Stomach ulcer, its types and stages
Gastric ulcer (hereinafter referred to as PUD) is a disease in which a mucosal defect occurs and the submucosal layer may be affected. This is a chronic disease that occurs in waves, with periods of exacerbation and remission.
An ulcer can be localized in different parts of the stomach:
- subcardial and cardiac - in the upper part;
- antrum - in the lower section;
- in the body - in the middle part;
- in the pyloric canal - at the transition to the duodenum.
The size of the ulcer is:
- small - up to 5 mm in diameter;
- medium - in diameter 6-19 mm;
- large - 20-30 mm in diameter;
- gigantic - more than 30 mm in diameter.
There are also ulcers associated with the bacterium Helicobacter pylori (hereinafter referred to as HP) and those not associated with it.
The disease occurs in several stages:
- exacerbations - the occurrence of a defect in the mucous membrane;
- scarring - the formation of connective tissue at the site of the ulcer;
- remission - healing of the defect.
The stage of cicatricial and ulcerative deformation of the organ is distinguished separately.
Main causes
The cause of a defect in the gastric mucosa is considered to be an imbalance between the aggressive secretions of the stomach and the protective qualities of the mucous membrane. To digest food, the stomach secretes pepsin and hydrochloric acid. To prevent them from destroying the stomach, mucus forms on its surface, protecting the organ. If more acid is produced and less mucus is produced, an ulcer may form. The background for such a pathology may be a decrease in gastric motility, a violation of the regenerative - restorative properties of the mucous membrane against the background of certain diseases.
The main etiological cause of ulcer formation is damage to the mucous membrane of the HP. This bacterium successfully survives in an acidic environment and produces an enzyme that causes an inflammatory reaction with subsequent formation of a defect. Helicobacter pylori is detected in 82% of patients suffering from gastric ulcers.
Another reason may be uncontrolled use of anti-inflammatory non-steroidal drugs, such as aspirin.
Provoking factors may be:
- smoking and alcohol abuse;
- constant consumption of spicy food;
- stressful situations;
- hereditary predisposition;
- dry food;
- eating disorder.
Gastric ulcers often develop against the background of certain diseases, such as atrophic gastritis and hormonal pathologies.
Foods High in Iron
Our body cannot synthesize iron; it only processes this element, extracting it from worn-out red blood cells. “Fresh” iron comes from food. However, even if you eat foods containing iron, this does not mean that you have enough. The thing is that there are two types of iron.
Iron can be heme (divalent) or non-heme (trivalent). The first is found in products of animal origin and is easily digestible (about 25%), the second is part of plants and is absorbed by only 8–10% maximum[3]. This is why vegans and vegetarians often lack this element, even if they eat foods rich in iron.
And yet, it is the right diet that is considered the main way to prevent iron deficiency. Iron is found in significant doses in the following foods:
Animal products:
- pork liver - 29 mg (hereinafter the figure is given per 100 g of product);
- hard cheese - 19 mg;
- beef liver - 9 mg;
- egg yolk - 6 mg;
- beef tongue - 5 mg;
- turkey - 4 mg;
- beef - 2.8 mg;
- chicken - 2.5 mg;
- mackerel - 2.5 mg;
- pork - 1.6 mg;
- herring - 1 mg;
- cottage cheese - 0.4 mg.
Products of plant origin:
- beans - 72 mg;
- hazelnuts - 51 mg;
- oat flakes - 45 mg;
- fresh forest mushrooms - 35 mg;
- millet - 31 mg;
- peas - 20 mg;
- seaweed - 16 mg;
- prunes - 13 mg;
- dried apricots - 12 mg;
- buckwheat - 8 mg;
- tofu - 5.5 mg;
- peaches - 4.1 mg.
Although the iron content of some plant foods is high, the non-heme form of iron is poorly absorbed. Therefore, it is important for those following a plant-based diet to check their iron levels and, if necessary, take dietary supplements that contain this element.
Our body perceives iron best from meat (on average 20% is absorbed), a little worse from fish and seafood (about 11%), legumes (7%) and nuts (6%). Only 1-3% of iron is absorbed from fruits, vegetables and cereals.
