Stomatitis is a group of inflammatory processes of various origins that affect the oral mucosa. The main symptoms of stomatitis are the appearance of areas of redness and swelling of the mucous membrane, as well as blisters and erosions. These signs are accompanied by pain and burning while eating. The specification of the clinical picture depends on the type of stomatitis. The cause is determined after taking a smear from the affected area. Treatment is complex and includes symptomatic, early cleansing and antiulcer therapy. In mild forms of pathology, recovery is sufficient to maintain hygiene and sanitize the affected areas. Frequent relapses and a complicated course indicate the presence of a systemic pathology, the symptom of which is stomatitis.
Causes of stomatitis in adults
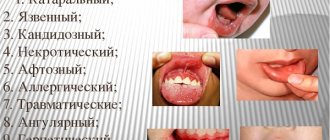
According to the etiology, stomatitis in adults occurs:
- traumatic;
- aphthous;
- catarrhal;
- ulcerative;
- candida;
- vesicular;
- bacterial (staphylococcal, streptococcal);
- angular;
- allergic.
Traumatic stomatitis develops as a result of injuries to the oral cavity caused by dentures, chips on tooth enamel, and food. After eliminating the traumatic element, the mucous membrane restores itself. Another reason for this type of pathology is the choice of hot or spicy foods. The result of such eating habits is a burn of the mucous surfaces of the mouth. Its development is provoked by:
- carious cavities with a sharp edge;
- fragments of teeth;
- burns;
- poorly installed crowns, dentures, braces;
- bad habit of biting lips, cheeks, tongue;
- malocclusion, pathological shape of teeth;
- addiction to excessively hot, cold or spicy foods;
- smoking;
- frequent consumption of foods that injure the mucous membrane (nuts, seeds).
The causes of the chronic form of aphthous stomatitis are not fully established. Presumably, the pathology is caused by staphylococci, adenoviruses, autoimmune reactions, and immune disorders.
Specific signs of aphthous stomatitis:
- the oral cavity is strewn with aphthae: round or oval ulcers;
- the center of the ulcer is covered with a gray or yellow coating, the edges are outlined by a narrow area of hyperemia.
Clinical picture of catarrhal stomatitis:
- swelling, hyperemia and painful discomfort of the oral mucosa;
- increased salivation;
- yellowish-white plaques of plaque on the mucous membrane;
- less often - slightly bleeding erosions, foul-smelling breath.
Ulcerative stomatitis occurs as a result of severe catarrhal stomatitis or independently. Sometimes considered a complication of catarrhal disease.
Candidal stomatitis (“thrush”) is a mycotic pathology caused by the hyperactivity of fungi of the genus Candida. Factors conducive to development include:
- immaturity of immunity in infancy;
- deterioration of the body's protective functions due to hematopoietic pathologies, infections, cancer, AIDS;
- old age (there is a natural decline of immune forces);
- hormonal changes during pregnancy;
- neglect of the rules of oral hygiene;
- use of dental prosthetic structures;
- drying out of the mucous membrane;
- pathologies of glucose absorption;
- taking glucocorticoid sprays;
- long-term antibiotic therapy.
Vesicular stomatitis develops as a result of contact with viruses of the genus Vesiculorus, which parasitize the body of cattle. Contamination occurs through the process of mosquito bites. Most often, this type of stomatitis affects veterinarians and farm workers.
Bacterial stomatitis occurs with a pathological increase in the population of bacteria of opportunistic microflora, usually against the background of weakened immunity.
Activation of staphylococcal and streptococcal stomatitis occurs against the background of:
- carious inflammations;
- oral injuries;
- purulent processes in periodontal pockets;
- reduction of local immunity of the oral cavity;
- non-compliance with antiseptic and aseptic rules during surgical and dental treatment.
A type of bacterial stomatitis is angular stomatitis. The cause of the pathology is not only streptococci, but also yeast-like fungi that are part of the symbiotic microflora of the human body.
Allergic stomatitis is a type of pathological autoimmune reaction. Clinical manifestations are polymorphic and include a group of dermatostomatitis, multimorphic exudative erythema and stomatitis of various etiologies (usually catarrhal or aphthous).
Types of disease
Based on the nature of the inflammatory elements formed on the mucosa, the following classification is accepted in dentistry:
- Aphthous stomatitis. Areas of inflammation look like oval and round ulcers - aphthae. This clinical form of pathology is divided into types:
- Necrotizing stomatitis. It occurs against the background of severe systemic pathologies. Characterized by the death of cells on the mucous surface in the mouth. Foci of inflammation are painful, on the 3rd-5th day of development of the pathological process they grow, and ulcers appear in their place. Aphthae heal within a month.
- Fibrinous stomatitis. The surface of aphthous ulcers is covered with a gray coating. From the moment of ulceration until the integrity of the mucous membrane is restored, 7-21 days pass. According to statistics, once every 1-3 years there is a relapse of fibrinous stomatitis.
- Scarring. Severe form of stomatitis. It begins with the formation of aphthous inflammations, growing day by day. Soon deep ulcers up to one and a half centimeters in diameter form in their place. Healing takes up to 12 weeks, and scars remain at the site of the ulcers.
