To understand what allergic stomatitis , it is necessary to clarify two concepts.
Allergy. An excessive protective reaction of the body's immune system to certain external substances foreign to the body, called allergens. These may be substances that are essentially harmless to humans, but for some people (allergy sufferers) they are perceived by the immune system as dangerous to the body. In immunology, there are several types of allergic reactions, but in practical allergology only type I (fast or instant reaction) and type IV (slow or delayed reaction) are relevant. These types of reactions in the body can occur separately, but they can also occur in parallel. In addition, symptoms similar to those of allergies can be caused by other pathologies, for example, pseudoallergic diseases, conditions of intolerance to certain substances.
Autoimmune diseases. A generalized medical term for pathologies that are based on an excessive reaction of the immune system to the body’s own tissue elements (fragments). That is, the immune system recognizes these elements of the body as foreign and triggers a chain of defensive reactions, leading to severe inflammation and pathologies of various internal organs.
Allergic reactions and autoimmune pathologies can manifest themselves on the oral mucosa and the generalized term allergic stomatitis .
Unfortunately, the relative number of patients with symptoms of allergic stomatitis has recently increased. This is due not only to the fact that the ecology of the external environment is deteriorating or new potentially allergenic components appear in food products. It is believed that a significant contribution is made by the emergence of new and diverse materials used in dental treatment - filling materials, materials for dental crowns and dentures, for the manufacture of braces and implants, various mouth rinses, etc. At the same time, new materials often do not go through the research stage for the risk of allergic reactions. allergic stomatitis may appear and children.
Symptoms of allergic stomatitis
The symptoms of allergic stomatitis are essentially no different from the symptoms of stomatitis of other nature. This is redness of the oral mucosa, swelling and rashes of various types, which can be localized both in the mucous membrane and affect the soft tissues of the oral cavity. In this case, erosions, ulcers, a burning sensation and pain in the mouth, and loss of taste are possible. Some types of allergic reactions, for example to pollen, may be accompanied by aphthous stomatitis, but it goes away after the plants finish flowering.
Prevention
If a patient once experiences allergic stomatitis, there is a high probability of it developing again. To prevent pathology, you need to pay attention to the following points.
- Immunity.
To strengthen the immune system and general health, it is recommended to take a course of comprehensive vitamin intake. - Nutrition.
It is better to exclude allergenic foods and hot spices from food and create a balanced menu. - Medicines.
When taking strong medications, especially antibiotics, it is necessary to include antihistamines, that is, antiallergic agents, in the list of medications. - Oral care.
If a toothpaste, brush or mouthwash causes discomfort, irritation or itching, you need to change the products yourself or choose the right ones together with your dentist.
The risk of developing allergic stomatitis and other diseases is minimal if you visit the dentist every six months for the prevention and timely treatment of pathologies in the early stages!
Classification of allergic stomatitis
There is no generally accepted classification of allergic stomatitis, and a classification based on the sources (triggers) of the allergic reaction is usually used. The following types can be roughly distinguished.
Stomatitis in patients suffering from general allergic reactions. For example, people who have an allergic reaction to pollen may experience an allergic reaction in the mouth (so-called cross-allergy) when eating certain foods. Another example is an allergy to latex, and the appearance of symptoms of allergic stomatitis when the oral mucosa comes into contact with gloves containing this component. These reactions are usually Type I (rapid or immediate reactions).
Contact allergic stomatitis. Sometimes the term is used - allergic contact eczema of the oral mucosa. Allergic contact stomatitis is a non-infectious inflammation of the oral mucosa, usually associated with a type IV immune reaction. Caused by prolonged and constant contact with various materials used in dental (therapeutic, orthopedic, orthodontic) treatment. The active principle is the various components of the materials used. Among them are metals (nickel - most often, gold-containing alloys, palladium, mercury compounds in amalgams, cobalt). Other options are filling materials (especially light-curing ones when polymerization is not deep enough, leading to the gradual release of residual monomer), materials for removable prosthetics (possible release of acrylates), materials for dental impressions. Hypersensitivity to such materials often leads to the gradual development of an allergic reaction in the oral cavity after treatment by a dentist. In such cases, treatment of allergic stomatitis involves removing its source.
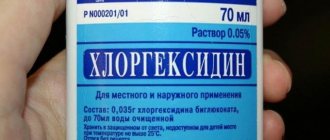
Toxic stomatitis. Usually associated with an allergic reaction to components of various products used to prevent dental diseases. Among them are various mouth rinses containing essential oils and preservatives. Damage to the oral cavity due to an allergic reaction to certain medications used in dental practice (perborate solutions, eugenol, preparations for dental fluoridation, sodium hypochloride, etc.) can also be attributed to this type.
