Filling is a complex of dental procedures, including the removal of tooth tissue destroyed by caries, disinfection and treatment of the resulting cavity with adhesive preparations, placement and grinding of a dental filling.
Normally, after performing the above procedures, the patient should not experience discomfort or pain. For this reason, the appearance of any unpleasant sensations in the area of a filled tooth is an absolute reason for a return visit to the dental office.
Causes of tooth pain after filling
Pulpitis
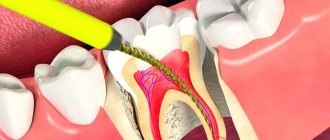
The appearance of acute, spontaneous pain that grows and intensifies at night in a filled tooth may be due to the development of chronic or acute pulpitis. If such symptoms are detected, it is necessary to contact a dentist as soon as possible to remove a previously placed filling, remove the inflamed pulp, fill the root canals and the carious cavity itself.
Development of secondary caries
The source of pain in the tooth after filling can also be secondary caries, which gradually develops under the filling. The most common causes of this pathology are:
Causes of secondary caries
- insufficient disinfection of the carious surface before placing a filling;
- displacement of the installed filling under the influence of external factors;
- shrinkage of the filling material, which contributes to the formation of gaps between the filling and dental tissues;
- injury resulting in damage to the filling;
- irregular oral hygiene;
- violation of filling technology.
Treatment of secondary caries
When a secondary caries process is detected, the dentist removes the previously placed filling, cleans the resulting cavity from destroyed tissue, disinfects it and re-fills the tooth.
Underdrying or overdrying of the cavity
The causes of spontaneous pain that increases with biting in a treated tooth may be under-drying or over-drying of the tissues before filling. Before applying adhesive preparations, the surface dental tissues must be dried to a “wet sand” state (that is, the surface must remain wet, but there cannot be drops of water on it).
Consequences of overdrying tissues
Overdrying of dental tissues leads to damage to the nerve endings located in the surface layers of dentin. In turn, the death of nerve fibers can cause inflammatory damage to the pulp and other serious complications. Mild pain caused by overdrying of the carious cavity most often goes away on its own within 5-13 days. In situations where pain intensifies or persists for two weeks, patients are advised to return to the dental clinic for help.
Consequences of not drying the cavity
Failure to dry out the treated carious cavity can also cause pain. Drops of moisture prevent the penetration of adhesive preparations into the dentinal tubules, therefore, when the filling material shrinks, the composite easily comes off from the cavity floor, thereby forming pathological sinuses in the dental tissues. The only way out of this situation can be to replace the previously installed filling.
Granuloma or dental cyst
One of the likely causes of tooth pain after filling may be the formation of a granuloma (a localized area of inflamed tissue) or a root cyst (a pathological cavity in the gum tissue filled with bacteria, dead cells, blood and other physiological fluids). Granulomas and cysts are treated both conservatively (for example, using the depophoresis method) and through surgical intervention (cystectomy, hemisection, etc.).
Allergic reaction
In some cases, pain in a filled tooth can be the result of an allergic reaction to the components of the filling material. The clinical picture may be supplemented by urticaria, the appearance of an itchy rash and swelling on the patient’s skin and mucous membranes. If a patient is diagnosed with an allergy to the material used, the filling is immediately replaced.
Plaque - symptoms and treatment
With regular visits to the dentist, dental plaque is detected at the initial stage and is easily removed. It is recommended to carry out hygienic teeth cleaning once every six months. If the plaque is not removed, it turns into a dense formation and caries develops. With timely consultation with a doctor and proper treatment, the prognosis will be favorable. In case of acute caries, you should visit the dentist 2-4 times a year, treat the oral cavity with chlorhexidine, eat less carbohydrates and monitor the microbiological parameters of saliva every 2-3 years.
Preventive examinations, timely treatment, and removal of plaque significantly improve the health of the oral cavity and prevent the development of diseases of the gums and teeth, but without satisfactory self-hygiene it is impossible to achieve favorable long-term results [7][9][15].
The very first thing in hygiene and plaque control is a toothbrush . It is selected individually, according to the anatomical characteristics of the patients. When choosing and using, consider the following main points:
- Brushes with artificial bristles with rounded ends are preferred. Natural bristles, as a rule, are quickly colonized by bacteria; moreover, they are short-lived, and the sharp ends of the bristles can injure the gums and hard tooth tissues.
