Generalized periodontitis: symptoms and treatment
Periodontitis is a very common pathology of periodontal tissues (soft tissue structures around the dental unit). If the pathological process is started and left without treatment, then you can lose all the dental units.
Periodontal pockets are the best location for the emergence and development of an infectious process, which does not have the best effect on the healthy state of the body. A beautiful and healthy smile gives you self-confidence and makes you feel natural. When periodontal tissue is damaged, the gums become red and swollen. The disease affects the overall health of the body and the well-being of a person. If something bothers you in the oral cavity, you should immediately consult a specialist. Dentist therapists at the branches of the West Dental family clinic in Yanino-1 and Vsevolozhsk will help with identifying the origins of anxiety and their treatment.
It has been scientifically determined that the occurrence of periodontitis is influenced by: soft plaque and hard deposits; filling material or orthopedic structure fixed in violation of treatment protocols.
History of periodontology (literature review)
Periodontal diseases have been known to mankind since prehistoric times. At the same time, periodontitis was a fairly common disease, as evidenced by studies of the embalmed bodies of ancient Egyptians (Fermin A. Carranza., 2003). Therefore, it is not surprising that much attention was paid to the problem in medical works of that time, in which many remedies for strengthening teeth and gums were presented. These products were made from various plants and minerals and were applied to the gums in the form of a paste with honey and plant resin as a base (Ebbel B., 1937).
In the works of the ancient Hindus, many severe cases of periodontal disease with loss of teeth and purulent inflammation of the gums are given, the role of brushing teeth, oral hygiene is emphasized and the toothbrush is described (Kaviratna AC, 1892; Kaviratna AC, 1907).
In the oldest manuscript written in Ancient China, Huang Ti around 2500 BC. e., contains a detailed description of gum inflammation and periodontal abscess (Dabry P., 1863). Medicinal herbs were recommended to treat such conditions. The Chinese were among the first to use “chewing sticks” for cleaning teeth and massaging gums, which were made from the roots or branches of plants by flattening one end into a soft fiber (Jones WHS, Withington ET, 1923, 1931; Kimery MJ, 1968).
The father of modern medicine, Hippocrates (460-377 BC), studying the causes of periodontitis and tooth loss, attached great importance to dental plaque and tartar. With the development of Greek culture, one of the golden periods of Western civilization began. Architecture, painting, sculpture, poetry, drama, philosophy and history reached perfection. These were the times of Homer, Plato and Aristotle. Modern science also originated in Greece. Medicine evolved with a diagnostic approach and technical skills. The father of modern medicine, Hippocrates (460-377 BC), studying the causes of periodontitis and tooth loss, attached great importance to dental plaque and tartar. Inflammation of the gums was characterized by bleeding, separation of the gum from the tooth and bad breath and was associated with chronic diseases of the spleen (Castiglione A., 1941; Jones WHS, Withington ET, 1923, 1931).
Medicine further developed during the era of Roman civilization and the early Byzantine period. The Romans paid great attention to oral hygiene. The use of a toothbrush is mentioned in the works of Roman poets. The Roman Aulus Cornelius Celsus (25 BC - 50 AD) wrote about gum disease and suggested chewing unripe pears and apples and holding their juice in the mouth for treatment. He described the loss of teeth caused by weakness of their roots or sluggish gums, and noted that in such cases the gums should be burned with a hot iron and then lubricated with honey (Spencer WG, 1935, 1938).
The fall of the Roman Empire was accompanied by the rise of Arab science and medicine. Most of the Arabic treatises were created on the basis of Greek medical sources, much was revised, and new approaches were proposed, especially in surgical treatment. Significant achievements of Islamic medicine formed the basis for the development of medicine in Europe during the late Middle Ages and the Renaissance. Abu Bakr Muhammed ibn Zakariya al Razi (Rhazes) (841-926) compiled a 25-volume encyclopedia on medicine, Ali ibn Abbas al Majousi (Haly Abbas) (930-994) described many dental diseases.
Ibn Sina's (Avicenna) (980–1037) treatise on medicine is probably the most famous work in this field of all time, being in continuous use for almost 600 years. The titles of the treatise's chapters on gum disease are eloquent: these are “Bleeding Gum”, “Cracked Gum”, “Gum Ulcers”, “Gum Separation”, “Gum Recession”, “Weakening Gum” and “Epulis”. Avicenna used many remedies in the treatment of periodontal diseases and rarely resorted to surgery (Hildesheim, Georg Olms., 1964).