Diagnostics
First of all, a visual examination is carried out: the dentist assesses the condition of the mucous membrane, looks for the presence of dentures, fillings and other materials that could become allergens. Then the doctor finds out the time of the first signs of the disease, the patient’s general well-being and possible factors of the disease: heredity, allergies, medication, diet, trips to other countries, contact with animals and insects. If allergic stomatitis is confirmed, tests are performed to clarify the allergen:
- study of the composition of saliva;
- sample from dentures or dental materials;
- immunogram;
- blood and urine tests.
Autoimmune stomatitis
Some autoimmune diseases can lead to the appearance of stomatitis, and this type of stomatitis can be conditionally classified as stomatitis of an allergic nature. In some cases, the mechanisms of damage to the oral cavity against the background of a general disease remain unknown; some authors classify them as allergic dermatostomatitis. These types of diseases that cause damage to the oral cavity include chronic recurrent aphthous stomatitis (the exact nature is unknown, but the disease is considered a specific allergic reaction to pathologies of the gastrointestinal tract), lupus erythematosus, exudative erythema multiforme, lichen planus, scleroderma, pemphigus and similar pathologies with them.
Request a consultation
What it is
Allergies can arise in a person out of nowhere, in the complete absence of any reactions to food, medications, dust, pollen and other irritants in the past. This happens due to failures of the immune system, as well as changes at the genetic level. Blood cells responsible for the formation of antibodies to infections at some point perceive a substance that has entered the body as an “enemy” of the immune system. A response begins, which is accompanied by typical allergy symptoms.
A person can calmly eat honey for half his life, drink chamomile tea, and be treated with penicillin. And at one point, any component of normal life can become a strong allergen, which can lead to a powerful reaction, anaphylactic shock and even death. Approximately a third of the world's population is susceptible to one or another manifestation of allergic reactions, and on average, in 20% of this number, allergies manifest themselves as rashes on the oral mucosa. So if you are faced with stomatitis, allergies may be one of the reasons for its occurrence.
Nutritional Features
Due to the fact that painful ulcers appear in the mouth with stomatitis, any meal gives the baby discomfort. Therefore, the diet during the period before recovery should have a number of features.
- All food taken should be warm and at a temperature as close as possible to body temperature. This will prevent unnecessary irritation and will not cause acute pain.
- Since chewing is quite painful, portions should be reduced by about a third, but the frequency of meals should be increased.
- When feeding your baby, you should give preference to dishes with a soft consistency, and it is better to postpone dense and dry foods until complete recovery.
- It is worth giving preference to products with a neutral taste. These are potatoes, bananas, pears, pumpkin.
- Until recovery, spicy, salty and sour foods are completely excluded from the child’s diet.
- To make eating less painful, you can purchase thick straws for cocktails and crush all food so that it can be drunk.
- The emphasis is on healthy foods rich in microelements and vitamins. For example, buckwheat, oatmeal, and rice can be recommended for cereals. It is preferable to give your baby cauliflower and broccoli as vegetables.
Bacterial stomatitis in children
Necrotizing ulcerative stomatitis is more common in weakened children and is caused by fusobacteria and spirochetes. May be a sign of periodontal disease (progressive destruction of periodontal tissue). It is characterized by the appearance of painful ulcers, weakness, gingivitis (inflammation of the gums), enlarged and painful lymph nodes, difficulty eating, speaking, and bad breath.
Often, erosions in traumatic stomatitis can become infected through dirty hands, toys and other objects, then bacterial stomatitis develops, so it is important to pay attention to antiseptic treatment.
Treatment
The main method of dental intervention is replacement of dentures. Ceramics are best suited for fixed dentures. This is a bioinert mass that does not cause allergies. Ceramic dentures make it possible to choose the material to suit your budget. Porcelain structures are cheaper than glass-ceramic ones (E-max, Empress), and they, in turn, are cheaper than zirconium ones. If it is not possible to install ceramics, then you need to select an alloy that excludes metals that cause allergies.
If you are allergic to removable dentures, the composition is also changed. Acrylic is replaced by nylon and Acry-Free polymer.
But in clasp structures you cannot do without metal. Ideally, it would be good to replace the arc and fasteners with inert metals: gold, platinum, titanium. In other cases, dentistry selects a composition that does not contain metals that were in the previous restoration. Another option may be to install a Quadrotti prosthesis. The material of construction is relatively hard thermoplastic. Clasps are also made from it. The absence of metals reduces the risk of allergies.
Anti-allergy treatment (antihistamines) is carried out against the background of dental procedures.
How many days do people suffer from stomatitis and what to do at the first signs of it?
How long does stomatitis last? This question is of great concern to parents of sick children, since all the symptoms of the disease are unpleasant and cause discomfort to the child.
