Chronic tonsillitis is a chronic inflammation of the tonsils.
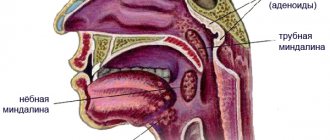
The palatine tonsils (popularly called tonsils) are an important part of the human immune system.
Bacteria, viruses, and microscopic fungi enter us with food and air. They settle on the mucous membranes, where they are picked up by a constant current of mucus, and this “river” flows in the direction of the oropharynx, just where the tonsils are located behind the palatine arches.
The palatine tonsils are like a sponge. They are dotted with gaps. When we swallow a bolus of food soaked in infected mucus, this mucus enters the lacunae of the tonsils. There, foreign microorganisms are attacked by the guard cells of the primary immune response: neutrophils and macrophages. The latter not only kill the infection, but also “cut” it into small molecular fragments, on which young cells of the secondary immune response—lymphocytes—are then “trained.” Prepared and trained lymphocytes emerge from the tonsils and “spread” throughout the mucous membranes of the pharynx and nose, forming a fairly reliable secondary specific defense.
Symptoms of the disease
Angina:
- pain in the throat when swallowing;
- increase in body temperature;
- the presence of purulent plugs on the tonsils;
- headaches;
- enlarged lymph nodes and their pain;
- a state of general weakness.
Chronic stage of tonsillitis:
- discomfort and pain when swallowing;
- presence of bad odor from the mouth;
- excessive fatigue;
- slight increase in body temperature;
- sleep disturbance;
- enlargement and tenderness in the cervical lymph nodes.
Tonsillectomy
Chronic tonsillitis can be cured. To get rid of it forever, the tonsils are removed. However, the operation is often postponed, justifying the decision by the participation of these formations in the formation of immunity.
In fact, the mass of the tonsils constitutes only 0.05% of the total mass of lymphoid tissue, which mediates the systemic immune response3. The functions of protecting the respiratory tract from microorganisms penetrating through the mouth and nose are taken over by other tonsils3: paired tubal and unpaired lingual and pharyngeal tonsils. Moreover, the tonsils affected by infection lose their functions1 and turn into a focus of infection that can cause serious illnesses.
The operation is performed in a hospital setting. It involves complete bilateral removal of the tonsils along with the surrounding capsule and often does not require general anesthesia5.
Contraindications to it are:
- blood diseases accompanied by a decrease in blood clotting;
- severe cardiovascular, renal, hepatic and pulmonary insufficiency;
- severe course of hypertension;
- heart problems such as cardiosclerosis with angina pectoris5.
The operation should be postponed if it is necessary to treat acute respiratory viral infections and other infections and concomitant diseases, the exacerbation of which is possible as a result of surgical intervention.
Up to contents
Possible complications of tonsillitis
- Rheumatism is the most dangerous complication, which, in turn, can affect the joints and lead to heart disease.
- Pyelonephritis.
- Peritonsillitis, peritonsillar abscess.
Causes of sore throat:
- various viruses;
- bacteria;
- hypothermia of the body;
- decreased immune system functions;
- tonsil injury;
- violation of nasal breathing;
- various inflammations in the oral cavity.
Causes of chronic tonsillitis:
- frequent sore throats and ARVI;
- diseases of teeth and gums;
- nasal breathing disorder.
- weakened immune system;
- presence of allergies.
Chronic tonsillitis: how to live with it?
There is probably no person in the world who has not suffered from a sore throat at least once in his life.
Sore throat (acute tonsillitis)
is an acute general infectious disease with local inflammation of the tonsils.
Chronic tonsillitis is a general infectious-allergic disease with local manifestations in the form of persistent inflammation of the tonsils.
How does chronic inflammation of the tonsils occur?
The main causative agents of chronic tonsillitis are streptococcus bacteria. Less common are other types of bacteria, fungi and intracellular parasites, as well as their various combinations. The participation of viruses in the development of chronic tonsillitis comes down to a decrease in local immunity in the palatine tonsils, which facilitates the penetration and reproduction of bacteria into them.
