Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
Not only the health of teeth and gums, but also the functioning of the digestive, immune and other systems and organs depends on the state of the oral microflora. Let's figure out what this part of the body is, what affects the conditions of the oral cavity and how to quickly restore the normal functioning of the microflora.
What is the microflora of the oral cavity?
Surprisingly, approximately 160 species of microorganisms live in the mouth of a healthy person. You've probably heard that “the mouth is the dirtiest place in the body.” This statement is partly true: the oral cavity is one of the most populated parts of the human body.
Microorganisms enter the oral cavity with food and water, as well as from the air. It is in the mouth that the most favorable conditions for the development of bacteria are observed. This part of the body always has uniform humidity and temperature (approximately 37 °C). The abundance of nutrients, sufficient oxygen content, the presence of folds in the oral cavity, interdental spaces and gum pockets, and slightly alkaline pH provoke the proliferation of various bacteria.
Microorganisms are unevenly distributed in the oral cavity. Their maximum number is observed on the surface of the teeth and on the back of the tongue. One gram of dental plaque contains approximately 300 billion microbes, and saliva contains approximately 900 million per 1 milliliter.
- 30-60% of the microflora are facultative and obligate anaerobic streptococci;
- part is occupied by Veillonella, coccobacteria, which ferment acetic, pyruvic and lactic acids to water and carbon dioxide. It is Veillonella that neutralizes acidic foods, so many dentists consider them as destroyers of cariogenic bacteria;
- Bacteria of the genera Propionibacterium, Corynebacterium and Eubacterium are also necessarily present in the mouth, which actively produce molecular oxygen, synthesize vitamin K and promote the development of obligate anaerobes. Some types of such bacteria provoke purulent inflammation.
- Lactobacilli are strict anaerobes. There are more than 10 types of similar bacteria in the mouth that form a biofilm in the cavity. The vital activity of these microorganisms creates a favorable environment for the development of normal microflora. Lactobacilli ferment carbohydrates to form lactic acid, lower the pH, and most importantly, prevent the development of pathogenic, putrefactive and gas-forming microflora.
- Rod-shaped lactobacilli in a certain amount are, like streptococci, producers of lactic acid.
- Bifidobacteria are necessary to ferment various carbohydrates, as well as produce B vitamins and antimicrobial substances that inhibit the growth of pathogenic microorganisms. Moreover, bifidobacteria are a bunch of epithelial cell receptors: they form a film that prevents the colonization of pathogenic bacteria.
It would take a very long time to list all the types of bacteria that populate the microflora of the oral cavity. It is important to understand that each person is unique, and to assess the “normality” of the microflora, you need to know the characteristics of a particular organism.
For example, in one case, a large number of lactobacilli in the oral cavity will preserve teeth, and in another, the formation of a large amount of lactic acid during their vital activity will retard the growth of other important microorganisms. The number of staphylococci, dysentery and typhoid bacilli decreases, carious processes become more active, and the microflora of the oral cavity will have to be restored.
Nine types of bacteria in the mouth
The human mouth is home to many microorganisms. It is not surprising that the oral microbiome ranks second in terms of the number and diversity of bacteria in the body, second only to the intestines, because inside there are different types of tissues and surfaces that come into contact with objects of the outside world.
Scientists count more than 700 known species of bacteria, as well as a variety of fungi, viruses and protozoa, inside the mouth. Many of the presented microorganisms are considered opportunistic flora, others – pathogenic. Let's look at nine types of microorganisms that have adverse effects inside the oral cavity.
Streptococcus mutans (streptococcus mutans)
The most well-known type of bacteria in the oral cavity, as it is considered the main cause of tooth decay. These bacteria begin to have a detrimental effect on teeth only if they manage to form colonies on the surface of the enamel, gradually destroying it.
Treponema denticola (Treponema denticola)
A type of gram-negative spirochete bacteria that plays a role in the development of periodontitis. They colonize periodontal pockets, causing inflammation. In the active stage of periodontitis, these bacteria are found in large quantities in periodontal tissues.
Trichomonas tenax (Trichomonas tenax, oral trichomonas)
The parasitic organism, often found in the mouths of people who do not practice good oral hygiene, is associated with periodontal infections. It is believed to feed on other microorganisms, but its secretions damage human tissue.