To improve the absorption of iron, it is also important to receive the right amounts of vitamins and minerals, which play the role of catalysts and help this element to be absorbed. These include:
- Vitamin C. Iron is almost not absorbed without ascorbic acid, so the menu must include foods rich in ascorbic acid - berries, oranges and grapefruits, cabbage, red peppers.
- Vitamin A. If a person lacks vitamin A, then iron will not be absorbed and used to “build” new red blood cells. Many orange and yellow fruits and vegetables are rich in vitamin A - it is this substance that gives them their cheerful colors. To replenish vitamin A reserves, you need to eat more dried apricots, carrots and pumpkin. However, it's important to know that fats are needed for this vitamin to be absorbed, so don't ignore sources of retinol like butter, fish oil, and egg yolks.
- Folic acid (vitamin B9). It helps absorb iron and normalizes the digestive tract, and healthy digestion is extremely important for the absorption of this element. Sources of folic acid are eggs, soybeans, yeast, green leafy vegetables, dill, eggplant, tomatoes, chicken liver.
- Copper. Sources of copper are offal, fish and seafood (shrimp, oysters, etc.), cabbage.
Symptoms of the disease
Peptic ulcer usually manifests itself more often in spring and autumn, during the period of exacerbation of the disease. The first sign of the disease is pain that occurs immediately after eating. This is due to the fact that pepsin and hydrochloric acid released during meals aggressively affect the defect unprotected by mucus. Moreover, the manifestations of pain symptoms increase within an hour after eating. The pain is localized in the epigastric region, in the region of the heart, and can radiate - radiate under the scapula, as in a heart attack. At the height of the pain syndrome, nausea often occurs, which can result in vomiting, which brings relief.
Other dyspeptic manifestations and signs of illness: heartburn, loss of appetite, constipation. A coated tongue may indicate stomach problems. Against this background, the patient quickly loses weight.
Changes in the oral mucosa in diseases of the gastrointestinal tract
- Changing the language
In diseases of the gastrointestinal tract, the condition of the tongue is best studied.
The appearance of the tongue, as many authors believe, can have important diagnostic value and indicate existing pathology of the digestive tract. Changes in the tongue in diseases of the gastrointestinal tract are of a nonspecific nature, manifested by the formation of plaque, swelling, desquamation, atrophy of the papillae, paresthesia, impaired taste sensitivity, and are also quite labile; they can disappear during the period of remission of the underlying disease or during its treatment. Coated tongue is most often detected. Plaque consists mainly of keratinized epithelial cells, bacteria, fungi, and food debris. The severity of plaque depends on various reasons. The amount of plaque on the tongue increases with a decrease in its self-cleaning, mainly during chewing. When assessing the degree of tongue coating, it is important to take into account the composition and consistency of the food consumed, as well as the regularity of individual hygiene measures and other factors. The amount of plaque on the tongue varies throughout the day: there is more in the morning than in the afternoon and evening, since the amount of plaque decreases after eating. Disruption of the process of normal (physiological) keratinization and desquamation of the epithelium also determines the amount and density of plaque. Thus, with atrophy of the filiform papillae of the tongue, there is little or no plaque. With hypertrophy of these papillae, a hard-to-remove thick layer of plaque is formed on the surface of the tongue, consisting mainly of stuck together keratinized filiform papillae.
The condition of the tongue may indicate disorders of the digestive system. Coated tongue is one of the characteristic symptoms of diseases of the gastrointestinal tract. Thus, with exacerbation of gastritis, peptic ulcer, enterocolitis and colitis, the amount of plaque increases, it covers the entire back of the tongue, localizing mainly in its posterior sections. Plaque formation, as a rule, is not accompanied by subjective sensations. Only with a thick, dense layer of plaque on the tongue can a feeling of discomfort and a slight decrease in taste sensitivity occur. Usually the coating on the tongue is grayish-white in color, but it can take on various shades (yellow, brown). The color of plaque is mainly due to dyes in food products, medications or exacerbations of gastrointestinal diseases: peptic ulcer, chronic hepatitis, cholecystitis (yellow, brown).