The duration of the disease depends on its form. Acute variants of stomatitis with adequate drug treatment resolve within 14 days.
If the disease does not go away for a month or more, then they talk about the chronic course of such a pathology. In this case, it is possible to alternate periods of subsidence of clinical symptoms and their exacerbation - recurrent stomatitis.
If you suspect signs of stomatitis in your child, you should urgently consult a doctor who will tell you how to numb the mucous membrane and prescribe comprehensive treatment. If it is not possible to visit a doctor as soon as the first symptoms of the disease begin, then it is possible to independently numb the mouth with local drugs (Dentinox, Kalgel). And you can’t delay medical consultation!
Establishing diagnosis
If there is a suspicion that the patient has allergic stomatitis, he must be examined by a dentist. If necessary, allergists, immunologists, dermatologists, endocrinologists, gastroenterologists, rheumatologists and other specialized specialists are involved in the diagnosis. The attending physician must collect a detailed medical history to understand what caused the disorder and what substance acts as an allergen.
During an examination of the oral cavity, the dentist observes reddened and swollen mucous membranes. In some places, round ulcers are visible on it, covered with a white or gray coating. Saliva is usually very thick.
The specialist pays attention to the condition of the existing prostheses and finds out how long ago they were installed. To study the electrochemical processes occurring in the oral cavity, a saliva test is taken from the patient. It is important to determine the pH of biological material and evaluate the content of microelements in it. Allergy diagnostics involves conducting special tests - skin tests, provocative tests, etc.
If allergic stomatitis is suspected, it is important to differentiate it from a deficiency of vitamins C and B, herpes, candidiasis, leukemia, and HIV. With all these diagnoses, changes in the structure of the oral mucosa are also observed.
Types of childhood stomatitis and their main manifestations
The classification of childhood stomatitis is based both on the cause of the disease and on some distinctive features in the clinical course of such pathology. We will tell you how to determine this or that type of disease in our article later.
Catarrhal stomatitis
It is the mildest and most common form of the disease. In this case, multiple inflammatory foci appear on the mucous membrane of the gums, cheeks or lips, covered with a whitish coating, but without the formation of aphthae or ulcers. In this case, the child will complain of pain in the mouth when eating, drinking or talking, increased salivation, bad breath, and general weakness.
With catarrhal stomatitis, the mucous membrane is very susceptible to injury and bleeding, even during normal activities: brushing teeth, eating. When inflammatory foci are localized only on the gums, the clinical picture of stomatitis will resemble gingivitis.
Ulcerative stomatitis
The ulcerative form is a consequence of untreated catarrhal stomatitis. In this case, against the background of edematous foci of redness, multiple ulcerations are formed, which gradually increase in size, spread deep into the tissue of the mucous membranes or merge with each other.
The child complains of severe pain in the oral cavity, which intensifies when trying to brush his teeth or eat, and the smell of his breath becomes putrid. General health worsens: body temperature rises, weakness and body aches occur.
Young children are capricious, refuse to eat, and have trouble sleeping.
Gangrenous stomatitis
The gangrenous form of the disease is a continuation of catarrhal and ulcerative forms. A characteristic sign of this pathology is the spread of the inflammatory process deep into the tissues of the jaw with the development of extensive necrosis, which can involve the bones and spread to other anatomical areas.
The condition of a child with gangrenous stomatitis is extremely serious. There may be disturbances of consciousness, severe weakness, and the smell of rotting meat from the mouth. Regional lymph nodes are enlarged and painful on palpation.
Candidiasis (fungal or milk) stomatitis
Candidal stomatitis is characterized by specific symptoms. At the onset of the disease, children have dry mouth. Subsequently, a burning sensation and an unpleasant aftertaste appear. A white coating in the form of small dots is deposited on the mucous membrane. As the process progresses, the points merge into a large lesion that resembles a curdled mass. Such plaque is difficult to remove, exposing the inflamed surface of the mucous membrane.
Fungal stomatitis often occurs without fever, and the general condition is little affected.
Infectious stomatitis
The phenomenon of stomatitis can also be observed in some infectious diseases. With scarlet fever, the typical picture on the mucous membranes of the mouth will be supplemented by specific manifestations of the disease: a pinpoint rash on the skin and a “crimson tongue” - the surface of the tongue is bright red, shiny with hypertrophied papillae.
With diphtheria, damage to the gums will be combined with the detection of dense grayish films on the tonsils or in the throat. In this case, a paroxysmal cough with episodes of suffocation will be noted.
Allergic stomatitis
The allergic form of stomatitis most often affects children over 4 years of age. It is characterized by a clear connection with the action of the allergen, a rapid increase in symptoms and their rapid extinction with adequate treatment. The clinical picture in this case is similar to the ulcerative version of the disease - ulcers or aphthae form on the mucous membranes, covered with a whitish coating and surrounded by a focus of redness. Quite often, this pathology occurs in the form of chronic stomatitis with periodic episodes of exacerbation.