Entamoeba gingivalis (oral amoeba)
The first protozoan species discovered in the human microbiome. Some authors classify oral amoebae as opportunistic microflora. Others cite the results of studies proving the influence of oral amoebas on periodontal inflammation. They are localized in periodontal pockets, at the very base of the tooth. Found in 95% of patients with active periodontitis. Interestingly, these microorganisms are extremely rare in the oral cavity of patients with healthy gums.
Candida (candida)
Candida is a genus of yeast, the most common type of fungus in the human mouth and intestines. Considered an opportunistic pathogen, the most common type is Candida albicans. However, under certain conditions it can cause diseases such as aphthous stomatitis and even invasive candidiasis.
Actinomyces israelii (Wolff-Israel actinomycetes)
A species of rod-shaped bacteria from the actinomycetes family. Found in the oral cavity of healthy people. However, they can contribute to the development of caries, and are also considered the main cause of actinomycosis.
Campylobacter concisus (Campylobacter consisus)
A type of campylobacter that inhabits the oral cavity. Unlike most previously described microorganisms, Campylobacter is found in various organs and can cause severe disease. For example, this species can be found in the intestines, causing inflammatory diseases of the intestines and lower gastrointestinal tract.
Veillonella parvula (veillonella parvula)
Often found in the microbiome of healthy people, it has a negative effect on the development of caries and periodontitis. It poses a great danger to the cardiovascular system, since the activity of the bacteria Veillionella parvula has been found to be associated with hypertension and endocarditis.
Fusobacterium nucleatum (Plauta's bacillus)
An opportunistic microorganism, which, nevertheless, contributes to the formation of periodontal plaque. Studies have found a connection between Plaut's bacillus and premature birth, as well as colon cancer.
Disturbance of oral microflora: causes
Oral dysbiosis can be caused by a variety of diseases and problems. Violation of opportunistic microflora of the oral cavity most often causes problems such as:
- Diseases of the gastrointestinal tract. Malfunctions of the digestive organs lead to a slowdown in metabolic processes in the body. The absorption of vitamins and nutrients deteriorates, the balance of the intestinal bacterial environment is disrupted, which provokes problems in other organs and systems.
- Decreased immunity. If the body's resistance deteriorates, the oral cavity automatically becomes more vulnerable to pathogenic microflora.
- Chronic diseases. Often, small caries or stomatitis, if left untreated, can spread from the source of inflammation to the entire oral cavity.
- Bad habits, such as systematic drinking of alcohol and smoking, inevitably affect the quality of the salivary glands. Prolonged drying out or too much moisture in the oral cavity has a detrimental effect on the composition of the microflora.
- Poor nutrition and lack of vitamins worsens the quality of saliva and makes the microflora of the oral cavity more vulnerable.
- Taking antibiotics and certain medications, such as hormones;
- Wearing dentures.
Why do bacteria and germs cause oral diseases?
Even stable microflora of the oral cavity cannot be called completely safe. Thus, any damage to the mucous membrane or tooth enamel and subsequent inflammation contribute to the development of pathogenic processes. Even normal microflora can become unfriendly with weakened immunity.
The most dangerous are “alien bacteria”. They reproduce as a result of disruption of the normal functioning of the ecosystem. This phenomenon is common in periodontitis, caries, stomatitis, gingivitis and other diseases. The uncontrolled spread of bacteria, fungi and microbes leads to the release of toxins and the development of the inflammatory process. Often such microorganisms demonstrate a tendency to constant relapses, especially if therapy is not accompanied by restoration of the microflora.
Stages of dysbiosis
Depending on the degree of development of the disease, dentists distinguish four stages of dysbiosis:
- Latent. The first, latent stage is characterized by subtle changes in the number of microorganisms of one strain. The patient feels well and does not experience any symptoms of inflammation.
- Subcompensated. The number of lactobacilli decreases, the disease has a blurred picture. The patient may feel discomfort in the oral cavity, but does not always understand that this is dysbacteriosis.
- Pathogenic. Lactobacilli are observed in minimal quantities in the oral cavity. The oral cavity begins to be populated by a facultative pathogenic environment.
- Decompensated. In addition to severe inflammation in the mouth, uncontrolled growth of yeast-like fungi occurs. The functioning of the salivary glands is disrupted, and an unpleasant taste and burning sensation occurs in the mouth.
Advanced forms of dysbiosis are characterized by symptoms such as:
- inflammation of the gums and mucous membranes;
- plaque on the teeth and surface of the tongue;
- bleeding gums;
- ulcers and blisters on mucous membranes;
- increased body temperature;
- swelling and soreness of the tongue;
- dry skin, sticking in the corners of the mouth.