- The coverage of the bristles is no more than two or three teeth, this will allow you to clean them better.
- The handle fits comfortably in the hand.
- Toothbrushes are changed every 6-10 weeks.
Electric brushes with rotating or oscillating heads are recommended for patients with impaired manual skills. They remove plaque well with constant use.
toothpaste plays an important role It should clean well, not damage the enamel, taste good, and protect against germs for a long time. The following compounds are important in its composition:
- fluorides (fluorine compounds, for example with sodium) - stabilize the level of minerals in tooth enamel;
- pyrophosphate, zinc chloride, zinc citrate - reduce supragingival tartar;
- strontium chloride, hydroxyapatites and potassium nitrate - relieve hypersensitivity of teeth;
- calcium carbonate - neutralizes acids, thereby protecting teeth [2][3][8].
, dental floss (floss) and threads on a holder (flossets) will be useful . They easily penetrate into the interdental spaces and remove food debris and plaque.
Patients with implants should use interproximal brushes . They consist of a spirally curved base with conically or cylindrically arranged bristles. Dental floss and interproximal brushes are for single use only.
To remove food debris, you can use wooden or plastic toothpicks, but remember that they will not get rid of plaque.
If you have fixed structures (braces, crowns, implants), an irrigator - a device that uses a jet of water under pressure to clean the tooth surface and massage the soft tissues.
Mouth rinses In case of chronic periodontal diseases, rinsing your mouth is not recommended - this increases the risk of particles of infected deposits getting into the gum pocket and can increase inflammation.
Chlorhexidine is an antiseptic that has an antibacterial effect and reduces dental plaque. But due to the side irritant effect (up to a chemical burn of the papillae of the tongue with impaired taste sensitivity), the course of chlorhexidine in the mouthwash is limited to two weeks, repeated after three months.
Chewing gum for 15-20 minutes after eating mechanically cleanses the teeth by increasing salivation. Chewing gum should be chosen without sugar and with xylitol, a sweetener that prevents the growth of bacteria in the oral cavity.
One of the important factors in the prevention of dental plaque is nutrition . To prevent tooth decay, it is important to get enough minerals (calcium and fluoride) from food and reduce the amount of sugar. You should also avoid smoking and reduce the consumption of coloring products - black coffee or tea [2][3][8][10].
Recommendations for eliminating the causes of pain in a filled tooth
If you experience discomfort or pain in a filled tooth, it is recommended:
- eliminate the load on the diseased tooth;
- seek professional dental care immediately;
- stop using traditional medicine.
Procedures related to filling replacement, removal of granulomas and cysts are performed on an outpatient basis and do not require much time.
At the same time, timely seeking dental care at a 24-hour dentistry allows you not only to get rid of unpleasant symptoms in the shortest possible time, but also to prevent the development of serious complications.
Fillings that destroy teeth
Most people, in fact, do not even remember when and which tooth was treated and turn to the dentist only when the old filling breaks or falls out.
It is believed that modern “light” fillings are the pinnacle of modern dentistry technology, a quick and reliable way to restore even severely damaged teeth.
However, it is not.
Even the most modern filling is a polymer. In essence, it is a technologically advanced type of plastic that is matched to the color of the tooth and cured with light. There are filling materials of different properties, some are more aesthetic, some are more durable, and so on. But at the core, each filling remains a piece of plastic.
And everything would be fine if it weren’t for the hopes for “eternal life” that we place on this miracle of modern dentistry.
Demand always creates supply. Unfortunately, this also applies to dentistry: When a patient comes to the doctor with a broken tooth, the patient asks the doctor to carry out all the treatment quickly, efficiently and with a guarantee.
And if you manage to save money, it will be absolutely wonderful!
All filling materials have significant limitations in their use and service life.
- The size of the filling cannot exceed 50% of the chewing surface of the tooth - even the strongest fillings cannot fully withstand the chewing load, which in an adult can reach 150 - 200 kilograms.
- The filling can be hermetically glued only to that part of the tooth on which there is enamel - often due to exposure of the roots, people develop sensitivity in the necks of the teeth and wedge-shaped defects are formed. It is important to know that in these cases fillings cannot be placed, but other treatment is necessary.
- Only a living tooth can be restored with a filling. When the tooth has been depulped (removal of the nerve) and the canal is hermetically sealed, this tooth needs increased protection, because to access the nerve it is necessary to create a deep cavity in the tooth. This access breaks the tooth frame. In this case, it is imperative to strengthen the tooth with ceramic restoration. Without such protection, the tooth will break due to a chip or crack.