Paracelsus developed an interesting and unusual theory of diseases: the doctrine of hard dental plaque, believing that pathological calcification occurs in various organs, and diseases are the cause of a metabolic disorder in which undigested material is released in the form of a “stone.” An undoubted contribution to periodontics was made by the most outstanding physician and the surgeon of the Western Caliphate in Cordoba, Abu'l-Qasim (936–1013). He had a clear understanding of the etiological role of tartar and described in detail methods for removing dental deposits, using a set of sophisticated instruments developed by himself. Abu'l-Qasim wrote: “Sometimes deposits of large and coarse unsightly calculi form on the inner and outer surfaces of the teeth or between the gums: the teeth become black, yellow or green, after which the gums change and the teeth become unsightly. To treat this condition, have the patient sit in front of you with his head on your lap. Clean teeth that have stones or rough deposits on them until they are completely removed. Scrub also in all those places where the teeth are black, yellow, green or other color, until they (calcified deposits) are completely removed. It is possible that one procedure will be sufficient. Otherwise, repeat a second, third, or fourth time until your goal is completely achieved. You should know that tartar removal is carried out with instruments that have different shapes according to the purpose required of them. The instruments used to remove tartar from the inner surfaces of teeth are different from the instruments used to treat external surfaces, as well as those used for interdental surfaces.” In addition, he described in detail the method of tooth extraction, methods of strengthening mobile teeth with gold wire (Fermin A. Carranza., 2003).
During the Renaissance, significant discoveries were made in the fields of anatomy and surgery. Paracelsus (1493-1541) continues to be an important figure of this era, the collection of his works in the modern edition of K. Sudhoff is still analyzed in order to understand his ideas and very complex concepts in various fields of science from chemistry to philosophy (Oldfenbourg R., 1922— 1933). He developed an interesting and unusual theory of disease: the doctrine of hard dental plaque, believing that pathological calcification occurs in various organs, and diseases are caused by a metabolic disorder in which undigested material is excreted in the form of “stone.” This fossilized or final material, consisting of bud sand and glue-like components, is exogenous and comes from barley and peas, milk, meat and fish, and beverages such as wine, beer and fruit juice. It can be removed by digestion and thus excreted in excrement. It was believed that the content of food in terms of elements capable of deposition varied in different geographical places, that saliva served for digestion in the mouth, like other substances in the stomach, that the formation of stone could be accelerated by the influence of salt, which thickens the mucus-like substance in food, that the amount of formed hard deposits depend on the area of the body. Paracelsus identified extensive tartar formation on teeth and associated it with toothache. Thus, dental pain was considered comparable to pain caused by calcification in other organs, such as the kidneys.
Most of the Arabic treatises were created on the basis of Greek sources, much was revised, new approaches were proposed, especially in surgery. The outstanding Roman anatomist Bartholomaeus Eustachius (1520-74) published a book containing many new concepts based on clinical research. Eustachius described periodontal tissues and periodontal ligaments. In addition, his method of treating periodontitis was surprisingly modern, he proposed removing tartar and curettage of granulation tissue using stimulating drugs so that a new attachment could form (Chernin DA, Shklar G., 1999).
The French surgeon Ambroise Pare (1509–90) made a significant contribution to periodontal surgery. He developed in detail many surgical procedures, including gingivectomy for gingival hypertrophy (Malgaigne JF, 1840). He recognized the etiological significance of tartar and used a set of instruments to remove hard deposits from teeth.
The first book in German by an unknown author was published in 1530 in Leipzig and was called “Artzney Buchlein or Zene Artzney”. The book was essentially a summary of previous works on diseases of the organs and tissues of the mouth and their treatment. Three chapters were devoted to periodontology. The publication presented the initial concept of the role of systemic and local factors in the etiology of periodontitis. Local infectious agents were also mentioned. Many ointments were offered, mostly of an astringent nature, and it was recommended to splint mobile teeth to healthy ones using silk or gold thread. The cauterization of gums with a hot iron was also mentioned, but only if the doctor had special skills. For “gum rotting,” necrotization of the gums was discussed using medications containing vinegar or alum. The author also suggested scraping black teeth and brushing them with toothpaste or powder, recipes for which were given in the book (Michael Blum, 1887).
Periodontal diseases were first classified by the Italian physician Girolamo Cardano (1501–1576). In a publication dated 1562, he mentions a type of disease that occurs with age and leads to progressive weakening and loss of teeth, as well as a very aggressive type of disease occurring in young patients (Held AJ., 1989). Such a classification was rediscovered and widely accepted only in the twentieth century.
Anton van Leeuwenhoek (1623-1783), using the microscope he invented, was the first to discover the bacterial flora of the mouth, and his drawings quite accurately depicted oral spirochetes and bacilli (Leeuwenhoek A., 1695).