A swollen tongue is an important sign of gastrointestinal diseases. As a rule, swelling of the tongue is detected by a doctor during examination, since it does not cause pain, except in cases of significant swelling when biting the tongue when eating or talking. The edematous condition is determined upon examination by pronounced tooth marks on its lateral surfaces, as well as an increase in its size. An objective research method to determine the presence of edema is the McClure-Aldrich blister test. Using a blister test, you can determine the state of latent edema, which will allow you to diagnose early (preclinical) changes. V.A. Epishev (1970) described a violation of hydrophilia of the oral mucosa in chronic gastritis. With anacid gastritis, a decrease was found, and with hyperacid gastritis, an increase in the time of resorption of the blister test was established. It should be taken into account that in which a violation of water metabolism is detected.
Changes in the papillae of the tongue are often recorded in pathologies of the digestive tract. The pathogenesis of these changes is mainly due to trophic disorders, as well as a violation of the vitamin balance due to insufficient absorption and synthesis of vitamins B1, B2, B6, B12 by the intestinal microflora.
Depending on the severity and color of the tongue papillae, hyperplastic glossitis can be differentiated from atrophic one.
Hyperplastic glossitis is observed more often in patients with gastritis with high acidity, with exacerbation of peptic ulcer disease. Glossitis is characterized by hypertrophy of the papillae of the tongue, a dense coating, and an increase in the size of the tongue due to severe swelling.
- Atrophic glossitis is found in gastritis with secretory deficiency, hepatitis, gastroenteritis, colitis. With this form of glossitis, atrophy and smoothness of the papillae of the tongue and the absence of plaque are observed. Sometimes the atrophy of the papillae is pronounced, the tongue is smooth and shiny. It may be hyperemic (erythematous) or pale pink. In some cases, the tongue has a “varnished” appearance with bright red spots and stripes, reminiscent of Meller's glossitis. Atrophy of the papillae of the tongue can cause a burning sensation, soreness, and tingling when eating hot and spicy foods.
Desquamation of the epithelium of the tongue is quite often found in diseases of the gastrointestinal tract and can be of varying degrees of severity. Desquamation occurs more often in patients with chronic gastritis with secretory insufficiency, chronic colitis, and liver diseases. It is characterized by the appearance on the back of the tongue of foci of desquamation of the epithelium of filiform papillae. With secretory insufficiency and infectious lesions of the liver, desquamative glossitis is often combined with atrophy and smoothness of the papillae of the tongue. These changes, as a rule, do not cause painful sensations and patients often do not suspect their existence, only sometimes complaining of burning and pain when eating irritating foods. The appearance of foci of desquamation during an exacerbation of a chronic disease of the gastrointestinal tract and their disappearance during remission are characteristic.
Paresthesia of the tongue often accompanies diseases of the digestive system. There is a burning, tingling, tingling sensation on the tongue. These sensations often accompany desquamative glossitis, but can occur without visible changes in the tongue.
Impaired taste sensitivity is determined by the method of functional mobility of its receptors. It is known that the number of functioning receptors depends on the age and condition of the digestive tract. Normally, maximum activity of taste buds is detected on an empty stomach. After eating, their level of mobility decreases. The reaction of the taste buds of the tongue appears in response to incoming excitation impulses from the receptors of the gastric mucosa in a centrifugal manner. In case of peptic ulcer, stomach tumors, due to a disorder of its secretory and motor functions, the reflex connection between the receptors of the tongue and the stomach is disrupted. This is manifested by various changes in the functional mobility of taste receptors (increased activity and lack of demobilization after eating, etc.). Disturbances in taste sensitivity can also occur with changes in the papillary apparatus of the tongue (heavily coated tongue, atrophy or desquamation).
- Lesions of the oral mucosa
Erosive and ulcerative lesions of the oral mucosa, developing in diseases of the gastrointestinal tract, are predominantly a consequence of trophic disorders. There are a large number of reports on the presence of erosions and ulcers on the oral mucosa due to gastric ulcers, liver diseases, colitis, enterocolitis, etc. There is a known connection between recurrent aphthous stomatitis and gastrointestinal pathology. Approximately 50% of patients with diseases of the gastrointestinal tract (chronic gastritis, gastric and duodenal ulcers) suffer from recurrent aphthous stomatitis of varying severity.