Methods for restoring oral microflora
Treatment of dysbacteriosis depends, first of all, on the nature of the pathogen, which is determined on the basis of dental examination.
Unfortunately, making a diagnosis of dysbacteriosis is often difficult, since at the initial stage the disease does not manifest itself in any way. At the slightest suspicion of a disease, the dentist refers the patient to a smear from the surface of the mucous membranes, blood and urine tests.
Depending on the diagnosed cause of dysbiosis, the dentist may prescribe the following methods of treating the disease:
- Sanitation of the oral cavity. The doctor removes tartar and fills all teeth affected by caries, and, if possible, treats the gums and mucous membranes.
- Treating the oral cavity with antiseptics to eliminate pathogenic microorganisms.
- Taking immunostimulants to strengthen the body and activate its defenses.
- A course of probiotics to restore the balance of beneficial bacteria in the oral cavity.
- Taking vitamin complexes for general strengthening of the body with vitamin deficiency. Properly prescribed vitamins promote cell regeneration and strengthen bone tissue.
In rare cases, antifungal agents and antibiotics are prescribed.
As a rule, the duration of treatment for dysbiosis is 2-4 weeks and depends on the patient’s health status, the number of foci of inflammation and existing complications of the disease.
A reliable assistant in the fight against dysbiosis will be the probiotic complex ASEPTA PARODONTAL*, a source of lactobacilli to restore the microflora of the oral cavity. This unique complex with patented strains of lactobacilli and vitamin D has the ability to effectively restore oral microflora. The complex normalizes the bacterial flora in the oral cavity, eliminates bad breath and prevents the formation of biofilms of pathogenic microorganisms.
To improve the effectiveness of the prescribed therapy, dentists recommend giving up bad habits (at least for the duration of treatment), reviewing the diet, paying attention to plant foods, and be sure to take care of the oral cavity after each meal.
Lek Microflora floor of the mouth dental plaque
9
Lecture. Microflora of the oral cavity, dental plaque, dental plaque. Pathogenicity factors of cariogenic streptococci, veillonella, fusobacteria. Causative agents of purulent-inflammatory processes in
dentistry. Dental sepsis. Anaerobic infection
maxillofacial region.
The microbial flora of the oral cavity is a collection of various bacteria, fungi, protozoa and viruses that can enter into a symbiotic relationship with humans as a biological species.
The dominant place, both in the diversity of species living in the oral cavity and in quantity, is occupied by bacteria. The number of bacterial species in this ecological niche ranges from 120 to 200. The content of microorganisms in saliva (oral fluid) ranges from 4 million to 5 billion per ml, in dental plaque (plaque) - from 10 to 1000 billion per g of material. They are widely represented by gram+ and gram– microorganisms, both coccoid bacteria and rod-shaped and convoluted forms.
Obligate anaerobic (fusobacteria, bacteroides) and microaerophilic (aerotolerant) flora (streptococci, actinomycetes, corynebacteria) of the oral cavity account for 80 to 96% of microorganisms. The remaining part consists of facultative anaerobic species - staphylococci, streptococci, enterobacteria, and aerobic neisseria, Haemophilus influenzae, non-fermenting gram bacilli (acinetobacter, moraxella, bordetella).
A significant place in the microbiocenosis of the oral cavity is occupied by convoluted forms: vibrios, campylobacters, spirillum and spirochetes. They are mainly obligate anaerobes and less often microaerophiles.
The number of anaerobic species of microorganisms is 106–1011 CFU/ml or g of material. The ratio of anaerobes to aerobes is approximately 100:1. Almost without exception, all types of anaerobic bacteria isolated during pathology are representatives of the normal microflora of the oral cavity.
Brief characteristics of the most clinically significant genera and species of obligate anaerobic
bacteria.
Genus Peptostreptococcus
– gram+ non-spore forming cocci, round or slightly elongated, often forming short and long chains. They have low saccharolytic activity, but decompose peptone and amino acids. They are contained in large quantities in dental plaque, released from carious cavities, root canals during pulpitis and periodontitis, from periodontal pockets, purulent exudate during acute and chronic inflammatory processes of the maxillofacial area. Important species: P.anaerobius, P.micros, P.asaccharolyticus.