- The seal has a limited service life. On average, every 3-5 years the filling must be replaced due to wear and loss of tightness. Microbes begin to get under the filling and Secondary caries is formed in the tooth - this is a carious process that occurs under the existing restoration. Such a process can develop asymptomatically for a long time, revealing itself only as a darkened filling on the tooth. But in fact, this darkening is tooth decay. Often such destruction leads to tooth loss; the process goes under the gum.
- Fillings disrupt the bite - this is due to the fact that when treating a tooth using filling materials, it is not possible to fully restore its morphology (the anatomical shape of the chewing cusps of the tooth). This leads to incorrect distribution of loads when closing the jaws. Some teeth begin to wear out faster and become overloaded. Ultimately, overload can lead to jaw displacement and/or injury to the temporal joint.
What to do? The answer is simple - get treatment correctly!
To do this, you do not need to graduate from a medical university on your own.
It is important to remember a few rules:
- If you have large fillings, they need to be replaced with ceramic onlays and restorations. This will protect your teeth and bite. It will also restore the beauty of your smile. Today there are even “Crown in an hour” technologies that allow such treatment to be carried out as quickly as possible.
- Do not place fillings near the gums, as they cannot be sealed there. Gum recession is treated by gum grafting (microsurgical treatment).
- Promptly undergo a dental check-up with an inspection of fillings. The inspection is carried out using a special contraster that detects a violation of the tightness of the seals.
- In order for the filling to be installed correctly, the doctor must use a rubber dam to isolate the tooth from saliva and moist air. Before installing the filling, the tooth surface is checked using a caries detector and treated with a special sandblasting machine to enhance the adhesion of the filling. If root canal treatment of a tooth is necessary, you cannot do without a dental microscope and 3D x-ray.
- Regularly undergo preventive examinations with a personal hygienist and follow the recommendations.
Health is the main treasure we have. You need to trust it to professionals who treat each patient with due care and attention.
Smirnov D.V. Ph.D.
Classification of the disease
Depending on the severity of the pathology, the following forms are distinguished:
- Streaked – characterized by the appearance of small stripes or streaks on the surface of the tooth. The upper jaw is most often affected by this form. The stripes are faint and cannot always be seen independently. Over time, they merge into one spot, in which strokes can also be distinguished.
- Spotted - this form is characterized by the presence of multiple chalky spots. They are well defined and located on the entire surface of the tooth. When drained, large spots form.
- A chalky-altered form - it is characterized by the presence of an affected light brown area, which turns into healthy enamel. This lesion is most often observed on the upper and lower incisors.
- Chalky-mottled - characterized by the presence of clear pigment spots. Sometimes there may be a variant of the presence of multiple dots on the enamel of a yellowish color. With this form, rapid thinning of the enamel is observed.
- Erosive - in addition to stains on the enamel, erosive defects occur. They contribute to the destruction of not only enamel, but also dentin.
- Destructive is the most severe form, in which the shape of the tooth crown is disrupted. This occurs due to thinning of the enamel and destruction of hard tooth tissue. The teeth themselves are quite fragile, prone to various damages (chips, breaks).
The disease can occur in mild, moderate and severe degrees. This depends on the number of teeth affected, as well as the depth of the pathological process. In severe cases, the patient experiences damage to more than 80% of the teeth. In this case, dentin is affected and crown deformation is observed. Fluorosis can also cause pathological disorders of skeletal bones.
Symptoms of purulent pulpitis
The following symptoms are characteristic of purulent pulpitis:
- painful sensations in the tooth for no apparent reason, occurring spontaneously, often the pain is pulsating in nature;
- pain of a constant nature, weakening only for a short time;
- increased pain from any hot foods or drinks, as well as its weakening from any cold foods;
- reaction to sour and sweet foods, which lasts up to half an hour even after stopping contact with the irritant;
- increased pain at night;
- swelling of the oral mucosa near the painful tooth;
- in some cases, gum bleeding and dark enamel color;
- pain not only in one tooth, but throughout the entire oral cavity, in the head and ears.
As a rule, with this disease, the patient even finds it difficult to answer the question of which tooth exactly hurts. In addition, other symptoms are often added to the pain: general weakness, slight fever and malaise.