the treatment of stomatitis // Scientific result. Medicine and pharmacy. – T.4, No. 1, 2022. – P. 78-87.
- Instructions for medical use of the drug HEXORAL® aerosol: , .
- Instructions for medical use of the drug HEXORAL® solution: , .
- Instructions for medical use of the drug HEXORAL® TABS: , .
- Instructions for medical use of the drug HEXORAL® TABS CLASSIC: , .
- Instructions for medical use of the drug HEXORAL® TABS EXTRA: , .
Up to contents
Treatment options
Timely treatment is extremely important if an ulcer is detected on a child’s gums. Only a specialist can tell you how to treat such damage to the mucous membrane after making a diagnosis. Universal treatment methods necessarily include regular rinsing of the mouth.
For these purposes you can use:
- A solution with soda and salt. To prepare the solution, dilute furatsilin (2-3 tablets), salt (1/2 teaspoon) and soda (1/2 teaspoon) in one glass of warm boiled water.
- Herbal infusions that help improve microflora in the oral cavity and have a drying effect on ulcers.
- Solutions with vitamin B12.
Attention! Also an important component of complex treatment is the use of medications depending on the nature of the pathology. Preference in this case is given to anti-inflammatory, antiviral and analgesic compounds.
They use drugs in the form of ointments and creams, which should be used to treat damaged areas after preliminary application of antiseptic compounds.
How to treat
If a child has a white sore on his gum, you can resort to drug treatment to achieve a quick therapeutic effect. It is recommended to give preference to the following medicinal formulations:
- Metrogyl Denta is a dental gel that has an antimicrobial effect. Allowed for use in children over six years of age. The drug is prescribed for the treatment of gingivitis, periodontitis, bacterial aphthous stomatitis, inflammation of the hood under the wisdom tooth, and periodontal abscess. Sores should be treated twice a day after meals and subsequent treatment of the oral cavity with antiseptic compounds.
- Cholisal is a dental gel that has antimicrobial, anti-inflammatory and analgesic effects. This drug is perfect for children, because it has no age restrictions. The ulcers should be treated with the drug twice a day for a duration of treatment of about 10 days.
- Kamistad is a combined drug for topical use that has a local anesthetic, antimicrobial, and anti-inflammatory effect. For children over the age of three months, it is recommended to apply the composition to the sores three times a day, keeping the strip length to 5 mm.
- Chlorhexidine is an antiseptic solution used for hygienic treatment of the oral cavity. Has a detrimental effect on bacteria and other harmful microorganisms.
- Acyclovir is a drug prescribed for the treatment of formations on the oral mucosa associated with herpes infection. The medicinal composition helps accelerate the healing of formations, relieve pain, and provide an immunostimulating effect. It is recommended to treat ulcers with cream about 5 times a day for a treatment duration of 5 to 10 days.
- Benzydamine is a medicinal non-steroidal anti-inflammatory composition that has local antiseptic, analgesic and antipyretic effects. Available in the form of lozenges, creams, and solutions. As part of complex therapy, the drug is indicated for stomatitis, pharyngitis, aphthous ulcers, tonsillitis, and gingivitis. The medicine can only be used after reaching 12 years of age.
Chlorhexidine solution.