- Glandular stomatitis. It affects the salivary glands, which are located throughout the oral cavity. Aphthae form at the exit of the salivary ducts. Painful when pressed.
- Deforming. The most severe variant of the pathology in its manifestations. Ulcers affect large areas of the mucous membrane and heal poorly. After the inflammatory stage, the ulcers heal with the formation of scars and scars that tighten the tissue, causing the oral cavity to become deformed.
- Catarrhal stomatitis is a process of pathology of the upper layers of the oral mucosa. Accompanied by bad breath, swelling and hyperemia of inflammation. The affected mucosal fragments are covered with plaques with a white coating, and tooth imprints remain on the gums and soft tissues of the tongue. There are severe pain, increased salivation, a slight increase in body temperature and weakness.
- Ulcerative gangrenous stomatitis. Severe form: the mucosa is affected by areas of ulceration and necrosis. The inflammatory process can destroy the entire thickness of soft tissue, down to the bone. Accompanied by severe weakness.
How to treat stomatitis?
Any treatment for stomatitis begins with a professional hygienic cleaning procedure, during which tartar and soft plaque are removed. Almost any dental clinic in Moscow provides a similar service. Teeth affected by caries are treated. The mucous membrane is treated with antiseptic rinses. During the day, rinse the mouth with a warm solution of chamomile or calendula decoction. With timely treatment, catarrhal stomatitis disappears in 5–10 days. For ulcerative or aphthous stomatitis, local treatment is combined with general treatment. In addition to professional oral hygiene, antiseptic procedures are carried out in the clinic where stomatitis is treated.
If the presence of herpetic stomatitis is suspected, additional antiviral therapy is carried out. In case of oral candidiasis, treatment is prescribed with antifungal drugs. If the cause of stomatitis is some other disease, for example, the stomach or intestines, then it is necessary to begin to treat the root cause. During the treatment process, you should definitely follow a diet limiting spicy, hot, cold, sour and rough foods. A side effect of taking medications can be a green coating on the tongue.
Symptoms of stomatitis in adults
Aphthous stomatitis. At the beginning, signs of general intoxication of the body and malaise, hyperthermia, soreness of the mucous membrane, which soon becomes covered with aphthous ulcers, are recorded. During the healing process, canker sores become scarred and leave scars.
Herpetic stomatitis. When the oral cavity is infected with herpetic virus type 1-2, there is a high risk of developing acute herpetic stomatitis. Typically, the rapid beginning of the formation of the clinical picture: hyperthermia, pronounced signs of general intoxication of the body. During examination of the oral cavity, hyperemic, edematous mucosa with areas of bleeding gums is visible. Increased saliva secretion and bad breath may occur. A few days after the manifestation of the pathology, the mucous membrane becomes abundantly covered with small pustules and vesicles, and necrotic changes in the epithelium occur.
Catarrhal and ulcerative stomatitis. The symptom complex of these two types of pathology is similar at the beginning of the disease, but after a few days the ulcerative form is identified by specific signs: severe hyperthermia, fatigue, headache and swelling of the lymph nodes closest to the source of inflammation. Ulcerative stomatitis affects the area of ulcer formation throughout the entire depth of the tissue, catarrhal lesions are limited to the upper layer of the mucous membrane. The pain intensifies while eating, sometimes so severe that it forces you to refuse food. Symptoms develop progressively and are most noticeable in people with weakened immune systems.
Necrotizing ulcerative stomatitis, or Vincent's stomatitis, occurs as a result of the activity of symbiotic microorganisms: spindle-shaped bacteria and a type of spirochete. The main reason for the pathological activity of these microorganisms is weakened immunity. Clinical manifestations of necrotizing ulcerative stomatitis:
- scattering of ulcers and erosions in the mouth;
- low-grade fever;
- pain and bleeding when pressing on the gums;
- bad breath with a hint of rot;
- the pathological process begins from the gingival margin and spreads further.
Angular stomatitis is widely known as “jams”. This form of stomatitis is characterized by painful cracks in the corners of the mouth. A feature of angular stomatitis is that in other forms of the disease the inner surface of the oral mucosa is affected, and when jammed, the integrity of the outer mucous layer is disrupted. In addition to the seasonal decrease in immunity, among the provoking factors recorded:
- gastrointestinal diseases
- metabolic pathologies
- disturbances in the functioning of the endocrine system
- oral health problems
- long-term use of artificial hormones
- pathological growth of the streptococcus population;
- unbalanced diet;
- smoking and alcoholism;
- incorrect bite.
These factors create conditions for permanent irritation of the mucous membrane, which makes it vulnerable to erosion, attachment and the development of infections.
Allergic stomatitis, with all the polymorphism of manifestations, begins with dryness of the mucous membrane, itching sensations in the mouth and along the inner edge of the lips, the process of eating causes discomfort. The oral mucosa swells, becomes hyperemic, and in the absence of timely treatment, atrophy of the lingual papillae occurs.