The occurrence of chronic inflammation is based on a violation of local immunity in the palatine tonsils. With a decrease in local protection, microorganisms in the palatine tonsils multiply, their waste products damage the tissue of the tonsils, and dead cells and microorganisms are exfoliated into peculiar crevices (crypts) and lacunae of the tonsils. The random cells clog the lumen of the lacunae of the tonsils, scarring occurs in them, and self-cleaning becomes difficult. As a result of prolonged inflammation, pathological immune reactions occur. The immune system begins to produce specific proteins and their compounds (antibodies and immune complexes), which are aimed not at destroying pathogens, but against the body’s own tissues. Violation of the barrier function of the palatine tonsils leads to the absorption of toxic waste products of microorganisms into the bloodstream, distribution throughout the body and the occurrence of general intoxication (increased body temperature, increased fatigue, decreased appetite).
Thus, local inflammation of the tonsils becomes general. The heart, kidneys, joints and lungs are most often affected.
What factors contribute to the occurrence of chronic tonsillitis?
Any general factors that weaken the body’s resistance (stability) can contribute to chronic inflammation: hypothermia, overexertion, malnutrition, lack of vitamins, unfavorable environmental conditions, frequent viral diseases, various congenital and acquired immunodeficiencies, diabetes mellitus and other chronic diseases.
Chronic diseases of the nasal cavity, paranasal sinuses and nasopharynx can lead to chronic tonsillitis. Excluding the nasal cavity and paranasal sinuses from the act of breathing, where humidification, warming and purification of the air occurs, leads to the fact that unprepared air saturated with microbes enters through the mouth onto the palatine tonsils. In addition, mucus or pus flowing down the back wall of the pharynx during chronic inflammatory processes in the overlying parts of the respiratory system leads to their contact infection.
Some diseases of the dental system (caries, pulpitis) can affect the occurrence of inflammation in the palatine tonsils.
Diseases of the digestive system can contribute to the appearance of chronic tonsillitis. For example, with gastroesophageal reflux disease (GERD), acidic or alkaline gastric contents are refluxed from the duodenum first into the esophagus, and then into the mouth and laryngopharynx. The aggressive contents of the stomach and duodenum damage the surface layer of cells of the palatine tonsils and promote the penetration of microorganisms into them.
What are the symptoms of chronic tonsillitis?
If the barrier function of the palatine tonsils is preserved, the disease is characterized only by local symptoms, which do not manifest themselves in any way and can only be detected by an ENT doctor. There may be bad breath associated with blockage of the lacunae of the palatine tonsils with pathological contents (pus or caseous masses), as well as discomfort when swallowing and sore throat.
When the barrier function of the tonsils is impaired, frequent sore throats and peritonsillar abscesses occur, when inflammation passes from the palatine tonsils to the surrounding tissue, followed by purulent melting. Absorbed from the tonsils into the blood, toxins cause general malaise, increased body temperature, periodic joint pain, loss of appetite and weakness. Functional disorders of the cardiovascular system may occur, which are manifested by palpitations, heart rhythm disturbances and changes in the ECG. In some cases, chronic tonsillitis develops rheumatism, arthritis (inflammation of the joints), nephritis (inflammation of the kidneys), and sepsis.
Microorganisms and their metabolic products, having antigenic properties, lead to general allergization of the human body.
It should be noted that there are forms of chronic tonsillitis in which tonsillitis does not occur, but damage to other internal organs already occurs.
A source of chronic infection in the tonsils affects the functioning of all organs and systems and in all cases aggravates any diseases occurring in the body.
What treatment methods exist for chronic inflammation of the tonsils?
In compensated forms of tonsillitis, when the process is limited only to damage to the palatine tonsils, and their barrier function is preserved, conservative treatment is carried out.
Treatment must begin with the elimination of predisposing factors: elimination of diseases of the nasal cavity, nasopharynx, treatment of affected teeth, gastroesophageal reflux disease and others.
Twice a year, the lacunae of the tonsils are washed with various antimicrobial drugs. Currently, treatment is used with Tonsillor devices, laser and cryotherapy, as well as photodynamic therapy.