Genus Veillonella
– gram-anaerobic cocci, in smears they are located in groups and clusters. Lactate, pyruvate, and acetic acid, which form streptococci and lactobacilli from carbohydrates, ferment well. They are found in saliva, on the mucous membrane of the mouth and gums, in the deep layers of dental plaque. They are often isolated during various pathological processes: from purulent exudate and the contents of periodontal pockets.
Genus Actinomyces
– gram+ rods with a tendency to form branching filamentous elements that form the basis of dental plaque. Due to adhesion, other symbionts of dental plaque, for example, cocci, are fixed on them. Actinomycetes are important in the etiology of caries, periodontitis, nonspecific inflammatory processes and actinomycosis. When fermenting carbohydrates, actinomycetes form lactate, acetic, formic and succinic acids, which have a strong cariogenic effect. Their dental plaques are isolated normally and in pathology, from carious cavities, periodontal pockets, and are contained in purulent materials in actinomycosis, chronic inflammatory processes of soft tissues and osteomyelitis of the maxillofacial region. Main species: A.israellii, A.naeslundii, A.viscosus, A.odontolyticus.
Genus Fusobacterium
– gram sticks of elongated spindle-shaped form with pointed ends. Produce butyric and other acids. Normally they inhabit the oral mucosa and dental plaque. In pathology, they are isolated from purulent exudate, the contents of the periodontal pocket, in ulcerative necrotic stomatitis and Vincent's angina in association with spirochetes. Main species: F.nucleatum, F.necroforum, F.mortiferrum.
Genera Bacteroides, Porphyromonas and Prevotella
– small gram rods and coccobacteria. They do not have spores or flagella. Produce fatty acids. Normally they are detected on the oral mucosa and as part of dental plaque. They are isolated in various inflammatory processes of the maxillofacial area, often in association with anaerobic cocci, fusobacteria, streptococci and staphylococci. Main species: B.fragilis, Porph.gingivalis, Prev.melaninogenica.
Genus Clostridium
– gram+ spore-forming rods, some are mobile, biochemically active. Normally they are part of the intestinal microbiocenosis. They are not constantly detected in the oral cavity. Isolated in patients with purulent wounds of the maxillofacial area. If the wound surface is contaminated and there is extensive tissue trauma, a gas anaerobic infection may develop. Main species: C.perfringens, C.septicum, etc.
Facultative anaerobic microflora. Staphylococci are isolated from inflammatory foci in 10-15% of cases: Staphylococcus aureus, less often S.epidermidis, S.saprophyticus, S.hominis, S.warneri, S.xylosus; in 15% streptococci: S.pyogenes, S.faecalis, S.viridans.
Microaerophilic streptococci play a huge role in the microbiocenosis of the oral cavity. The frequency of their isolation from purulent exudate or the contents of periodontal pockets is 10-35%; they constitute a significant part of the material of dental plaque and other biotopes of the oral cavity.
The metabolic features of one of them - S.mutans - release a significant amount of lactic acid, leading to decalcification of tooth enamel due to the low pH of the environment. In combination with high adhesive properties to tooth enamel, it can be considered as one of the leading factors in the development of caries. S.sanguis also play an equally important role.
Microaerophilic streptococci S.sanguis, S.salivarius, S.milleri, S.mitis, S.intermedius are often found in pathological material from periodontitis, abscesses, phlegmon and osteomyelitis of the maxillofacial area, the contents of periodontal pockets and purulent discharge.
Aerobic non-fermenting gram bacteria of the genera: Acinetobacter, Eikenella, Moraxella, Pseudomonas, Neisseria also take part in the development of purulent-inflammatory processes. In the development of purulent periodontitis, the role of gram bacteria Actinobacillus actinomycetemcommitans has been proven.
In immunodeficiency states, purulent-inflammatory processes in the maxillofacial area are associated with gram-enterobacteria of the genera Escherichia, Enterobacter, Proteus, Providencia and bacilli (B.licheniformis, B.coagulans, B.cereus).
Biotopes of the oral cavity:
- Oral mucosa
- Ducts of the salivary glands containing saliva
- Gingival fluid and gingival groove area
- Oral fluid
- Dental plaque
The microbiocenosis of each biotope differs due to differences in physical and chemical characteristics, pH of the environment, viscosity, temperature, the presence of organic compounds and food residues, and partial pressure of gases.
