From this article you will learn:
- herpes virus - types, symptoms,
- reasons for repeated outbreaks,
- how to treat herpes - the best remedies,
- How effective is the vaccination (Vitagerpavac vaccine).
Herpes is a viral disease in which characteristic eruptions of fluid-filled blisters (vesicles) appear on the skin and mucous membranes. But within 2-3 days the blisters burst with the formation of ulcerations, which, if localized on the skin or red border of the lips, become covered with crusts, and if on the mucous membrane, then with a yellowish fibrinous film. There is a whole family of herpeviruses, but people usually have to deal with the “herpes simplex virus” - types HSV-1 or HSV-2.
It is these types of herpes that are responsible for the appearance of rashes - on the skin of the face, lips, oral mucosa, and they are also the cause of genital herpes. It should be noted that if previously the herpes virus HSV-2 was associated only with the development of genital herpes, now it also causes herpes on the face, lips and oral mucosa - in approximately 10% of patients. Herpes type HSV-2 is more pathogenic (than HSV-1), and such patients always experience both more severe clinical manifestations and a higher frequency of relapses.
Herpes: photo
The herpes simplex virus is clinically manifested by the formation of a group of crowded blisters located on an inflamed base (skin or mucous membrane). The bubbles are first filled with transparent contents, which quickly become cloudy. If you have herpes, treatment must be started before the herpetic vesicles open. Otherwise, not only the ointment for herpes, but also the best tablets for herpes will no longer allow any noticeable acceleration of healing.
What does herpes look like?
Important: the appearance of herpetic rashes is almost always preceded by the appearance of itching or burning in this area, or a feeling of tissue swelling. It is very important to teach the patient to “catch” these first symptoms, because if you start treatment for herpes already at this stage (during the prodromal period of the disease), the number and size of the herpetic blisters that subsequently form will be significantly smaller. And besides, the healing of erosions will occur much faster.
In rare cases, early initiation of therapy can even prevent the appearance of herpetic blisters (for example, when using combination drugs containing “5% acyclovir + 1% hydrocortisone”). Faster healing can also be achieved if treatment for herpes is started in the first 12 hours - from the moment the first herpetic blisters appear. You must understand that the later treatment begins, the lower its effectiveness will be. After opening the vesicles, treatment with antiviral ointments and tablets will no longer affect the healing rate, although it will still be indicated for patients with severe herpes.
Myth: Herpes only affects the skin
This is not true at all. The herpes simplex virus is integrated into the genome of nerve cells, so rashes occur at the sites of nerve endings and are accompanied by severe pain. Theoretically, herpes can appear anywhere there is nervous tissue, which means in almost any organ. With a decrease in general and local immunity, a herpetic rash can develop in the mucous membrane of the mouth and larynx, cornea and conjunctiva of the eye, lymph nodes, genitals, intestines, liver, kidneys, lungs.
Herpes virus (how does infection occur) –
Initially, children are born with immunity to the herpes virus - thanks to the antibodies that each child receives from the mother (even during pregnancy). However, gradually the number of antibodies decreases, and usually in the period from 6 months to 3 years maximum, the child develops a primary herpes infection. It usually occurs in the form of primary herpetic gingivostomatitis. And in the future, the herpes virus remains in the body for life, periodically exacerbating.
How is herpes transmitted?
The best remedy for herpes is certainly its prevention, but below we will also talk about special ointments and tablets. You should know that contact is the main route for transmission of herpes infection; Airborne transmission is more rare. Contact transmission means that infection with the herpes virus occurs:
- through kisses and touches,
- when you use personal items that have been in contact with a person with herpes or simply a “carrier”,
- for example, you dried yourself with someone else's towel,
- for example, you tasted your child's food with his spoon,
- for example, you eat with someone from the same plate, etc.
The most contagious are people who have clinical manifestations of herpes - we are talking about whole or newly opened herpetic vesicles. Keep in mind that the risk of infection does not disappear once crusts form, but only decreases slightly. Modern research shows that infection with herpes is possible even from a clinically completely healthy person.
Important: in approximately 10% of people, the herpes virus is constantly detected in the saliva (even against the background of the complete absence of any symptoms of herpes).
What causes relapses of herpes -
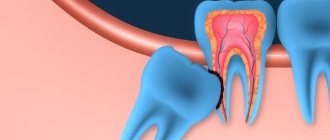
After the initial infection, the herpes virus penetrates the nerve cells, then it spreads along the nerve trunks, ultimately ending up in the nerve ganglia. There it remains for life - in the form of a “dormant infection”.
Under the influence of certain triggering factors, the virus is activated and again moves along the nerve trunks to the surfaces of the skin and/or mucous membranes - where it causes the formation of herpetic vesicles (vesicles). Relapses can occur 1 or 2 times a year, but sometimes much more often, which ultimately depends on the state of your immune system and nervous system.
Factors that cause recurrence of herpes –
- contact with a person with clinical manifestations of herpes,
- decreased immunity due to influenza or ARVI,
- immunodeficiency states,
- hypothermia, dehydration,
- physical fatigue and emotional stress,
- cuts and scratches on the skin, for example after shaving,
- after a visit to the dentist (due to the fact that when the mouth is opened wide for a long time, cracks form in the corners of the mouth),
- after invasive cosmetic procedures,
- during menstruation in women,
- prolonged exposure to the sun.
You should know it
Test yourself
If rashes appear no more than 4-5 times a year and only on the lips, there is nothing to worry about. This is unpleasant; most likely, there are no systemic failures in the body. It is only important to learn how to quickly relieve exacerbations. Antiviral ointments and creams, which are widely sold, will help with this.
SOS
If exacerbations occur more than 5 times a year, rashes appear not only on the lips, but also on other parts of the body, be sure to undergo an immunological examination. In older people, frequent relapses of herpes may indicate the development of tumor processes accompanied by immunodeficiency.
Important
Peanuts, chocolate, raisins, and beer are harmful to people with herpes. Dairy products, meat, eggs, fish, legumes, and boiled potatoes are healthy. Eat as many fruits and vegetables as possible. Drink 1–1.5 liters of liquid per day.
Article on the topic
How to get rid of “colds” on your lips Avoid fatty foods. Reduce the amount of sugar, sugary carbonated drinks and caffeine-containing drinks. Reduce the amount of salt and wheat bread.
Patient Reminder
You can't kiss anyone while you're sick.
The sick person must have personal dishes, soap, towels, bedding, and all personal hygiene items.
During a herpes outbreak, forget about going to the pool, sauna, or bathhouse.
Refrain from intimate contact. Unless, of course, you want your lover to also suffer from itchy “decorations” on his body. Do not despair: in the stage of remission (attenuation of the disease), you can safely indulge in the joys of love.
Apply the cream to treat rashes on your lips not with your fingers, but with cosmetic sticks.
Herpes symptoms –
A striking hallmark of herpes is the appearance of a group of blisters filled with liquid. However, before they erupt, there is always a period (lasting from several hours to 1 day) when there are no clinical manifestations yet, but the virus has already been activated. As a rule, during this period you may feel itching, burning or swelling of the tissue in the area where herpetic blisters should appear in the future (24stoma.ru). Further symptoms depend on the location of the rash...
