Anatomy, physiology
The periodontium
is a complex organ of the oral cavity surrounding the teeth, formed from specialized tissues. It is located on the jaws and its main functions are to support (support) the teeth and their nutrition and innervation.
Nutrition (trophism) is provided by blood and lymphatic vessels that supply oxygen and metabolic products to the periodontal tissue.
There are four main anatomical and functional elements of the periodontium:
- gum,
- periodontium,
- alveolar bone with periosteum,
- root cement
The gum is a soft tissue - a mucous membrane covering the alveolar processes, with an underlying connective tissue layer.
It contains lymphatic vessels (they are involved in regulating fluid pressure in tissues and protecting against microbial agents).
Through the periodontium - the ligament of the tooth, the latter is fixed in the jaw bone.
Periodontium
(otherwise known as desmodont) is a connective tissue formation surrounding the tooth and located between the root cement and the inner cortical plate of the alveolar bone.
This ligament, consisting of the main substance, fibers and cellular elements, like an elastic gasket, absorbs the load on the tooth, giving it minimal mobility. When periodontal disease and death occur, fusion of the bone with the tooth – ankylosis – can occur.
The next element of the periodontium is cement, which is also a hard tissue covering the root of the tooth. It is formed by collagen fibers directed along the root and an adhesive substance.
Bone
The alveolar process, in which the tooth is strengthened by periodontium, is composed of outer and inner dense plates and a spongy part between them.
Spongy bone consists of trabecular septa, the direction and shape of which is determined by the load on the jaws and teeth, and bone marrow.
Bone tissue contains mainly crystals of hydroxylapatite (inorganic) and small amounts of water and organic substances.
The cellular elements of bone - osteoblasts, osteoclasts and osteocytes, under the influence of the nervous and humoral system, determine changes in the shape, volume and quality of this tissue.
The bone tissue of the alveolar process is covered with a dense connective tissue structure - the periosteum; it, with the vessels located in it, plays a significant role in the blood supply to the bone.
The blood supply provides tissues and anatomical formations with organic and mineral substances.
At the level of the enamel-cement junction (neck of the tooth), an anatomical formation stands out in the marginal part of the gum - a vascular cuff, which, like an elastic band, ensures a tight fit of the gum to the tooth due to hydrostatic pressure.
The main source of blood supply to periodontal tissue is the external carotid artery with the maxillary and mandibular arteries branching from it.
Venules and veins collect blood into the internal jugular vein. The periodontium is innervated by the trigeminal nerve and the superior cervical sympathetic ganglion.
Among others, there is an anatomical formation - the dentogingival junction
. This is the connection between the gum epithelium and the neck of the tooth.
It is physicochemical: molecules of epithelial cells adhere to cement structures through gingival fluid cells.
Gingival fluid produced by periodontal tissue plays the role of a protective barrier against microorganisms through the activity of phagocytes and its chemical properties. It should be noted that the periodontium is washed by saliva. It is secreted by the major and minor salivary glands.
In addition to water (99.42%), saliva contains organic substances, salts and trace elements. Organic substances enter the oral fluid from blood serum and are secreted by the salivary glands and microorganisms present in the mouth.
Of the inorganic substances, calcium phosphate and calcium bicarbonate (they take part in the formation of tartar), phosphate and sodium chloride are important.
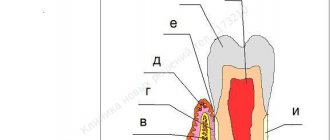
Diagram 1: periodontium
. a – submucosal layer with lymphatic vessels; b — mucous membrane of the attached gum; c - spongy bone of the alveolar process between the plates of the compact substance; d – periodontal fibers are woven into the root cement; e – gingival margin with vessels of the gingival cuff; e – dentogingival junction; g – tooth enamel; h – dental pulp; and – root cement; j – root dentin.
Age-related changes in periodontium
In the periodontium, with age, there is a decrease in the number of collagen fibers and a decrease in their quality. The epithelial layer of the mucosa becomes thinner, and keratinization is disrupted.
The bone tissue of the alveoli becomes less dense, the cortical layer atrophies.
Medical Internet conferences
The need for orthodontic treatment has increased significantly in recent years. But at the same time, the number of dental diseases that are directly related to the presence of structures in the oral cavity is growing [3]. This is explained by the fact that orthodontic appliances are not indifferent to the human body and, when exposed to the oral mucosa, change the activity of salivary enzymes, causing dental diseases. These complications of orthodontic treatment lead to changes in homeostasis: the destruction of normal microflora or a disproportionate change in the number of components of the oral microbiocenosis, which ultimately leads to the development of dysbiosis and the occurrence of both inflammatory processes in periodontal tissues and processes of demineralization of hard dental tissues [2, 7, 10, 12, 13].