Oral mucosa
– the most extensive and diverse biotope. On the surface of the mucous membrane, predominantly gram-anaerobic and facultative anaerobic flora, as well as microaerophilic streptococci, grow.
In the sublingual region, on the inner surface of the cheeks, in the folds and crypts of the oral cavity, anaerobes predominate: veillonella, peptostreptococci, lactobacilli, and streptococci (S.mitis). The dorsum of the tongue is colonized by S. salivarius.
Streptococci, corynebacteria, neisseria, hemophila, pseudomonads, yeast-like fungi and nocardia are found on the mucus of the hard and soft palate, palatine arches, and tonsils.
There are from 200 to 20,000 microbial cells per 1 cm2 of CO.
Salivary gland ducts and saliva
practically sterile due to the high bactericidal activity of enzymes, lysozyme, secretory immunoglobulins and other factors.
Gingival fluid and gingival groove
. The biotope is dominated by filamentous and convoluted obligate anaerobic species of bacteria: fusobacteria, leptotrichia, actinomycetes, spirillum, anaerobibrio, campylobacter and spirochetes. This is the main habitat of anaerobic bacteroids, porphyromonas, prevotella. Protozoa, yeast-like fungi and mycoplasmas are also found here. The number of bacteria in the gingival fluid in a healthy person is no more than 105 mt/ml, and with the development of gingivitis or periodontitis up to 108 mt/ml.
Oral fluid.
The basis of oral fluid is saliva, which receives microbes from the mucous membrane, gingival groove, folds and dental plaque. This biotope contains Veillonella, microaerophilic streptococci (S.salivarius), facultative anaerobic streptococci, aerococci and mycoplasmas. The number of microorganisms in healthy people is 106–1010 mt/ml.
Dental plaque
– the most complex and multicomponent biotope formed on the surface of the tooth. Almost all representatives of the microbial flora of the oral cavity are determined in the composition of dental plaque. Their number varies significantly among different people and at different periods of their lives.
In the formation of a biotope, the determining role of the macroorganism and environmental factors (diet, lifestyle, occupational hazards, etc.) is undoubted. Quantitative and qualitative disturbances in the composition of the symbionts of a given biotope, disturbances in their interaction with the macroorganism play a decisive role in the emergence of such important nosological forms as dental caries and periodontitis.
To study the composition of dental plaque, a technique is used to take the material with a probe or metal spatula, followed by weighing on an analytical balance. After this, mechanical grinding of the plaque or its disintegration by ultrasound and quantitative inoculation on optimal nutrient media and cultivation under both aerobic and anaerobic conditions are carried out. The number of bacteria is expressed in colony-forming units per g of material (CFU/g).
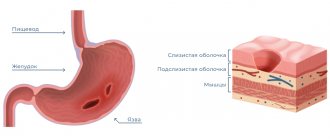
According to modern ideas, on the surface of the tooth enamel there are:
1 – cuticle, which is a reduced enamel epithelium,
2 – pellicle – an organic polymer film formed when enamel comes into contact with saliva,
3 – dental plaque or dental plaque.
Dental plaque consists mainly of microbes with a small inclusion of structureless substance of organic nature.
In the formation of dental plaque, several main mechanisms can be distinguished:
- Adhesion of epithelial cells invaded by bacteria to the enamel, followed by the growth of microcolonies,
- Precipitation of extracellular glycans produced by S. mutans and S. sanguis
- Precipitation of salivary glycoproteins forming a pellicle with subsequent specific adhesion of bacteria to it,
- Agglutination of bacteria with antibodies followed by fixation on the enamel surface. The bacteria in dental plaque are coated with IgA and IgG.
Dental plaque begins to form within 1–2 hours after brushing the teeth, and in the dynamics of its formation, significant changes in the nature of the microbiocenosis occur. The general trend is a change in the composition of the flora from the dominance of aerobic and facultative anaerobic forms, mainly cocci, to obligate anaerobic gram-negative rods and convoluted forms.
1 phase
formation of dental plaque – the first 2-4 hours after thorough brushing of teeth. It mainly consists of cocci (streptococci, neisseria and staphylococci) and short rods (lactobacillus). This is the so-called "early" dental plaque.
2 phase
– up to 4-5 days. It is characterized by a decrease in the proportion of Gram+ cocci and the prevalence of gram-variable filamentous forms - leptotrichia and fusobacteria.