- Herpes on the lips (Fig. 7-9) - the red border of the lips and the skin around the mouth are the most common localization of herpes. Herpes of this localization is called “labial”. The blisters that appear on the skin and red border of the lips burst and dry out after 2-3 days, and the affected surface becomes covered with crusts that persist for a period of 7 to 10 days. Under no circumstances should the crusts be peeled off, because... Removing the crusts can also lead to a new outbreak of herpes.
Labial herpes: photoFor detailed information about the most effective treatment regimens for herpes of this localization, read the article: “How to quickly get rid of herpes on the lip”
- Herpes on the skin of the face – foci of herpes can appear on any part of the facial skin, which is usually associated with a violation of the integrity of the skin (scratches, cuts, abrasions). Typical localization is herpes on the cheeks and nose, earlobes, chin, and forehead. The skin around the eyes can also be affected, but we have identified this type of lesion in a separate column.
Depending on the extent of skin damage and the severity of clinical manifestations, either a skin cream with an antiviral effect or a cream in combination with tableted antiviral drugs may be prescribed. You can see a detailed review of treatment drugs at the end of the article. - Herpes in the mouth (Fig. 10-11) - herpes of the tongue, gums and other areas of the oral mucosa most often occurs in children, rarely in adults. This disease is called herpetic stomatitis. After the bubbles on the mucous membrane burst, bright red erosions form in their place, which are quickly covered with a whitish-yellow fibrinous coating. Along the perimeter of the lesions there is always a bright red rim of inflamed mucous membrane.
In children, herpetic stomatitis is often accompanied by gingivitis. In this case (in addition to multiple blisters and erosions in some area of the oral mucosa), you can see bright red inflamed gums.
- Ophthalmoherpes
(Fig. 12-13) – the herpes simplex virus can spread to one or both eyes. Most often, this happens when you introduce the virus with unwashed hands that have recently touched areas of the skin affected by herpes. You can spread the virus simply by using a regular face towel. Most often, the virus infects the upper layer of the cornea, causing herpetic keratitis. If rashes may appear on the skin of the eyelids, this option is called “herpetic blepharitis.”Symptoms: pain, blurred vision, sensitivity to light in one eye (if one eye is affected), feeling of “sand in the eyes.” Eye herpes is very dangerous, and untimely or improper treatment can lead not only to dryness of the cornea and the appearance of scars on it, but also to deterioration of vision, constant pain, and even blindness and loss of the eye.
General symptoms of herpes - primary herpes infection can occur with symptoms similar to influenza or ARVI (fever, muscle pain and even enlarged submandibular lymph nodes). But such acute symptoms are observed in only 10% of all patients. With repeated outbreaks, the general condition of the body is usually not disturbed.
Myth: Condoms protect against genital herpes
A condom really reduces the risk of infection, so its use is necessary during an exacerbation of the disease, in the presence of inflammatory changes on the mucous membranes and skin of the genital organs.
Article on the topic
What folk methods will help get rid of fever on the lip? But, unfortunately, he does not give a 100% guarantee. Transmission of the virus can occur through areas of the body not covered by a condom. Therefore, if possible, you should abstain from sexual activity during the period of exacerbation of the disease.
How to treat herpes in adults (medicines) –
Very often, patients ask questions about how to cure herpes forever. Unfortunately, at the moment medicine does not have the ability to achieve complete removal of the herpes virus from the body. However, modern antiviral agents (ointments and tablets) can effectively block the replication of the virus, especially when it comes to the herpes simplex virus (types HSV-1 and HSV-2). It can be much more difficult to cure herpes on the body, which is referred to as “shingles” or “herpes zoster”.
Modern antiviral tablets and ointments for herpes can significantly reduce the severity of herpes infection, speed up healing, and also reduce the frequency of relapses. There is also a domestic vaccine against the herpes simplex virus (types HSV-1 and HSV-2) called “Vitagerpavak”, which can reduce the frequency of repeated outbreaks of herpes infection by several times. Below we will tell you about the best remedy for herpes - both among means for external use and among tablet preparations.
But in order for herpes treatment to be as effective as possible, you must strictly follow the following rules:
- Herpes therapy will show good effectiveness if it is started no later than 12 hours from the moment the first herpetic rash appears. Keep in mind that the later treatment is started, the less effective even the best herpes medications will be.
- The maximum effectiveness will be shown by therapy that is started in the prodromal period (i.e., when the actual herpetic blisters have not yet appeared, but the patient already feels itching, burning or swelling of the tissue in this area). If treatment begins during this period, then the number and size of herpetic blisters formed in the future will be significantly smaller, and in this case, complete healing can be achieved in just 4-5 days.
- Remember that if you start treatment later than 48 hours , or after the herpetic blisters have opened, such therapy will not noticeably affect the speed of recovery (healing of lesions). However, in patients with severe and frequent relapses, such therapy can avoid complications.
Treatment methods for herpes
Treatment of herpes is aimed at suppressing viral activity, as well as increasing immunity. Oral and topical medications may be prescribed.
The selection of drugs is carried out by a doctor depending on the type of disease (type of infection), as well as on the location of the lesion.
It is impossible to completely eliminate the herpes virus from the body. That is why it is important to always maintain the body’s defenses at a sufficiently high level, and also to prevent re-entry of the virus.
Prevention of herpes
If a person close to you has manifestations of herpes (“a cold has popped up on the lip”), try to ensure compliance with the following hygiene rules:
- use an individual towel and personal hygiene products (soap, toothbrush, etc.);
- be careful with cosmetics: do not use lipstick of a sick person;
- If you have genital herpes, avoid sexual intercourse.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Choosing an ointment for herpes -
If you have herpes, treatment in adults and children is most often carried out with one of the external agents containing 5% Acyclovir (an antiviral agent effective against the herpes virus). Preparations based on acyclovir: Acyclovir cream 5% (Russia), Acyclovir ointment 5% (Russia), Acyclovir-Hexal cream (Germany), Acyclovir-Sandoz cream (Switzerland), as well as original drugs with acyclovir - a line of branded products Zovirax (UK).
Zovirax cream: the original drug of acyclovir
Herpes cream or ointment with acyclovir should be applied to the lesion and the skin around it at least 5 times a day (but better every 2 hours while you are awake). The duration of therapy is usually 5 days, but in case of severe herpetic lesions, the duration of use can be increased to 7-10 days. It should be noted that the cream form is more preferable to the ointment, because from the ointment substance, the active substances penetrate the skin much worse.
It is worth paying attention to the composition, for example, the effective concentration of acyclovir is exactly 5% (although in pharmacies you can also find products with a 3% concentration). In addition, the composition should preferably contain propylene glycol and/or cetomacrogol, which increase the penetration of acyclovir molecules through the surface layers of the skin. This is important because Acyclovir itself penetrates quite poorly through the epidermis of the skin and the resulting crusts.