Changes in the color of the oral mucosa can occur against the background of gastrointestinal pathology. During the period of exacerbation of peptic ulcer, enterocolitis, colitis, catarrhal gingivitis, glossitis or stomatitis often develop, the severity of which depends on the duration and frequency of exacerbations of the underlying disease. The oral mucosa in the affected area is characterized by hyperemia with symptoms of cyanosis due to the chronic course of the process. In this case, patients complain of a burning sensation in the mouth, changes in the color of the mucous membrane, and sometimes pain when eating irritating foods. The most pronounced phenomena are catarrhal gingivitis and stomatitis during exacerbation of chronic colitis. During the period of remission of gastrointestinal diseases, the symptoms of catarrhal gingivitis or stomatitis become mild or completely disappear.
It should be remembered that such changes in the oral mucosa can be manifestations of other diseases and conditions of the body (infectious, including fungal, allergic, cardiovascular, hypovitaminosis). In this regard, for successful diagnosis and selection of treatment methods, a thorough examination of the patient is necessary.
Salivation disorders can manifest as hyper or hyposalivation. Studies by a number of authors have proven that patients with gastric and duodenal ulcers experience morphological and functional changes in the minor salivary glands. With peptic ulcer disease in the initial stage (for up to a year), as well as its exacerbation, salivation increases with the subsequent development of hyposalivation. Patients begin to complain of dry mouth. Clinically, impaired salivation is often combined with other previously described changes in the oral cavity, characteristic of gastrointestinal pathology.
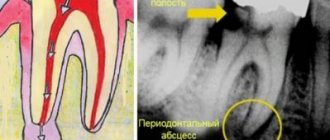
Treatment of the disease
Gastric ulcers are well treated with conservative methods, which include pharmacotherapy and physiotherapeutic procedures. In emergency and some other cases, surgical intervention is indicated.
Drug treatment
The treatment of gastric ulcers uses complex pharmacotherapy, including medications aimed at the root cause of the pathology, relieving irritation of the mucous membrane and creating a protective barrier for gastric juice and relieving pain. The main group of drugs includes:
- Proton pump inhibitors are long-acting drugs that reduce gastric secretory activity.
- Antacids - envelop the mucous membrane, protecting it from the aggressive effects of gastric juice, and reduce its acidity.
- Antibacterial drugs are aimed at eradication (destruction) of Helicobacter pylori. The best effect is achieved when antibiotics are combined. For peptic ulcers, macrolides, antiprotozoal drugs, penicillin and tetracycline antibiotics are prescribed.
- Bismuth preparations relieve inflammation and form an insoluble colloid that creates a protective film when combined with protein.
- Vitamin B5 (Pantothenate) - normalizes the production of hydrochloric acid, stimulates the regeneration of the mucous membrane.
- Methylmethionine sulfonium chloride, also called vitamin U, acts as a cytoprotector that helps reduce gastric secretion and heal gastric ulcers.
Treatment can be supplemented with other drugs aimed at eliminating the causes of ulcerative pathology.
Physiotherapy
Physiotherapy helps ulcer healing and can be used in complex therapy. The mechanisms of self-regulation and adaptation are beneficially affected by:
- laser puncture - exposure of bioactive points with a laser beam;
- EHF therapy - the influence of electromagnetic waves in the millimeter range;
- magnetotherapy - exposure to low-frequency magnetic fields.
Ultrasound therapy is used to improve gastric motility in case of gastric atony. This procedure also improves blood supply to the organ, reduces the number of bacteria and relieves inflammation.