If there is no effect from conservative treatment, and also when the tonsils cease to perform their functions and represent a source of infection for the body, they are removed - tonsillectomy. For surgical treatment, various radio wave and plasma scalpels are used, which can reduce blood loss during surgery.
Clinical experience and scientific data indicate the absence of serious general and local negative consequences for the body after removal of the tonsils.
THERE ARE CONTRAINDICATIONS, SPECIALIST CONSULTATION IS REQUIRED
Treatment of tonsillitis in the clinic
To prescribe high-quality and effective ENT treatment, the doctor must accurately determine the nature of the inflammation (acute, chronic), its type (with or without purulent content), and the type of pathogen (virus, fungus). If tonsillitis is chronic, it is important to determine whether conservative treatment will be sufficient or surgery is indicated.
Conservative treatment involves washing the tonsils, removing plugs with pus, gargling, drinking plenty of warm fluids, and taking anti-inflammatory drugs.
In no case should you self-medicate - it is better to consult a specialist who, after an examination, will prescribe you the correct treatment.
What tests need to be taken for tonsillitis?
In order to determine the pathogen and determine further treatment, the doctor may prescribe a number of laboratory tests to the patient, for example:
- a smear from the tonsils, arches and back of the throat to identify bacteria and their resistance to various groups of antibiotics, but such a study may take several days
- rapid test for the detection of group A beta-hemolytic streptococcus to determine streptococcal tonsillitis5
- a general blood test with a leukocyte formula, which pays attention to elements that reflect inflammation and the immune response to the disease. Increased band neutrophils, leukocytes, increased ESR, decreased lymphocytes
- CRP (C-reactive protein - a marker of inflammation) is the most sensitive protein responsible for inflammation in the body
A little anatomy and physiology
The palatine tonsils are located on the side walls of the pharynx and are shaped like large almond kernels. The second name - “tonsils” - tonsils received due to their resemblance to acorns, which are called “glandulae” in Latin. Since the Latin word for tonsils is “tonsilla,” their inflammation is called tonsillitis.
The palatine tonsils belong to the organs of the immune system and are small accumulations of lymphoid tissue 2. The part of the tonsils protruding into the pharynx has depressions (lacunae), in the walls of which there are numerous slit-like pockets (crypts)1. The surface of the crypts is the “working area” of the tonsils. Basic physiological processes take place here: immune cells, phagocytes, absorb microbes that have penetrated the tonsils, “study” them, send the received information to higher departments of the immune system, and then kill the infection1. If the microbes are very aggressive and there are a lot of them, and the immune system is weakened, an infectious inflammation of the tonsils develops - tonsillitis.
Up to contents
Literature
- D.L. Yalymova, V.V. Vishnyakov, V.N. Talalaev, V.N. Kostyuk. Chronic tonsillitis: diagnosis, classification, treatment. Directory of a polyclinic doctor. 2014; 08: p. 29-31.
- Chronic tonsillitis. Directory of a polyclinic doctor. 2014; 09: p. 43.
- G.S. Maltseva. Chronic tonsillitis: current issues (clinical lecture). Consilium Medicum. 2011; 11: p. 32-38.
- A.I. Kryukov, Yu.V. Better. Sore throat and chronic tonsillitis: the problem of choosing an antibacterial drug in an outpatient setting. Directory of a polyclinic doctor. 2007; 04: p. 42-44.
- Instructions for use of the drug HEXORAL® solution.
Up to contents
Tonsilloliths and what they look like
Repeated episodes of infection can cause fibrosis in the lacunae of the tonsils, leading to the accumulation of epithelial debris. These remains calcify and turn into soft or rather hard “pebbles” - tonsilloliths (from tonsillae - tonsil and litos - stone). White, grayish, yellowish, they smell unpleasant, cause a sensation of a foreign body, mild pain, and coughing. Sometimes they are released suddenly - with a sharp cough, loud scream, after a hot meal, when rinsing the mouth and throat. Treatment usually involves removal of the tonsils by an ENT doctor (curettage) [3]