For women, it may be important to be able to apply cosmetics on top of the absorbed cream. In this case, you should choose a cream that contains dimethicone (silicone). Today, dimethicone in combination with propylene glycol and cetomacrogol is found in the following products - Zovirax cream, Zovirax Active-Duo cream, Acyclovir-Sandoz cream.
The best remedy for herpes with acyclovir is
Today, the best drug for external use against herpes is Zovirax Duo-Active cream, which contains a combination of 5% acyclovir and 1% hydrocortisone. Acyclovir blocks the multiplication of the virus, and hydrocortisone reduces inflammation and swelling. Moreover, if the use of the cream begins even before the appearance of herpetic blisters, then hydrocortisone sometimes makes it possible to prevent their formation altogether. But if bubbles do form, their number and size will be smaller, which in itself will significantly speed up healing.
Disadvantages of acyclovir-based drugs - acyclovir is an outdated drug, but in principle it works well for most patients (with some exceptions). For example, in patients with good immunity, resistance of the herpes virus to acyclovir occurs on average in only 3% of cases, which is quite small. However, the problem is in patients with weakened immune systems + frequent courses of acyclovir use in the past - in such groups of patients, resistance to acyclovir can be observed in 10 to 27% of cases.
In addition, acyclovir molecules have a very low tropism for the herpes virus, which means that acyclovir usually simply does not find a certain percentage of viral particles in cells (for example, drugs based on penciclovir / famciclovir have a much higher tropism in the virus). In addition, acyclovir molecules tend to penetrate poorly through the skin, as well as through the resulting crusts (to the site of virus reproduction). In order to somehow reduce this problem, some manufacturers add propylene glycol and cetomacrogol to external products containing acyclovir.
Alternative external remedies for herpes -
First of all, this is the Fenistil-Pentivir cream, which contains the antiviral component Penciclovir. Compared to acyclovir, penciclovir is several times more effective (including due to the significantly greater tropism of penciclovir for the herpes virus, and due to better penetration into cells affected by the virus). It should also be noted that the resistance of the herpes virus to penciclovir is extremely low - it is no more than 0.2%.
The drug is applied to the lesion every 2 hours (8 times a day), but the course of use is usually only 4 days. Such a short course is due to the fact that after the last application of the cream, the clinically active concentration of penciclovir will remain in the cells for about 2 more days (i.e., the therapeutic effect after a 4-day course will last about 6 days). Clinical studies have also found that repeated outbreaks of herpes occur less frequently when using Fenistil-pencivir than when using other drugs. However, in recent months this drug has disappeared from Russian pharmacies, most likely due to the re-registration procedure.
We have already said above that patients with weakened immune systems often develop resistance of the herpes virus to acyclovir. What should such patients do? International recommendations in this case speak of the need to use courses of famciclovir in tablets - these are drugs such as Favirox or Famvir. Tablet preparations based on valacyclovir (if resistance to acyclovir is suspected) does not make sense to use, because valacyclovir is a precursor to acyclovir. The latter means that if there is resistance to acyclovir, there will be resistance to valacyclovir.
Cream Devirs for herpes –
Maybe there are some other topical products that would be effective against herpes and do not contain acyclovir? In pharmacies you can find such a prescription drug - Devirs cream (manufactured by Vertex, Russia), containing the antiviral component ribavirin. According to the instructions, this drug can be used in patients over 18 years of age - for genital herpes, for the treatment of labial herpes, herpes localized on the face and body.
Unfortunately, there are very few clinical studies on the effectiveness of local ribavirin-based products, and all of them, in our opinion, have a rather weak degree of evidence. Getting acquainted with the studies, we noticed that this drug was very rarely used in studies in the form of monotherapy (usually it was combined with either oral ribavirin or oral acyclovir), which already indicates the rather weak effectiveness of the cream. Therefore, our editors cannot recommend this drug for widespread use, especially for the treatment of herpes lips and small lesions on the face. But the drug may well be used as part of complex therapy, for example, for genital herpes.
How does recurrent herpes on the lips manifest?
Recurrent herpes on the lips is recorded in 50-70% of patients who previously suffered from an asymptomatic or clinically pronounced primary form of the disease. Relapse is the repeated appearance of typical rashes in the same place - at the site of primary infection (“Locus minoris”).
Fact The state of immunity determines the likelihood of development and severity of the disease, the frequency of subsequent relapses of herpes on the lips.
Factors contributing to the development of relapse are:
- hypothermia, overheating, hyperinsolation (including in a solarium),
- neuro-emotional stress,
- medical and cosmetic procedures (tattoo), surgical operations,
- somatic, endocrine, oncological, infectious diseases (frequent ARVI),
- hormonal changes
- decreased immunity, primary or acquired (secondary),
- poor nutrition,
- long-term use of medications (hormones, chemotherapy, antibiotics, including antivirals, cytostatics),
- active sexual life (for example, with frequent changes of sexual partners or orogenital contacts).
Herpes on the lips manifests itself symptomatically during relapses. Relapse of the disease occurs against the background of circulating antiviral antibodies and therefore proceeds more easily compared to primary herpes. Subjective sensations and intoxication may be mild or absent altogether.
Fact The clinical picture of recurrent herpes on the lips resembles that of primary herpes.
The duration of relapse is less than the duration of primary herpes on the lips and is 7–10 days.
It should be noted that along with the typical manifestation, herpes on the lips can be asymptomatic, with symptoms that go unnoticed, as well as atypical or abortive.
Atypical forms of herpes on the lips may be caused by a change in the development cycle of herpetic elements in the lesion. In atypical forms of recurrent herpes on the lips, as a rule, one of the stages of development of the process in the lesion (erythema, formation of single or multiple blisters) or one of the components of inflammation (swelling, hemorrhage, necrosis) or subjective symptoms (itching) predominates. For example, the edematous form of herpes on the lips differs from the typical form by a sharp swelling of the subcutaneous tissue and hyperemia of the skin (usually on the lips); vesicles may be completely absent.
The hemorrhagic form of herpes on the lips is characterized by the appearance of blisters not with transparent, but hemorrhagic contents, and the subsequent development of ulcerations.
The abortive form of herpes on the lips occurs in patients who have previously received antiviral treatment and/or vaccine therapy. The lesion in an abortive course goes past some of the stages characteristic of the typical form and may appear as an itchy spot or papule.
The subclinical form of recurrent herpes on the lips is detected during a virological examination of sexual partners with any sexually transmitted disease, or during an examination of married couples. Symptoms in this form are mild or completely absent. Patients with a subclinical form of herpes on the lips are a source of infection for their loved ones, children, and sexual partners.
Choosing tablets for herpes -
Herpes treatment in adults: drugs in tablets
- Acyclovir,
- Valaciclovir,
- Famciclovir.
Below we will compare the effectiveness of these antiviral tablets against the herpes simplex virus. It should be noted that Acyclovir tablets are approved for use from 0 years of age, and the drugs “Valacyclovir” and “Famciclovir” - only from 12 years of age. All these drugs are available only with a doctor's prescription.