The main etiological factor causing inflammation in periodontal tissues, as well as dental caries, is dental plaque. In patients undergoing orthodontic treatment, the cariogenic situation in the oral cavity increases due to the fact that around the elements of the orthodontic structure, in the spaces between the teeth and in the cervical areas, due to difficulty in hygiene, food residues accumulate in which microorganisms multiply, producing acids in the process of their vital activity, leading to a decrease in the pH of the oral fluid, increased enamel permeability and demineralization [5, 9, 11, 14–16].
Plaque contributes to the development of not only caries, but also periodontal disease. Pathological processes in the periodontium begin with gingivitis, which is manifested by redness and bleeding. Bleeding gums during orthodontic treatment occurs quite often when brushing teeth, as well as while eating solid foods. If left untreated, gingivitis progresses to periodontitis. With periodontitis, tooth mobility appears, pathological periodontal pockets form, and patients may be bothered by bad breath.
To avoid complications during orthodontic treatment, it is necessary to follow the rules of hygiene and a balanced diet. It is very important to teach the patient the rules of hygiene and monitor its implementation even before installing the device. It should be explained to the patient that toothpaste and toothbrush alone will not be enough to maintain the oral cavity in good condition. It is necessary to use a soft toothbrush and a special paste to clean the surface of the removable appliance from plaque, a gel or mouthwash for daily use that dissolves dirt and destroys bacteria that accumulate on the appliance. Once a week you need to soak the device in cleaning concentrate for more thorough care. An integral part is the use of the following additional hygiene products: brushes - for cleaning interdental spaces and removable orthodontic appliances; floss - will clean the interdental spaces and gum pockets; irrigator - for thorough cleaning of dental spaces, cleansing the surface of teeth from newly formed plaque and improving blood circulation in soft tissues; plaque indicator tablets – allow you to evaluate the quality of hygiene.
During meals, it is necessary to remove the orthodontic device and put it on after carrying out hygienic measures [1, 6].
It is well known that after tooth eruption, active mineralization of the enamel occurs within 2–3 years. Therefore, it is advisable to carry out local preventive measures during this period. One of the most effective modern methods of preventing dental caries, stimulating the process of “maturation” of enamel, is fissure sealing. For this purpose, special materials are used - sealants. Most sealants contain silanes - fluorine-containing substances that split off fluoride ions over a long period of time, which diffuse into the layers of hard tooth tissue adjacent to the sealants, stimulating their mineralization. The use of sealants leads to stabilization of the carious process for 1–9 years.
The next important point is diet correction. It is necessary to reduce the consumption of easily digestible carbohydrates (chocolate, sweets, flour products), and, on the contrary, increase the consumption of foods containing easily digestible Ca2+ (milk, low-fat cottage cheese) in order to increase the mineralizing function of saliva. At the same time, it is useful to consume foods that help shift the pH to the slightly alkaline side, for example, cheese [4, 8, 16].
Such an integrated approach to prevention will help improve the hygienic state of the oral cavity and reduce the incidence of dental caries and periodontal diseases in patients during orthodontic treatment.
Classification of periodontal diseases.
Gingivitis
Gingivitis is an inflammatory superficial disease of the gum tissue.
With gingivitis, there is no disruption of the periodontal junction and bone. Based on the form of manifestation of periodontal disease, the following are distinguished:
- catarrhal gingivitis,
- hypertrophic gingivitis,
- ulcerative gingivitis.
According to the type of course, gingivitis is divided into acute, chronic, aggravated and remission. According to the distribution, gingivitis can be localized and generalized. Without active treatment, gingivitis progresses to periodontitis.
Periodontitis.
Periodontitis is a deep inflammatory disease of the periodontium with destruction of the periodontal junction and bone tissue of the alveoli.
There are acute, chronic course of periodontitis, exacerbation of the disease and remission. Periodontitis can be mild, moderate or severe.
According to the prevalence, this gum disease is divided into generalized and localized periodontitis.
Photo 1. X-ray picture of severe periodontitis. The roots of the teeth are exposed by two-thirds.
2. 1.
Additionally, there is a condition known as
an aggressive form of periodontitis.
This diagnosis can be made by a doctor based on the presence of a set of signs of gum disease. In this case, periodontal destruction is generalized and rapid.
Such periodontitis is typical for ages from adolescence to 35 years. Often the aggressive form of periodontitis is accompanied by gum growth and granulation. During the period of remission, inflammatory manifestations may subside and even disappear.
Periodontal disease
Periodontal disease is a chronic degenerative periodontal disease.
In European and American classification as a separate gum disease
doesn't stand out. Periodontal disease is characterized by a long-term, benign course and almost does not lead to loosening and loss of teeth.
Periodontal diseases - as symptoms of other diseases
There are idiopathic periodontal diseases with progressive destruction of periodontal tissue (periodontal syndrome).