Treatment of stomatitis in adults
It is important to start etiotropic treatment in a timely manner to prevent chronicization of the pathology. Therapy for stomatitis includes a set of measures:
- the symptomatic part of therapy consists of taking antipyretic drugs;
- in case of severe pain, painkillers are prescribed;
- the key stage of treatment is to find and eliminate the root cause of stomatitis: the causative agent or the underlying disease; which helps prevent relapses of the painful condition;
- local treatment involves the use of local agents with a healing and antibacterial effect;
- An important component of the treatment plan is the selection of a diet and the exclusion of products containing aggressive and irritating substances (menthol, sodium lauryl sulfate) from the regimen of regular hygienic treatment of the oral cavity.
A gentle diet includes adding soft fermented milk products, neutral vegetables and fruits, cereal porridges, lean boiled meat and low-fat broths to the diet. Tea and coffee should be avoided; it is recommended to replace them with decoctions, fruit drinks and water. Spicy, sour, hot dishes or food, parts of which can physically injure tissues affected by stomatitis, are excluded. After eating, you should rinse your mouth with water or a medicinal solution.
In cases of recontamination of ulcerated areas of the mucosa, drugs containing chlorhexidine bigluconate are used. Long-term use of these drugs has an unpleasant side effect: dark spots appear on tooth enamel and fillings, which disappear after the end of treatment.
Questions and answers
— Which doctor treats stomatitis in adults?
— The dentist deals with the treatment and prevention of stomatitis. He is also competent to diagnose the type of pathology and select an adequate therapeutic regimen. Since stomatitis in adults often acts as a symptom, consultation with another specialist is possible: a gastroenterologist, an infectious disease specialist, an endocrinologist, an allergist.
— How long does stomatitis last?
— Depending on the type and severity of stomatitis, the inflammatory process should subside within 7-10 days, and two weeks after the onset of the disease, complete recovery occurs. If alarming symptoms do not go away within the specified period, you need to contact your dentist again to find out the reasons or adjust treatment measures.
— What medicine helps with stomatitis?
— Unfortunately, a universal remedy for stomatitis is still unknown to science. Stomatitis is a group of pathologies, the causes of origin and manifestations are diverse. The development of pathology is influenced by factors such as the decline of the body’s immune forces, concomitant systemic diseases, and stress. The decision to prescribe a particular drug is made individually, depending on the clinical picture and characteristics of the body. When two different people have the same diagnosis, therapeutic measures differ.
Stomatitis and treatment at home
Treatment of stomatitis at home primarily involves the use of various herbal decoctions and infusions with antiseptic, anti-inflammatory and immunostimulating effects. For example, even doctors recommend rinsing with calendula - it has a strong antimicrobial and anti-inflammatory effect and promotes healing. Chamomile is an excellent antiseptic - it is one of the most popular remedies that is widely used in folk and official medicine.
Stomatitis is treated using folk remedies not only for rinsing, but also for oral administration. For example, rosehip decoction is a real storehouse of vitamins and other substances necessary for the human body. It improves immunity, prevents the development of inflammatory processes, and also helps destroy harmful bacteria. Despite the miraculous power of herbs, it should be remembered that candida and herpetic stomatitis will not be eliminated by such folk treatment, since fungi and viruses are not affected by antiseptic, anti-inflammatory and immune-modifying agents.
Sources
The following materials were used in preparing the article:
- Anisimova I.V., Nedoseko V.B., Lomiashvili L.M. Clinic, diagnosis and treatment of diseases of the mucous membrane of the mouth and lips. - M.: 2008. - 194 p.
- Borovsky E.V., Mashkilleyson A.L. Atlas of diseases of the mucous membrane of the oral cavity and lips // Medicine - M.: 2001. - 703 p.
- Langle R. P., Miller K. S. Atlas of oral diseases: Atlas / Translation from English, ed. L. A. Dmitrieva. - M.: GEOTAR-Media, 2008. - 224 p.
- Danilenko S. M. The most common diseases of the oral mucosa // Consilium-Provisorium. - 2001. No. 6. - With. 6.
Prevention of stomatitis
The basis for the prevention of stomatitis is compliance with the rules of oral hygiene. Brushing your teeth twice a day with an ultrasonic brush and visiting a hygienist every six months are mandatory. It is important to monitor the general condition of your teeth. Wearing braces or dentures will require special attention, as they can injure the oral mucosa.
To prevent stomatitis, it is very important to be careful about your diet. Using special tests, it is recommended to identify and exclude foods that cause allergies from the diet. You should not eat foods that have a traumatic or irritating effect on the oral mucosa: crispy, salty, hot and spicy foods. Tomato and orange juices and alcohol are not recommended. The diet must be sufficiently balanced, since a lack of vitamins and microelements can cause an attack of the disease. Remember that stomatitis is always recurrent, that is, it occurs periodically during periods of general weakening of the body.
If you have had stomatitis at least once in your life, there will always be a risk of it occurring again. Therefore, prevention comes to the fore. Avoid bad habits, stick to a diet, try not to be nervous and, of course, maintain oral hygiene!