Acyclovir in tablets of 200 and 400 mg –
Tablet acyclovir has the same disadvantages as creams: low tropism for the virus (i.e., acyclovir molecules do not find viral particles well); in patients with poor immunity + frequent courses of acyclovir use in the past - in 10-27% of cases the herpes virus may be resistant to acyclovir; plus low oral bioavailability. Pros: no age-related contraindications, affordable price, fairly few side effects.
We recommend choosing the original drug with acyclovir - Zovirax 200 mg tablets (instructions for use, see PDF). Moreover, its cost is not much higher than that of Russian generics.
Examples of drugs with acyclovir -
Acyclovir tablets certainly work, especially when it comes to patients with good immunity and rare relapses of herpes. If you have a weakened immune system, if you have taken acyclovir too often in the past, if you decide to start taking the drug more than 24-48 hours after the onset of herpetic rashes, acyclovir will not be particularly effective. In this case, it is better for you to immediately start taking the drug Famciclovir, which works better even at later dates of initiation of therapy, as well as in patients with immunodeficiency conditions.
The regimen of use - if you look at the official instructions, the standard regimen for adults and children over 2 years old - is to take acyclovir 200 mg 5 times a day (for 5 days). A single dosage of 400 mg is recommended in the official instructions - either only for severe herpes infection, or in patients with weakened immune systems. However, most clinical studies (source) show that a dosage of 200 mg has virtually no effect on either the duration of symptoms or the healing time of herpes.
Studies have shown that only 400 mg (respectively, 5 times a day, for 5 days) is an effective single dose. In children under 2 years of age, the dosage is reduced by exactly 2 times - from the adult dosage. In case of severe herpes infection, taking the drug can be extended to 7-10 days. By the way, abroad, at the moment, acyclovir is practically not used for chronic recurrent herpes, giving preference to valacyclovir and famciclovir.
Valacyclovir (Valtrex) tablets –
We have already said above that tableted acyclovir has poor bioavailability, i.e. only about 10-20% of its amount is absorbed in the intestine, which makes it difficult to achieve high concentrations of acyclovir in tissues. This problem is solved by Valacyclovir, which has a bioavailability of 50%. Valaciclovir is a precursor to acyclovir (i.e., it is converted to acyclovir once it enters the bloodstream). Taking tablets with valacyclovir allows you to create a concentration of acyclovir in tissues that can be achieved with traditional acyclovir - only through intravenous infusions of the latter.
The drug Valtrex is the original drug of Valaciclovir (we recommend this drug), but there are also a large number of cheaper generics. The cost of the original drug “Valtrex” (UK) is from 1350 rubles for 10 tablets. 500 mg each. There is a good Bulgarian generic “Valvir” - it costs from 750 rubles for a package of 10 tablets. 500 mg each. The cost of the Russian “Valacyclovir-Akos” will be from 450 rubles (for a package of 10 tablets of 500 mg).
Regimen: There is a short 1-day treatment regimen. Clinical studies have shown that taking high dosages of the drug for 1 day was the most effective for the treatment of herpes on the lips and facial skin, as well as herpetic stomatitis. In this case, the dosage regimen is 2000 mg 2 times a day, with an interval of 12 hours (1 day in total). But it should be noted that such a short regimen will be effective only if treatment begins no later than 12 hours from the moment the herpetic eruptions appear, and also in patients with satisfactory or good immunity.
If more than 12 hours have passed since the appearance of the rash, and also if you have a weakened immune system, it is optimal to use the standard treatment regimen of 500 mg 2 times a day for 3-5 days (for severe herpes infection - up to 10 days). When choosing a drug, keep in mind that if your herpes virus is resistant to acyclovir, taking valacyclovir will also be ineffective.
Famciclovir tablets (Favirox, Famvir) –
Famciclovir products are the most modern and effective tablets for herpes. Above we told you about the cream “Fenistil-pencivir” (based on penciclovir), which is used on the skin of the face and the red border of the lips. So, drugs with famciclovir are tablet analogues of penciclovir. Most often in pharmacies you can find drugs with famciclovir - under the trade names “Favirox” or “Famvir”.
The advantage of famciclovir drugs like Favirox is their rapid antiviral effect due to maximum bioavailability (for famciclovir it is about 74%, for example, for valacyclovir it is only 54%, and for acyclovir only 10-20%). Therefore, a package of three 500 mg tablets is enough for a short 1-day course of therapy to relieve the manifestations of herpes on the lip. Read more about this application scheme below.
→ Favirox instructions for use (view PDF)
Regimen for using famciclovir - there is a short 1-day treatment regimen: either take 1500 mg once, or 750 mg 2 times a day (with a 12-hour interval between doses) - our experience suggests that the second option is still better. This 1-day regimen is effective only if you start taking the drug before 12 hours from the moment the herpetic rash appears, and also if the patient’s immunity is normal. In case of weakened immunity, and/or if treatment is started later than 12 hours from the moment of the appearance of herpetic eruptions, the standard dosage regimen should be used.
The standard regimen according to the instructions is 250 mg 2 times a day for 5 days (however, in severe cases of herpes infection, dosage can be extended to 7-10 days). Here I would like to add that numerous clinical studies show the weak effectiveness of this standard regimen - especially in patients with poor immune system conditions. Studies have shown that the effectiveness of therapy increases significantly when famciclovir is prescribed in higher dosages. In patients with good immunity, a more effective regimen will be 500 mg 2 times a day (for 5 days). In immunocompromised patients - 500 mg 3 times a day (for 7 days).
Important: once again we draw your attention to the fact that short 1-day treatment regimens for herpes in adults (herpes on the lips and skin around the mouth, on the face) work well only if the following conditions are met. Firstly, only if you start taking medications no later than 12 hours from the moment the herpetic rash appears. Secondly, if you have a satisfactory or good immune system. If treatment is started later than 12 hours from the onset of the rash, as well as in patients with weakened immune systems, short 1-day courses of therapy are usually ineffective. Here we already need a standard regimen of administration.
Important : if more than 12 hours have passed since the first rash appeared (and even more so if more than 24 or 48 hours), it is better to opt for famciclovir, because the latter works better at later dates of initiation of therapy for herpetic infection.