Surgery
Emergency surgery is performed in case of massive bleeding and perforated gastric ulcer. Surgical intervention is also indicated for complicated forms of ulcers in the case of a non-healing ulcer, as well as for malignancy, when the pathology becomes malignant. In some cases, gentle methods are used: laparoscopy or endoscopy.
specialist
Our doctors will answer any questions you may have
Tumasova Anna Valerievna Gastroenterologist
Diet and bad habits for stomach ulcers
Diet for gastrointestinal ulcers is an essential part of treatment. During the acute period, nutrition should be as gentle as possible, gentle on the mucous membrane and not stimulating the secretory activity of the stomach. In the first two days, preference is given to slimy soups with rice water without vegetables and meat, jelly or warm tea with sugar and crackers. In the next 6 days, table No. 1 is used in therapeutic nutrition.
Authorized Products
General nutrition rules:
- include easily digestible foods in the diet;
- food should be warm
- Do not eat cold or hot foods;
- you need to eat slowly, in small portions
- products need to be crushed and ground;
- Baking, boiling, stewing is allowed;
- fried foods and spices are excluded;
- the break in eating should not be more than 3 hours;
- food must be chewed thoroughly.
The following foods and dishes are allowed for stomach ulcers:
- Slimy soups: with the addition of rice, semolina, oatmeal, you can add cream or butter;
- Slimy porridges: with water or milk from the same cereal, you can add cream;
- Fish and meat: lean beef, veal, turkey, rabbit, chicken. To prepare the meat, you need to boil it, pass it through a meat grinder, add butter, bake it into a soufflé puree, you can cook steamed cutlets, meatballs, meatballs;
- Eggs: soft-boiled, or steam omelet;
- Berries and fruits: baked unsweetened fruits, dried fruit compotes;
- Dairy products: milk, steamed pureed cottage cheese soufflé, cream.
- Drinks: weak tea with added cream or milk, rosehip decoction, milk or fruit jelly.
You can add refined vegetable oil or unsalted butter to dishes.
Prohibited Products
During an exacerbation, foods that irritate the gastric mucosa and increase the production of gastric juice are excluded: fatty meat, baked goods, preserves, canned and smoked foods, confectionery with cream, dishes with vinegar and spices, garlic.
Do not include vegetables with coarse fiber in the diet, as well as radishes, radishes, daikon, cabbage, tomatoes, turnips, and mushrooms.
It is necessary to avoid foods that cause fermentation processes: legumes, sweet fruits and juices, carbonated drinks.
During the treatment period, you are strictly prohibited from smoking and drinking alcohol.
Is my tongue my doctor? What diseases can be identified by the organ of taste?
The tongue is one of the most important organs in the body. It contains receptors that allow you to recognize all shades of taste of products entering the oral cavity.
As scientists noted back in ancient times, human language has a connection with various organs of the body. When diagnosing, they divided it into conventional parts: basal, middle and tip. And they believed that in case of pathology of a particular organ, the lesion would be observed strictly in one of these areas. AiF.ru looked into what diseases leave their mark on the language together with Professor, Doctor of Medical Sciences, head of the laboratory for the development of an interdisciplinary approach to the prevention of chronic non-infectious diseases of the Federal State Budgetary Institution "State Research Center for Preventive Medicine of the Ministry of Health of Russia", expert of the National Health League Mehman Mamedov .
Color spectrum
When examined by a doctor, you are often asked to show your tongue. And they do this not out of idle curiosity. After all, even by the color of the tongue it is quite possible to determine whether there is a particular disease. For example, the tongue of a healthy person should be pale pink: this is what is accepted as the norm. If there is a white coating on the tongue, we can talk about fungal infections of the body or disorders of the gastrointestinal tract. A gray tongue is usually the result of chronic pathologies. Bright red - will indicate infectious and inflammatory processes in the human body; if the red color has a shade of scarlet, doctors will suspect problems with the circulatory system. A burgundy tint is a clear sign of an acute infectious process. The tongue is part of the gastrointestinal tract, and is also connected with the respiratory system, because located in the oral cavity. With stomach and duodenal ulcers, problems with the gallbladder, liver and intestines, there may be changes in the color of the tongue. Each disease has its own manifestations - in some places it can be more contrasting, in others it can be lighter.