For the first time, periodontal diseases were classified by the Italian doctor Girolamo Cardano. In a publication dated 1562, he mentions a type of disease that occurs in patients as they age and leads to progressive weakening and loss of teeth. Dentistry as a science and specialty began its rapid development in Europe in the 18th century, mainly in France and England. Along with general dentistry, there was an active development of periodontology. Pierre Fauchard, although he did not have the appropriate education, was able to develop a systematic approach to dental practice based on modern knowledge. He greatly improved the instruments and technical skills used in dental treatment, and his book The Surgeon Dentist, published in 1728, contributed to the improvement of the technical and surgical skills of dentists (Fauchard P., 1728). The book paid special attention to the prevention of dental diseases. He described in detail his tools for treating periodontal disease and his technique for removing tartar.
John Hunter (1728–1793), the most eminent anatomist, surgeon, and pathologist in 18th-century England, wrote a superb work on dentistry, providing remarkably clear illustrations of the anatomy of teeth and their supporting structures. He also described the clinic of periodontitis and outlined the concept of active and passive tooth loss (Hunter J., 1771).
Hunter's contemporary Thomas Beardmore (1740–85), known as "his majesty's dentist" (i.e., King George III), published a Treatise on the Disorders and Deformations of the Teeth and Gums in 1770, several chapters of which were devoted to periodontal diseases. In Chapter 7, “On Tartar, Gum Recession, and Toothache Caused by Unremoved Tartar,” Beardmore offered a detailed description of the instruments for removing tartar, thereby emphasizing its importance in the prevention of periodontal disease, and used the surgical treatment method to remove hypertrophied gums after removal of dental plaque (Hunter J., 1835; Major RHL., 1954).
One of the representatives of dentists in the 19th century was the German Leonard Koecker (1785-1850). In 1821, the Philadelphia Journal of Medicine and Physical Sciences published his description of inflammatory changes in the gums and the presence of tartar on the teeth, leading to their loosening and loss. He wrote about the need for careful removal of tartar and oral hygiene, which, according to his recommendations, should be carried out in the morning and after each meal using an astringent powder and a toothbrush. He denied splinting as weakening healthy teeth, and recommended postponing treatment of caries and prosthetics until gum treatment was completed. Koecker was one of the first adherents of the theory of odontogenic infection and recommended removing all affected teeth in order to prevent systemic infection (Koecker A., 1821).
Levi Spear Parmly (1790–1859), a New Orleans dentist, is considered the founder of oral hygiene and the inventor of dental floss (Fischman SL, 1997).
The term pyorrhea alveolaris was first used by Alphonse Toirac (1791–1863) in 1823, although some scholars dispute this fact, believing that it was introduced to the United States by the German émigré physician F. H. Rehwinkel.
One of the representatives of dentists in the 19th century was the German Leonard Koecke. In his works, he wrote about the need for careful removal of tartar and oral hygiene, which should be carried out in the morning and after each meal using an astringent powder and a toothbrush. In the 19th century, the most authoritative in the field of treatment of periodontal diseases was John W. Riggs (1811-85 ). This is supported by the fact that periodontitis or alveolar pyorrhea is known as “Riggs disease”. He was the first doctor to limit his practice to the treatment of periodontal diseases. Therefore, we can consider him the first specialist in this field. Riggs and his students were proponents of the so-called conservative approach to the treatment of periodontal disease, developing the concept of preventing oral diseases. He advocated a clean mouth, believing that “the teeth themselves, with their accumulated deposits and rough surfaces, are the cause of disease,” and therefore strongly opposed periodontal surgery, which at that time consisted of gingival resection (Riggs JW, 1876; MacManus C., 1902; Rawls AO, 1885).
Among his followers was W. J. Younger (1838–1920), who considered periodontitis to be a local infection and was the first to discuss the possibility of gum tissue grafting. In 1902, he published a case of a free gingival graft from the retromolar region to cover gingival recession in the canine of the same patient (Black GV, 1915).
In the second half of the 19th century, several important events occurred in medical science (the invention of anesthesia, asepsis and antisepsis, radiography), which marked the beginning of a new period in dentistry (Carranza FA, 1998). In addition, the studies of Rudolph Virchow (1821–1902), Julius Cohnhein (1839–84), Ilya Mechnikov (1845–1916) and others gradually began to shed light on the morphological changes that occur during inflammation. Based on this, the Moscow doctor N. N. Znamensky established the complex interaction of local and systemic factors in the etiology of periodontal diseases, which led to an understanding of their pathogenesis based on histological studies. In 1902, he published an article in which he described a cellular infiltrate in the inflamed gum, penetrating deeper as the disease progressed, causing bone resorption involving multinucleated cells.
Moscow doctor N. N. Znamensky established the complex interaction of local and systemic factors in the etiology of periodontal diseases, which led to an understanding of their pathogenesis based on histological studies. It is believed that Adolph Witzel (1847-1906) was the first to prove the bacterial nature of periodontitis (American Dental Club of Paris : Meetings of December 1902 and January and March 1903. Dent Cosmos 1904; Witzel A., 1882), but in fact the first researcher of oral microphora was Willoughby D. Miller (1853-1907), who devoted his career to introducing modern principles of bacteriology into dentistry In his book, published in 1890, he describes the symptoms of periodontitis and considers the role of predisposing factors, irritants and bacteria in the etiology of pyorrhea alveolaris. He believed that the disease was not caused by specific bacteria, but by a complex of bacteria that are normally present in the mouth. This constituted what later became known as the “nonspecific plaque theory,” which persisted without much change for seven decades (Ackernecht EH, 1981; Miller WD, 1891).