HERPES SIMPLE (HERPESIS SIMPLE)
This paper outlines the present-day concepts of the pathogenesis of herpes simplex, describes its main clinical manifestations, and considers its therapy. V.N. Grebenyuk, doctor med. Sciences, prof., head. Department of Pediatric Dermatology of the Central Research Institute of Dermatovenerology of the Ministry of Health of the Russian Federation. VN Grebenyuk, professor, MD, Head, Department of Pediatric Dermatology, Central Research of Dermatovenereologic Institute, Ministry of Health of the Russian Federation. P
Herpes growth is a serious medical and social problem. This is one of the most common human viral infections, often characterized by a persistent chronic course, affecting various organs, systems and tissues. According to WHO, about 70% of the population of our planet is infected with the herpes simplex virus (HSV) and approximately 10 - 20% of those infected have some clinical manifestations of herpes infection. HSV is a predominantly dermatoneurotropic DNA-containing virus; it also has tropism for other tissues, its size is 150 - 300 nm. The virion, in addition to DNA, consists of an icosahedral capsid and an outer shell containing lipids. It reproduces intracellularly (in the nucleus and cytoplasm) with a 14-hour reproduction cycle. During an acute infectious process, daughter virions are released from decaying cells. HSV infection can cause spontaneous abortions, fetal death and congenital deformities. The herpes virus is associated with the possibility of developing cervical cancer and some cardiovascular diseases. There are two antigenic types HSV-I and HSV-II, which cause lesions of the skin and mucous membranes of various localizations, which is determined by the place of introduction of the virus, usually through contact (coitus, kissing, through household objects). The source of infection can be not only patients with herpes, but also virus carriers who do not have symptoms of herpes.
| Rice. 1. Herpetic lesions of the face. a - forehead, eyelids, bridge of the nose; b - cheeks; c - lips and chin. |
3-4 weeks after infection, antibodies to HSV are formed in the body, the level of which remains relatively constant throughout a person’s life, regardless of the form of infection - manifest or latent. In the vast majority of people, the infection is asymptomatic or subclinical, and only in some infected people does it manifest clinically. Having penetrated the body, the herpes virus reaches a certain regional sensory ganglion (spinal or cranial) through lymphogenous, hematogenous or neurogenic routes, where it constantly persists. The latent state of the virus is based on the biological balance between micro- and macroorganisms. Under the influence of various provoking factors (psycho-emotional arousal, intoxication, overheating, etc.), a relapse of the disease occurs due to the reactivation of latent HSV, which leads to the formation of a recurrent disease. The range of clinical manifestations of the disease - from virus carriage to generalized forms - is determined both by the biological properties of the pathogen and the reactivity of the host. In most people, immune mechanisms, mainly cellular, maintain HSV latency. But in some infected people, antiviral resistance turns out to be untenable and relapses occur. There are two hypotheses that allow for the development of relapses based on both the static and dynamic state of the virus. According to the first hypothesis, the virus is located in the cells of the paravertebral sensory ganglion in an integrated or free non-productive state. Under the influence of the “trigger factor,” the virus, when activated, moves from the ganglion along the axon of the peripheral nerve to the epithelial cells, where it replicates. Cell susceptibility and weakened immune control are thought to contribute to this. According to the dynamic state hypothesis, replication and release of small amounts of virus from the ganglion occur continuously. Reaching the skin nerve, HSV causes microfoci of infection, which are restrained by defense mechanisms, which prevents relapses or weakens their manifestations. The development of relapses is also influenced by the state of local immunity. Its inhibition creates conditions for the replication of the virus that has reached the skin. The immune system plays an important role in containing the spread of herpes infection in the body. Immune protection is determined by the interaction and complex participation of specific and nonspecific factors. The main place in this system belongs to T-cell mechanisms of immunity. Mononuclear phagocytes and neutrophils play a significant role in maintaining local immunity and preventing the dissemination of infection. The protective functions of the body and the preservation of its homeostasis are also greatly influenced by the ability of cells to produce interferon.
Rice. 2. Herpetic felon.
| Rice. 3. Manifestations of herpes. a - on the palmar surface of the hand; b - on the thigh; c - on the buttocks |
Diseases caused by HSV are distinguished by a wide clinical variety of localization, severity, and characteristics of clinical manifestations. Primary herpes usually occurs after the first contact with HSV. More often it is observed in childhood against the background of a reduced immune status, in particular in the absence or low content of specific humoral antibodies. It is distinguished by the high intensity of clinical symptoms. The incubation period lasts several days. Primary herpes in newborns due to hematogenous dissemination becomes systemic, affecting the central nervous system and internal organs. The disease is characterized by herpetic lesions of the oral cavity, eyes, liver, bronchi, lungs, and brain. Usually the disease occurs acutely in the first days after birth and is manifested by anorexia, dyspeptic disorders, convulsions, septic condition, body temperature (39 - 40 ° C), disseminated herpetic rash on the skin and mucous membranes; Deaths are common in the first 2 weeks of illness. Children who have had generalized herpes experience neuropsychic complications. Kaposi's eczema herpetiformis is another severe type of herpes. Occurs mainly in children. It usually occurs in patients with atopic dermatitis, eczema, and other dermatoses in which there are skin lesions. The source of the disease can be patients with herpes in the acute stage. In adults, the disease may be associated with a recurrence of herpes labialis or another clinical form. Kaposi's eczema herpetiformis is characterized by a sudden onset (chills, malaise, body temperature up to 39 - 40 ° C for 1 - 1.5 weeks), a profuse vesicular rash on large areas of the skin, and painful regional lymphadenitis. The rashes appear in paroxysms over 2-3 weeks at intervals of several days. Often, along with skin lesions, the mucous membranes of the oral cavity, pharynx, trachea, and eyes are involved in the infectious process. Grouped and disseminated vesicles soon turn into pustules. In the center of the rash elements there are often umbilical recesses. After the crusts are rejected, secondary erythema remains on the vesiculopustules. Subjectively, the rash is accompanied by itching, burning, and soreness of the skin. Regional lymphadenitis is not uncommon. Patients are subject to hospitalization in an infectious diseases hospital or clinical hospital wards. In severe forms, the pathological process may involve the nervous system, eyes and internal organs. Relapses of Kaposi's eczema herpetiformis are rare, characterized by shorter duration and weakened clinical manifestations.
| Rice. 4. Genital herpes. a — bubble manifestations; b — erosive and ulcerative manifestations. |
The most common clinical form of primary infection is acute herpetic stomatitis.