Such conditions can occur when exposed to physical factors (radiation), poisoning, immunodeficiency, diabetes mellitus, eosinophilic granuloma, Papillon-Lefevre syndrome, neutropenia, etc.
Periodontomas. Epulis (epulid) and gingival fibromatosis
Periodontomas are tumors and tumor-like conditions of the gums. The most common of them are epulis (epulid) and gingival fibromatosis.
Gingival fibromatosis is characterized by the proliferation of periodontal tissues, which causes tumor-like damage to the gum tissue. Gingival fibromatosis is most common in adults, but is sometimes diagnosed in children.
The diagnosis of gingival fibromatosis is made by a specialist based on the patient’s complaints, examination data, radiography, and histological examination.
The main reason for the growth of gum tissue, as a rule, is a violation of metabolic processes; drug-induced fibromatosis of the gums is also identified. Treatment of the disease is surgical and consists of excision of the overgrown gum to the periosteum.
Photo 2. Gingival fibromatosis
Etiology and pathogenesis (causes and development) of periodontal diseases
Calculus
The main point in the development of gum diseases such as gingivitis and periodontitis is dental plaque (plaque), which turns into tartar (calculus).
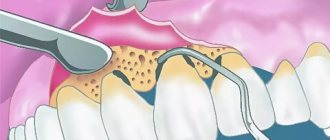
Photo 3. Soft plaque (plaque). Marginal periodontitis.
It is believed that organic soft dental plaque, which is formed from food debris due to poor hygiene, is gradually saturated with calcium from saliva and serum exudate of the gum pockets and is converted into hard tartar.
The latter can be of different hardness and color, which is determined by its composition. It consists of 18-25% organic matter (microbes and dead cells) and 75-82% inorganic matter (calcium, phosphorus, metal salts).
Tartar causes traumatic compression of the gums and prevents the cleaning of the periodontal pocket, promoting the development of microbial agents.
Microorganisms diffuse deep into periodontal tissues, lingering on the surface of the basement membrane and further into the bone tissue of the alveolar process.
Traumatic closure of teeth
In the absence of part of the teeth, in case of violation of the position of the teeth, in case of partial destruction of teeth and other traumatic factors, the remaining teeth are subjected to excessive and inadequate load. The latter, in turn, destroys the periodontium of the teeth.
Improper functioning of the temporomandibular joint (TMJ).
The ANS may be a significant factor in the development of gum disease.
Dentistry (rare atlases and books) / Periodontal diseases in children
7
the plate of the mucous membrane is smooth, because There are no connective tissue papillae here.
The attachment epithelium is multilayered and is a continuation of the sulcus epithelium. The surface cells of this epithelium provide attachment of the gum to the tooth surface using hemidesmosomes associated with the second (inner) basement membrane. As a result, they are not subject to desquamation. The cells lying under the surface layer of the epithelium undergo desquamation, which are displaced towards the gingival sulcus and sloughed into its lumen, i.e., epithelial cells from the basal layer are displaced simultaneously towards the enamel and gingival sulcus. The intensity of desquamation of the attachment epithelium is very high, but the loss of cells is balanced by their constant new formation in the basal layer, where epithelial cells are characterized by very high mitotic activity. The rate of renewal of the attachment epithelium under physiological conditions is 4-10 days in humans.
The cells of the attachment epithelium differ from the epithelial cells of the rest of the gum: they contain more developed granular endoplasmic reticulum and the Golgi complex, a set of cytokeratins, surface membrane carbohydrates, etc. All this is typical for poorly differentiated cells. This is important for preserving their ability to form hemidesmosomes, which ensure the connection of the epithelium with the surface of the tooth. The intercellular spaces in the attachment epithelium are expanded and occupy about 20% of its volume, and the content of desmosomes connecting epithelial cells is reduced four times compared to those in the sulcal epithelium. Due to this, the attachment epithelium has high permeability, allowing the transport of substances through it in both directions. From the oral fluid and from the surface of the mucous membrane, a massive flow of antigens into the tissues of the internal environment occurs; many substances are transferred in the opposite direction: from the blood to the epithelium and then into the lumen of the gingival sulcus.
The lamina propria in the area of the periodontal junction is formed by loose fibrous tissue with a large number of small vessels. Four to five parallel arterioles form a dense network-like plexus in the area of the gingival papilla. The capillaries of the gums are very close to the surface of the epithelium: in the area of epithelial attachment they are covered with only a few layers of spinous cells. The blood flow of the gums accounts for 70% of the blood supply to other periodontal tissues. Comparison of microcirculation levels at symmetrical points of the gums on the upper and lower jaws, as well as on the right and left, during a biomicroscopic study, showed a uniform distribution of capillary blood flow in the intact periodontium.
Granulocytes (mainly neutrophils) migrate through the vascular wall, less often monocytes and lymphocytes, which