Traumatic stomatitis
In cases of mechanical trauma, a significant focus of infiltration appears on the mucous membrane, which ulcerates as the inflammation progresses. When burned by hot drinks, a bubble often appears, after opening which a fairly deep ulcer is exposed. A distinctive feature of the traumatic form of the disease is a clear connection with trauma or thermal burn of the oral mucosa and the formation of a single lesion.
In case of severe inflammation, local symptoms may be accompanied by general symptoms: fever, malaise, headache.
Herpetic stomatitis
In herpetic stomatitis, the main morphological element is small blisters located against the background of a hyperemic mucous membrane. They quickly open and erosions form, which are covered with fibrous plaque. The lesions can be localized separately or merge into a single affected area.
Erosion is extremely painful, the child refuses to eat, is capricious, sleep is disturbed, and in severe cases there is a significant increase in body temperature. In this case, typical herpetic lesions can be found not only in the oral cavity, but also on the face or other parts of the body.
Bacterial (purulent) stomatitis
Most often, bacterial stomatitis appears due to constant improper oral care or microbial sore throat. The clinical picture is typical for stomatitis: initially foci of inflammation appear, which then transform into deep ulcers covered with abundant purulent plaque.
At the same time, purulent deposits on the tonsils are detected, the child’s general well-being suffers, body temperature often rises significantly, and the cervical, submandibular and clavicular groups of lymph nodes enlarge.
Vesicular stomatitis
Vesicular stomatitis is an infectious disease. Its causative agent is vesiculovirus, a virus transmitted from sick animals to people. The incubation period of this disease is 5-6 days, during which children may complain of fatigue, weakness, and slight chills. Subsequently, small painful blisters with whitish contents appear on the mucous membranes of the oral cavity. Similar elements appear in the area of the feet and hands.
The general symptoms are very similar to a banal acute respiratory infection: the body temperature rises, there may be signs of rhinitis and conjunctivitis. If the intestines are damaged, there may be dyspeptic symptoms: diarrhea or constipation.
Fighting the disease
What therapeutic regimen the doctor will offer the patient depends on the cause of the disease and the type of provoking factor. The first thing to do is to completely eliminate contact with the allergen. But to do this, you must first establish what exactly this allergen is. If there is no answer to this question, the patient is asked:
- stop taking medications he was previously using;
- follow a strict diet;
- change your toothbrush and toothpaste;
- stop wearing dentures.
In this way, the doctor tries to eliminate the influence of the most common allergens.
Drug therapy involves the patient taking antihistamines. They are always used for allergies. The use of vitamin-mineral complexes is also indicated. It is especially important that they contain folic, nicotinic and ascorbic acid, and B vitamins.
Affected areas should be treated regularly:
- special dental anesthetics;
- corticosteroid gels;
- enzyme compounds;
- drugs that accelerate regenerative processes.
If stomatitis is a consequence of recent dental treatment, you should consult a dentist again as soon as possible. It is possible that you will have to replace the installed fillings and crowns.
Among the folk methods that are effective for stomatitis, rinsing with cabbage juice, aloe infusion, diluted sea buckthorn oil, and chamomile decoction help. You can also apply grated raw potatoes to the wounds.
Treatment of allergic stomatitis in adults and children is carried out according to the same scheme. The only difference is in the medications prescribed: not all formulations for adults are suitable for children, and vice versa.
Manifestations of the disease
The disease negatively affects the functioning of the entire body. It doesn’t just cause inflammation of the mucous membranes—it also causes migraines, elevated body temperature, and lethargy. Many people notice dry mouth, severe pain when chewing, which is present even when the integrity of the tissues has not yet been compromised.
Saliva thickens, becomes viscous, more like foam. The gums, tongue, and inner surface of the cheeks may swell. All these symptoms deprive the patient of the opportunity to lead a normal lifestyle.
You shouldn’t wait for the disease to clear up. The sooner her treatment is started, the sooner her health will be normalized.
Possible complications
The prognosis for the disease is usually favorable. However, incorrect or untimely treatment can lead to the development of complications:
- The addition of a secondary bacterial infection, accompanied by a worsening of the sick child’s condition.
- Sometimes severe necrotizing forms of stomatitis lead to osteomyelitis - destruction of the bone tissue of the jaw.
- Persistent or frequent stomatitis can provoke the loss of teeth from both the primary and permanent sets.
- The presence of a chronic purulent inflammatory focus in a child’s body negatively affects the state of immunity, and also, under the influence of unfavorable factors, can lead to blood poisoning - sepsis.