It is more often observed in children in the first years of life; it is rare in adults. In weakened children, dissemination of the virus can lead to visceral pathology (in particular, hepatitis) and death. Acute herpetic stomatitis, occurring after about a week's incubation period, is characterized by a violent clinical picture. Chills, high body temperature (up to 39° C), painful vesicular-erosive rashes in the oral cavity, headache, general malaise, drowsiness - this is a list of the main symptoms of this disease. The rashes are most often located on the mucous membrane of the cheeks, gums, palate, lips, tongue, less often - on the soft and hard palate, palatine arches and tonsils, and spread to the skin around the mouth. The rash initially looks like grouped vesicles against a background of erythematous-edematous islands of the mucous membrane. The transparent contents of the elements become cloudy after 1 - 2 days, the covers of the vesicles are destroyed, and erosions form. In this case, regional lymph nodes are almost always enlarged and painful. Regression of the process usually occurs after 2 - 3 weeks. Recurrences of herpetic stomatitis, as a rule, are milder and resolve earlier. Herpes simplex is more common as a recurrent form. Clinical manifestations compared to primary herpes are less pronounced and not as long lasting. Most often, rashes are located on the face (lips, cheeks, nose), conjunctiva and cornea of the eyes, on the genitals and buttocks. The disease can last for many years and recur with varying frequencies - from several times a year to several times a month. In rare cases, the process becomes permanent when new rashes appear against the background of previous lesions that have not yet resolved. Frequent relapses of genital herpes are especially painful. The localization of herpetic lesions is determined by the site of virus introduction. The appearance of the rash is preceded by prodromal symptoms (burning, itching, tingling and other sensations). Grouped vesicles with a diameter of about 2 mm occur against a background of erythema. The transparent contents soon become cloudy and shrink into lumpy-yellowish crusts. When the vesicles rupture, scalloped erosions form. Their bottom is soft, reddish, the surface is smooth and moist. Regional, slightly painful lymphadenitis with a pasty consistency often occurs. The rash resolves within 1 to 2 weeks, leaving reddish-brown spots. When a microbial infection is added, the duration of relapses increases. Atypical forms of herpes simplex are known: abortive, zosteriform, disseminated, hemorrhagic-necrotic, migratory, elephantiasis-like, ulcerative, rupioid. The abortive form occurs in areas of the skin with a thickened stratum corneum and manifests itself as barely noticeable papules. Abortive manifestations of the disease also include erythematous and pruriginous-neurotic forms, characterized by local subjective disorders without typical rashes. The edematous form is usually located in areas of the skin with loose subcutaneous tissue (eyelids, lips) and is characterized by pronounced tissue swelling. Zosteriform herpes simplex is localized along the course of a nerve on the limbs, trunk, face and is accompanied by neuralgia, headache and general weakness. In the disseminated form of the disease, the rash simultaneously appears on areas of the skin that are distant from each other. The migratory form of recurrent herpes is characterized by a change in the localization of lesions. In hemorrhagic and hemorrhagic-necrotic forms, an admixture of blood is detected in the contents of the vesicles and necrosis develops. The elephantiasis-like form of the disease is characterized by severe swelling followed by the development of persistent elephantiasis in the affected area. Chronic cutaneous herpes simplex is an extremely rare clinical form. It is observed in patients with immunodeficiency and is characterized by permanent active manifestations of infection. Persistent ulcerative lesions up to 2 cm in diameter appear. The ulcerative form of herpes simplex is characterized by the development of ulcerative lesions, which is associated with a weakening of the patient’s immunobiological defense mechanisms and the increased virulence of the virus strain. This clinical type of herpes is characterized by the formation of ulcers at the site of weeping vesicles and fused erosions. The bottom of the ulcers is soft, pink-red in color, sometimes with a grayish-yellowish coating. In the first days of the disease, local pain and burning are expressed. Sometimes the rash is accompanied by inguinal lymphadenitis. The rupoid form of herpes simplex is usually localized on the face. It is caused by pyogenic infection with the development of cracks and layered crusts. Relapses occur several times a year. The rash is often accompanied by tenderness and enlargement of regional lymph nodes. With herpes of the hands, the process is often located on the distal parts of the hands. Limited lesions are represented by single dense blisters, accompanied by severe pain. The most common type of herpes simplex is facial herpes. In most people, these are sporadic focal vesicular eruptions, often resolving within 1 week. In severe cases, the process involves large surfaces of the face - nose, cheeks, forehead, skin and red border of the lips. Genital herpes occupies a significant place in the structure of herpetic diseases. Etiologically, its occurrence is equally often associated with types of HSV-I and/or HSV-II. Infection with one type of virus does not prevent the occurrence of HSV infection of another type, which leads to the formation of intermediate (“double”) antibodies. Mixed infection with HSV-I and HSV-II is quite common. The frequent isolation of HSV-I, which was previously considered the causative agent of non-genital forms of herpes, in genital lesions is due to the prevalence of orogenital contacts. Genital herpes is distinguished by the variability of its clinical picture and its tendency to have a chronic, relapsing course. In men, limited herpetic eruptions are often localized on the inner layer of the foreskin, in the head groove, and less often on the head and shaft of the penis. In women, the labia minora, clitoris, cervix, perineum and thighs are most often affected. Rashes (vesicles, erosions, ulcers, cracks) against a background of erythema and swelling are usually painful and are also accompanied by itching, a feeling of tension and heaviness in the perineum. About a third of patients have inguinal lymphadenitis. When the urethral mucosa is involved in the pathological process, serous discharge from the urethra and pain when urinating appear. The source of infection in the case of genital herpes is usually a patient in the acute stage of the disease; it can also be a virus carrier, given the possibility of asymptomatic persistence of HSV in the genitourinary tract in men and in the cervical canal. The incubation period for primary genital herpes lasts from one to several days. Clinically, primary genital herpes has a more severe and prolonged course. The localization of rashes on the genitals and adjacent areas is determined by the gates of the viral infection. A recurrent course of genital herpes is observed in the majority of infected people. Provoking factors are a variety of influences - psycho-emotional experiences, hypothermia, menstruation, weather and climate fluctuations, and other factors that disrupt the state of biological balance of the body, contributing to a decrease in the immune response and activation of HSV. The clinical picture, the amount of virus secreted by the patient and the associated infectivity are more pronounced with primary herpes than with a recurrent disease. Possible complications of herpes simplex: the addition of a secondary bacterial infection, reinfection with the released virus of other epithelial integuments, neurological manifestations (aseptic meningitis, transverse myelitis), encephalitis, disseminated infection of internal organs, psychosocial consequences (psychological instability). The risk of developing cervical cancer is 2 times higher in women who are seropositive for human papillomavirus types 16/18 and infected with HSV-II.
Diagnostics
The diagnosis of herpes simplex, especially its genital form, in most cases is based on the clinical picture. Difficulties arise with atypical manifestations of herpes. In this case, it is important to carefully collect anamnesis, paying attention to relapses accompanied by itching, burning, and ineffectiveness of antibiotic therapy. In addition, the patient may have a tendency to colds, general weakness, malaise, low-grade fever, and depression. Recurrent herpes is characterized by a wave-like course of the disease - an alternation of relapses and remissions. In women, relapses of herpes may be associated with certain phases of the menstrual cycle. The occurrence of erosions and ulcers on the genitals simulates syphilitic lesions. This similarity is most pronounced when a secondary microbial infection is attached, as well as during irrational therapy. The diagnosis of genital herpes is complicated by the fact that HSV is often associated with some resident autoflora microorganisms: chlamydia, streptococci and staphylococci, gardnerella and others, which can determine the occurrence of mixed infections. In addition, because herpes can be transmitted sexually, the patient must be tested to rule out other sexually transmitted diseases, including syphilis and AIDS. In complex cases, when clinical data is insufficient, laboratory diagnosis is possible. There are a number of specific laboratory tests to recognize HSV infection: isolation of HSV in cell culture, including HSV-I and HSV-II typing, tests to determine HSV antigen or DNA using polymerase chain reaction; serological tests - complement fixation test, ELISA, indirect immunofluorescence reaction, reverse passive hemagglutination reaction, protein-specific immune tests (immunoblotting), cytological examination (detection of multinucleated giant cells in scrapings from the lesion).