3 phase
– from 6-7 days onwards. The dental plaque takes on its final form in terms of the composition of symbionts, although quantitative changes in it occur constantly. The number of aerobic species - Neisseria, Rotium, and facultative anaerobic streptococci - sharply decreases. The dominant species are gram-obligate anaerobic bacteria - bacteroides, fusobacteria, veillonella and gram+ actinomycetes, microaerophilic streptococci and peptostreptococci.
The total number of bacteria in a dental plaque increases from 90-100 CFU/g in the 1st phase of formation to 1-10 million CFU/g in the 2nd phase and to tens and hundreds of billions per 1 g in the 3rd phase of formation.
Bacteria have unequal adhesion to different tooth surfaces. The adhesion process is influenced by mechanical factors associated with the chewing process, physicochemical conditions, etc. Therefore, on different surfaces of teeth, in pits and fissures, the composition of the microflora differs even within the same tooth.
Dental plaque also forms on the surface of fillings, and its composition is somewhat different and depends on the nature and quality of the filling material. The microbial flora on cements and amalgams is most richly represented. An average level of colonization is typical for macrocomposite filling materials. On microcomposite materials, dental plaque is poorly formed due to the low affinity of bacteria.
It has been established that after eating food, especially one rich in carbohydrates, a sharp increase in the enzymatic activity of bacteria occurs in the oral fluid - a “metabolic explosion”. At the same time, the process of glycolysis is activated, which leads to a sharp shift in the pH of the environment to the acidic side due to the release of acidic catabolites - acetic, lactic, formic, pyruvic and other acids.
In turn, this leads to the release of calcium ions from the hard tissues of the tooth (demineralization), as well as a decrease in the phosphate content during the process of phosphorylation in bacteria. In addition, dental plaque bacteria accumulate excess carbohydrates in the form of reserve polysaccharides - dextrans and levans.
Etiology and pathogenesis of inflammatory diseases of the maxillofacial area
In the balance of all components of the microbiocenosis, the violation of which leads to the development of the infectious process, regulatory (immune and non-immune) mechanisms play a determining role. This is confirmed by the polyetiological nature of opportunistic infections. As a rule, associations of several types are isolated from the inflammatory focus.
At the same time, the properties of the microorganisms themselves may change and under certain conditions they may exhibit their pathogenic properties. Opportunistic bacteria have genes that encode the formation of the most important phenotypic signs of pathogenicity. However, their implementation of this information is significantly reduced or blocked due to the constant influence of the regulatory systems of the human body and other components of the normal microbiocenosis.
Signs of pathogenicity of UPM
- Colonization
– the ability of bacteria to colonize a specific biotope or ecological niche of an organism. This is possible if they have
- Adhesion factors
ensuring adhesion to the surface of tissues or tooth enamel. Adhesion is realized through several basic mechanisms:
- Through cell wall molecules such as galactose-binding lectins of actinomycetes or lipoteichoic acids of streptococci, interacting with fibronectin, a protein in blood plasma and tissue fluid,
- Through specific bacterial villi - pili or fimbriae, as well as surface vesicles in Porphyromonas gingivalis,
- Due to hemagglutinins and coaggregation factors with other bacteria, which are identified in oral streptococci, actinomycetes, fusobacteria and bacteroides,
- Due to the adhesive properties of the capsule in streptococci and bacteroides.
- Factors of protection
which allow bacteria to “protect themselves” from bactericins that produce antagonist microbes and resist the action of numerous protective factors of the human body.
Protection factors include: 1) the polysaccharide capsule
of bacteroides, streptococci and other bacteria, which determines resistance to phagocytosis, the action of antibodies and some antibacterial drugs;
2) enzyme systems
of bacteria that break down IgG and IgM, C3 and C5 components of complement, transferrin, hemopexin, haptoglobin, etc. - Invasiveness
– the ability of bacteria to leave the biotope with subsequent local spread in tissues (contamination) or spread throughout the body by blood and lymph flow (dissimination). Invasiveness is the trigger point in the pathogenesis of an infectious disease. In its implementation, the main role is played by aggression enzymes - hyaluronidase, chondroitin sulfatase, lecithinase, heparinase, protease, DNAase, neuraminidase, alkaline phosphatase, catalase, peroxidase, β-lactamase, etc.
- Toxigenicity
– the ability of bacteria to form exo- and endotoxins, as well as toxic metabolic products – indole, ammonia, formic acid, hydrogen sulfide, etc. Hemolytic and hemotoxic properties are expressed in streptococci, prevotella, bacteroides, clostridia. Clostridia exotoxins have necrotic, histolytic, neurotoxic and other properties.