It also happens that the color of the tongue changes to blue and purple. In this case, they talk about problems with the lungs or severe kidney ailments. Yellowing of the tongue is not only a characteristic feature of a heavy smoker, but also a signal of problems with the gastrointestinal tract. If there is a lack of vitamins in the human body, the tongue may completely lose color.
It is worth considering that a shade that is too dark and saturated is a sign of problems that require immediate medical intervention, or even hospitalization.
Additional factors
However, not only color matters. If the tongue is too dry, the following diagnoses may be made: dehydration, intestinal obstruction, peritonitis. Often, dry tongue is observed with an increase in body temperature. If the situation approaches critical, the taste organ may even crack due to dryness. In this case, an additional threat is created: it is easily infected with bacteria, resulting in suppuration and severe inflammation.
The type of coating on the tongue is also of particular importance. So, if it is thin, it means that the disease is in the initial phase, and if it is frankly fatty and thick, then the problem most likely lies in pathologies of the gastrointestinal system: this usually happens if mucus has accumulated there and food stagnates. A spotted and purple coating indicates the development of blood stagnation. Malfunctions in the digestive system will cause the tongue to become slightly swollen and wet. In this case, it is recommended to be checked for gastritis, cholecystitis, ulcers and even appendicitis.
Doctors pay special attention to the place where plaque accumulates. So, if it is more adjacent to the root of the tongue, then problems are noted in the large intestine: most likely, many human waste products have accumulated there and cannot find a way out. Plaque in the middle indicates problems in the small or duodenal intestine or stomach. If the plaque is so thick and the tongue is so swollen that you can see teeth marks along the edge, you need to reconsider your diet: with a high degree of probability it can be said that the intestines cannot cope with the food that a person eats.
The presence of deep wrinkles and cracks located transversely should alert you and send you to a neurologist - as a rule, this problem manifests itself with a predisposition to vascular disorders of the brain.
The tongue can even indicate serious cardiac and vascular problems, which may occur without any symptoms for some time. For example, a tongue that is slightly shifted to the side or slightly bent will indicate a hemorrhagic stroke, cerebrovascular accidents, or problems with the functioning of the cerebellum.
An increase in the volume of the taste organ may be a consequence of problems with the thyroid gland, malfunction of the pituitary gland, or mental disorders.
Shaky and grainy
Sometimes a person may notice that his tongue... trembles. This condition indicates nervousness and problems with the central nervous system. In such a situation, doctors recommend changing the psychological environment, as well as working on your lifestyle. It is also worth checking with a doctor if your sense of taste begins to decrease. After all, it does not develop out of the blue: there must be a reason why a person no longer feels the tastes to which he is accustomed. Moreover, it is important to understand that there are certain zones and areas on the tongue that are responsible for the reaction to different tastes: spicy, salty, sweet, etc. If a malfunction is noted in any of the parts, this may indicate that the nervous system is suffering. or endocrine system. Loss of taste in the taste buds of the tongue manifests itself as a result of metabolic disorders in the human body, as well as malfunctions of the central system of various etiologies, the development of anemia and the presence of cancer.
Also, people often begin to notice that the tongue has become rougher: this is due to an increase in the size of the papillae on the surface of the organ. When swollen papillae are localized at the tip, it is worth being examined by a cardiologist. If the tongue becomes “spiky” around the edges, you need to check the liver. An affected middle part of the tongue indicates problems in the stomach and intestines. At the same time, you should not rejoice when the tongue becomes smooth and “mirror-like”. After all, this is also a pathology. This happens with anemia, exhaustion or severe pathologies of the stomach.
Prevention of peptic ulcers
Stomach ulcers can be avoided if you follow some rules. First of all, give up bad habits, since ethyl alcohol and tobacco reduce the protective properties of the mucous membrane and irritate it.
Diet is no less important in prevention: you need to eat at a certain time, the interval between meals should not exceed 4 hours. You cannot eat dry food, as dry rough food injures the walls of the stomach.
For those who work at night, it is recommended to change jobs to work only during the daytime. It is necessary to avoid stress, treat inflammation of the stomach, hormonal diseases, and visit a gastroenterologist at least once every six months.