Treatment
Treatment of recurrent herpes remains a difficult task, which is not always solved effectively. It is possible to achieve some success if complex etiological and pathogenetic treatment is carried out at different stages of the disease, aimed, on the one hand, at suppressing the infectious agent, and on the other, at increasing the body’s immune reactivity. When choosing treatment, the stage of the disease should be taken into account. For relapses, interferon, antiviral chemotherapy, measles immunoglobulin, human normal immunoglobulin, levamisole, ascorbic acid, deoxyribonuclease, applications of 0.05% zinc sulfite solution are indicated; in the inter-relapse period - herpetic and polio vaccines, pyrogenal. The etiological focus is on antiviral chemotherapy drugs, which are more effective when used in the first hours and days of the appearance of rashes. Among them is the domestic drug Bonafton, which is used orally at 50–150 mg/day for 5–7 days for relapses. Simultaneously with the tablet form, 0.5% bonaftone ointment can be prescribed. It is applied to the lesions in an open manner when signs of relapse appear and is easily rubbed into the skin 2 - 3 times a day for 5 - 7 days. Side effects observed in some patients include malaise, loose stools, and dermatitis. Acyclovar (Zovirax) is effective, characterized by low toxicity and selectivity against HSV. The drug is used intravenously, orally and topically. It gives a pronounced therapeutic effect for Kaposi's eczema herpetiformis. Acyclovir is administered intravenously at the rate of 20 mg per 1 kg of body weight per day. However, the drug does not prevent herpes from recurring, infecting newborns, or infecting other people. Treatment of patients with recurrent herpes with acyclovir 0.1 - 0.2 g 5 times a day for 5 days during relapses shortens the time for resolution of rashes, reduces the severity of subjective sensations, smoothes out clinical manifestations and reduces the degree of virus shedding. Prophylactic administration of the drug 0.1 - 0.2 g 4 times a day for 6 - 12 weeks reduces the duration of relapses and weakens clinical manifestations. Other chemotherapy drugs: famciclovir, alpizarin (2 and 5% liniment), Viru Merz Serol, 1% oxolinic ointment, hevisos, ribavirin (virazol). A certain therapeutic effect is provided by immunocorrective drugs (myelopid, poludanum, arbidol), used both as monotherapy and in complex treatment. Myelopid (0.003 g in 2 ml of saline) is administered intramuscularly once every 3 days (5 injections per course). Treatment is carried out in two courses with an interval of 7 - 10 days. Poludan is administered subcutaneously into the forearm every other day, 100 mcg, for a course of 1000 mcg. Arbidol is prescribed 0.2 (2 tablets) 3 times a day - 5 days with a 2-day break, and then 0.1 g (1 tablet) 1 time per week for 3 weeks. Sodium nucleinate is also used orally at 0.5 - 1 g / day in 2 - 3 doses daily for 2 - 4 weeks. Taktivin is used to stop relapses and for prophylactic purposes. The drug is administered subcutaneously at a dose of 100 mcg every other day, 8 - 10 injections. During the inter-relapse period, 50 mcg is prescribed every other day, a course of 5 injections is repeated every 3-6 months. A course (4 - 5 injections) of treatment with timoptin is also carried out, which is administered subcutaneously at 100 mcg every 3 - 4 days. The courses are repeated after six months.
External treatment
Antiviral ointments, creams, lipsticks accelerate the epithelization of erosions, reduce or reduce subjective sensations in the affected areas. Local use of one or another antiviral drug in the treatment of herpetic lesions for 5 - 7 days shortens the time of regression; use 2 - 3 times a week during the inter-relapse period allows to prolong remission. Interferon has an inhibitory effect on HSV, which is applied to the skin and easily rubbed in for 4 to 7 days. During treatment, it is advisable to alternate antiviral drugs during relapses. Human interferons are effective in the treatment of recurrent herpes in the prodromal period and when the first signs of relapse appear. The ointment is applied to the lesions 2-4 times a day and rubbed in lightly; treatment is continued for a week. The use of interferon ointment during the inter-relapse period prolongs remissions and interrupts the development of relapses. In order to prevent relapses in frequently recurrent forms of herpes, patients for whom treatment is ineffective are prescribed a herpetic vaccine. Contraindications to its administration are lesions of parenchymal organs, diabetes mellitus, stage II and III hypertension, decompensated heart failure, acute infections and allergic diseases. The drug is administered intradermally during the period between relapses, 0.2 - 0.3 ml into the area of the flexor surface of one of the forearms. The first 5 injections are given after 3 - 4 days, the next 5 doses are administered after a 2-week break (once every 5 - 7 days). These 10 injections constitute the main course of treatment, 3–6 months after the end of which 1–2 cycles of revaccination are carried out, each of 5 injections with an interval between injections of 7–14 days and between cycles of 6–8 months. Over the next 2 years, an additional revaccination cycle of 5 injections is carried out every 8 - 12 months. At the injection site, after 18-24 hours, a local reaction develops, manifested by the development of erythema with a diameter of 2-5 cm with a papule in the center and accompanied by a burning sensation. During vaccination, a focal reaction such as abortive relapses may be observed. In this case, a break is taken in the treatment for 2 - 3 days, then it is continued. Specific vaccine therapy leads to an increase in the duration of remissions, a reduction in relapse periods, and the disappearance of subjective sensations. For the purpose of secondary prevention of relapse of herpes, the factors that provoke the disease are controlled. Great importance is attached to the sanitation of the body and health-improving measures in the process of medical examination.
Literature:
1. Barinsky I.F., Shubladze A.K., Kasparov A.A., Grebenyuk V.N.M.: Medicine. 1986, 269 p. 2. Masyukova S. A., Rezaikina A. V., Grebenyuk V. N., Fedorov S. M., Mkhitaryan A. G., Kolieva M. Kh. Immunotherapy of recurrent herpes simplex. Sexually transmitted diseases. Information analytical newsletter. Sanam Association 1995, 3, 27-30. 3. Minde CA. Genital Herpes. A guide to pharmacological therapy. Drugs 1994;47(2):297-304. 4. Whatley JD, Thin RN. Episodic acyclovir therapy to abort recurrent attacks of genital herpes simplex infection. J Antimicrobial Chemotherapy 1991;27:677-81.
Treatment with immunomodulators, prevention of herpes –
If you have a high frequency of relapses of herpes, or even rare, but severe outbreaks, it is very important for you to take up the prevention of outbreaks of herpes. And the point here is not only that the severe course of a herpetic infection and/or its frequent relapses themselves indicate problems with your immunity. The fact is that the herpes virus has an immunosuppressive effect on the entire immune system - both cellular and humoral immunity.
This means that the immune system under the influence of the herpes virus will continue to weaken, leading to a further increase in the frequency of relapses and the severity of outbreaks. At the moment, there are the following directions for preventing outbreaks of the herpes simplex virus (HSV-1, HSV-2), but you should choose one or another method only after consulting a doctor. All patients with a frequency of outbreaks of more than 6 during the year must be tested for the number of specific IgG and IgM antibodies to the herpes simplex virus, as well as consult an immunologist and have an immunogram (which evaluates the subpopulation composition of cells, NK activity, and also the levels of α- and γ-interferons).