Inflammatory diseases caused by opportunistic microbes affect any tissue of the maxillofacial area: mucous membrane, fatty tissue, muscles and fascia, ligaments and bones. For the development of a disease, it is necessary that conditions arise for the microflora to go beyond the limits of its inherent ecological niche or biotope in the body.
They can be local, purely mechanical, or general, associated with disruption of regulation and protection throughout the body.
To local conditions
include: trauma to the oral mucosa, tooth extraction, blood stasis in the capillaries, tissue necrosis, decreased partial pressure of oxygen, deficiency of various local systems and protective factors.
General terms
: somatic diseases and conditions leading to a lack of nonspecific resistance or immunological reactivity of the body as a whole.
Etiology of purulent-inflammatory diseases
maxillofacial area and neck
In the vast majority of cases, purulent-inflammatory processes are caused by resident microflora of the oral cavity. The development of these diseases is preceded by the activation of chronic odontogenic foci (chronic periodontitis, periodontitis, periocoronitis, lymphadenitis, etc.), acute processes (acute periodontitis, lymphadenitis, etc.). Penetration of infection into soft tissues and bone can occur in various ways: lymphogenous, hematogenous, along the length, contact, etc.
In 90-100% of cases, the focus of inflammation is determined from 2 to 7 types of different microorganisms, while in more than half of the patients a combination of obligate and facultative anaerobic species is determined, in 30% of associations only anaerobes are detected.
About 65% of the strains were represented by non-spore-forming anaerobic bacteria, predominantly gram-bacillus (bacteroides and fusobacteria) and gram-+ cocci (peptostreptococci and peptococci); actinomycetes and veillonella were less frequently identified. Facultative anaerobic and aerobic bacteria account for an average of 35% of all isolated strains. Of these, the most frequently identified are staphylococci (17.4%), streptococci, enterobacteria and bacilli.
A special place in the development of odontogenic inflammation belongs to anaerobic bacteria of the bacteroid group. In purulent foci there are more than 10 types of these microorganisms, which belong to three genera Bacteroides, Porphyromonas, Prevotella. The main species identified are: P.melaninogenicus, P.assaccarolyticus, P.capillosus, P.oralis. These species form pigment and produce a variety of fatty acids.
Bacteroides are often isolated from purulent foci and in 1/3 of patients they predominate in the microbial association. Bacteria of the genus Peptostreptococcus predominate in 20%, staphylococci - 15% of associations. Other microorganisms are leading in 3-8% of cases. The concentration of microorganisms in purulent exudate is lower with limited foci and higher with diffuse ones, involving two or more cellular spaces.
Microflora in acute odontogenic purulent-inflammatory diseases
is mixed with a clearly defined anaerobic accent, which must be taken into account when conducting antibacterial therapy.
In chronic inflammatory diseases, both nonspecific (chronic lymphadenitis, chronic osteomyelitis, etc.) and actinomycosis, the microflora of the inflammatory focus differs little: obligate anaerobes make up about 60%, microaerophilic streptococci up to 6%, in other cases facultative and aerobic microorganisms. The dominant microflora in these patients are bacteroides, peptostreptococci, staphylococci and, less commonly, bacilli. Anaerobic actinomycetes (A.israelii, A.naeslundii, etc.) are isolated in 8-10% of patients.
Possible complications of dysbiosis
It is important for each patient to closely monitor the state of the oral microflora. Lack of treatment for dysbiosis can lead to such unpleasant diseases as:
- pathological halitosis – bad breath caused by an imbalance of the oral microflora;
- caries – destruction of hard tooth tissues;
- pulpitis - inflammation of the pulp - the internal tissues of the tooth;
- periodontitis – inflammation of the tooth root membrane and adjacent tissues;
- gingivitis – inflammation of the oral mucosa;
- stomatitis – damage to the oral mucosa;
- periodontitis is a deep lesion of the periodontal tissue.
In addition, the close relationship between the state of the oral microflora and the state of the cardiovascular system has been scientifically proven. In 2008, it was proven in the USA that periodontal disease, as a source of chronic inflammation, is an independent risk factor for coronary heart disease (CHD).
So, now you know the role of normal oral microflora in the human body. Treat yourself carefully, and your healthy body will delight you every day.