Prevention methods:
- Prolonged use of antiviral drugs - in this case, Acyclovir tablets are prescribed 400 mg 2 times a day (but we do not recommend this option, since the use of acyclovir in patients with weakened immune systems very often leads to the development of resistance of the herpes virus to acyclovir ).
A preventive course of drugs from the list below should last about 9-12 months, and only on the recommendation of a doctor. The drug "Valacyclovir" - 500 mg 1 time per day (but for patients with a relapse rate of more than 9 times a year - 500 mg 2 times a day). The drug "Famciclovir" - 250 mg 2 times a day. Studies show that the preventive effect is more pronounced with Valacyclovir, but cross-resistance must also be taken into account (since if the herpes virus is resistant to acyclovir, it will also be resistant to valacyclovir). - Immunocorrective therapy – the immune system can be improved with special drugs “immunomodulators”. There are several drugs that have proven effective in preventing relapses of herpes, and for which this indication for use is directly stated in the instructions. The use of immunostimulating drugs allows - 1) to reduce the frequency of relapses by about 40-50%, 2) to reduce the duration of each outbreak, for example, complete healing will occur faster by about 2-3 days than usual.
Good drugs, the instructions for which specifically indicate “as part of the complex therapy of herpetic infection” are over-the-counter tablet drugs “Cycloferon”, “Polyoxidonium”, “Licopid” (you can look at the official instructions for treatment regimens). The first two drugs also have a release form as an injection solution, but this is only by prescription. By the way, Cycloferon, in addition to stimulating the immune system, also has its own antiviral activity against the herpes simplex virus (24stoma).Accordingly, if the patient has active manifestations of herpes, and the immunomodulator is used as part of complex therapy for herpes infection (together with antiviral drugs), Cycloferon will be the optimal choice. And, by the way, it can be used from 4 years old. If you use an immunomodulator between herpes outbreaks, i.e. in the absence of clinical manifestations, it is better to choose “Likopid” or “Polyoxidonium” (they can be used from 3 years of age).
Likopid" can be in tablets of 1 and 10 mg (tablets of 10 mg can only be taken as prescribed by a doctor, and tablets of 1 mg are available over the counter). Recommended use of Likopid 1 mg for adults – 2 tablets 3 times a day (orally or sublingually), course of treatment is 10 days. Scheme of use of Likopid 10 mg tablet for adults - 1 tablet 1 time per day, course of treatment for 6 days. For children over 3 years old, Likopid 1 mg tablets can be prescribed, and the regimen is as follows - 1 tablet 3 times a day (orally or sublingually), for a total of 10 days.
Important: taking immunomodulators is indicated not only for the prevention of relapses of herpes infection - in patients who are often and/or seriously ill with herpes. Immunomodulators should be used as part of the basic therapy of herpes infections (in addition to therapy with antiviral drugs) in patients with weakened immune systems.
Moreover, if the immunomodulator is used during an exacerbation of herpes, then it is best to use Cycloferon, because it also has a direct antiviral effect on the herpes simplex virus. If we are talking about taking immunomodulators in the period between outbreaks, then you can use Lykopid or Polyoxidonium. In the next section we will talk about the Vitagerpavac vaccine, which is nothing more than a real herpes vaccine.
Myth: You can be cured by cauterizing the rash with alcohol, iodine and brilliant green.
Unfortunately no. Cauterization does not affect the herpes virus and its activity, but burns to damaged skin and mucous membranes are possible. It is better to carefully lubricate the rash with an antiseptic that does not contain alcohol (this will prevent the addition of a purulent infection).
Article on the topic Herpes: causes, symptoms and treatment And herpes itself is treated with special antiviral drugs (the most famous and common is acyclovir). For frequent exacerbations, medications that strengthen the immune system and general restoratives are also used.
LekOboz recommends:
In addition to antiviral drugs, in the first 3 days of illness, take a multivitamin containing 600–800 mg of vitamin C and 600 mg of B vitamins. This will reduce pain and speed up the healing of ulcers.
Article on the topic
It is impossible to get rid of the herpes virus - there is no cure. How to fight it? Take immunomodulatory medications as prescribed by your doctor. The goal of such treatment is to bring the virus to a state of hibernation and at the same time eliminate disorders of the immune system.
Plant extracts of eleutherococcus, ginseng, echinacea, mumiyo, pantocrine help increase the duration of the relapse-free period. It makes sense to take them as a course. But they are ineffective for relieving exacerbations.
Prevention of genital herpes
The main preventive method is personal sexual abstinence, exclusion of casual sexual contacts, and the use of condoms:
- If casual sex occurs, it is necessary, without delaying for long, to undergo a full examination for the presence of hidden sexually transmitted infections.
- If signs of herpes or other suspicious symptoms appear, you should immediately visit a medical facility, get tested and begin timely treatment.
- It is worth excluding situations when you have to use other people’s hygiene products - towels, washcloths; everyone should have their own set of hygiene products, including in the family.
- It is not recommended to kiss children on the lips or use someone else's lipstick.
- If infection occurs, the patient must take medications to contain the virus and prevent the spread of infection.
Considering that the virus can be in the body undetected, it is worth regularly undergoing preventive tests to make sure that you are not carrying the virus.
It is also worth supporting the body and its immunity. Lead a healthy lifestyle, eat right, maintain intimate hygiene.
There is no 100% guarantee against infection. However, risky factors should be avoided. If casual sex occurs, herpferon ointment should be used for prevention within the next hour or two. And then be sure to get tested for antibodies.
Diagnosis of genital herpes
Despite the characteristic rash of herpes, other diagnostic data are also necessary to clarify the diagnosis. These tests also make it possible to determine the type of virus.
The doctor must refer the patient to:
- general blood analysis;
- blood testing for the presence of hidden infections, primarily herpes viruses;
- ultrasound diagnostics of the pelvic organs;
- diagnosis of vaginal microflora by examining a vaginal smear.
Sometimes you may need to consult other specialists - a urologist, gynecologist, cardiologist, neurologist.
Complication of genital herpes
Genital herpes leads to serious consequences. Once in the body, it causes not only skin rashes and itching. It can cause:
- Alzheimer's disease;
- meningitis, inflammation of the membranes of the brain;
- damage to the pelvic nerves;
- miscarriage, fetal death, premature birth;
- damage to organs and systems in a newborn child;
- blindness;
- neuralgic manifestations;
- frequent colds, chronic bronchitis, pneumonia;
- inflammation of the genitourinary system;
- infertility;
- inflammation of the gastrointestinal tract;
- provokes cystitis, vasiculitis, thrush.
Complications of herpes are difficult to treat. The herpes nature of the disease is difficult to diagnose. Sometimes people do not associate these illnesses with herpes infection.
In order to correctly diagnose the causes of the disease, it is recommended to undergo a herpes test.
If herpes appears frequently and in large numbers, this indicates serious disruptions in the immune system. In such cases, you will need the help of an immunologist.