At the same time, surgical methods for the treatment of periodontal diseases were developed. Salomon Robicsek (1845–1928) was born in Hungary, received his doctorate and practiced dentistry in Vienna. He developed a surgical technique consisting of scalloped continuous excision of the gum (gingivectomy) followed by curettage and bone remodeling (Stern IB, 1965).
The first description (1901) of the possible role of trauma in occlusion disorders and bruxism in periodontal diseases belongs to the Austrian dentist Moritz Karolyi (1865-1945), who recommended correcting occlusion by grinding the chewing surfaces and using bite plates (Karolyi M., 1901).
In 1904, the French doctors Hyacinthe Jean Vincent (1862-1950) and Hugo Carl Plaut (1858-1928), with acute necrotizing ulcerative gingivitis, isolated spirilla and bacilli that caused what was later called Vincent's angina (Vincent JH, 1896 , 1904; Plaut HC, 1894; Gold SI, 1985).
In the first third of the twentieth century, periodontics flourished in Europe, with two major centers of excellence: Vienna and Berlin.
The Viennese school developed the histopathological direction, which formed the basis of modern periodontology. The main representative of this trend was Bernhard Gottlieb (1885-1950), who conducted extensive microscopic studies of periodontal tissue using autopsy material. He described the adherence of the gingival epithelium to the tooth, the histopathology of inflammatory and degenerative changes in the periodontium (Carranza FA, 1998), active and passive teething and traumatic occlusion (Editorial. JAMA 1952; Gottlieb B., 1923, 1925).
Extensive histological studies carried out by Gottlieb's contemporary in Vienna, Bälint J. Orben (1899–1960), served as the basis for the development of therapeutic measures for periodontitis. Other members of the Vienna School, Rudolf Kronfeld (1901–40), Joseph P. Weinman (1889–1960), and Harry Sicher (1889–1974), emigrated to the United States in the 1930s and contributed to the development of American dentistry.
Non-surgical approaches to the treatment of periodontal diseases were developed by Isadore Hirschfeld (1882-1965), who wrote classic manuals on oral hygiene about the importance of local factors, etc. (Hirschfeld 1., 1936) The Berlin group consisted mainly of clinicians who developed and improved surgical methods treatment of periodontitis. The most prominent among them were Oscar Wesky (1879–1952) and Robert Neumann (1882–1958). O. Veski wrote a manual that compared histopathological changes with the clinical manifestations of periodontal diseases (Weski O., 1921). R. Neumann, together with L. Widman (1871-1956) and A. Cishinsky, described the principles of periodontal surgery, including bone remodeling. These methods are currently used by specialists (Gold SI, 1982; Widman L., 1971; Neumann R., 1923).
At this time, surgical methods of treatment for exposure of tooth roots were developed in the USA (Younger WJ, 1902; Harlan AW, 1906; Rosenthal P., 1912 American Dental Club of Paris: Meetings of December 1902 and January and March 1903. Dent Cosmos 1904). However, they were not widely used at that time. Before the First World War, the improvement of periodontal surgery was carried out by many other researchers (Zentler A., 1918; Black GV, 1915; Kirkland O., 1936; Ward AW, 1928).
Non-surgical approaches to the treatment of periodontal diseases were developed by Isadore Hirschfeld (1882-1965), who wrote classic manuals on oral hygiene about the importance of local factors, etc. (Hirschfeld 1., 1936). In 1913, the first school for dental hygienists in Connecticut was established by Alfred Fownes (1869–1938).
The most comprehensive monograph on periodontology published in the first half of the twentieth century was El Paradencio, Su Patologia y Tratamiento by the Uruguayan author FM Pucci, which appeared in 1939.
Since 1818, the role of focal infection in the mouth in the development of septic and rheumatic processes and other diseases has been recognized (Miller WD, 1891). In order to prevent systemic diseases, removal of affected teeth was proposed (Ackernecht EH, 1981; Hunter W., 1900, 1911). However, the enthusiasm for this method led to its discredit, since positive results were not always noted (Editorial. JAMA 1952; O'Reilly PG, 2000).
The idea was returned to in the 1990s, this time with clearer indications. Since the 1950s in the United States and Scandinavia, clinical knowledge in periodontology has been expanded through experimental microbiological and immunological research (Irving Glickman, Herman Becks, Paul Boyle, Henry Goldman, Balint Orban, Sigurd Ramfjord, Isaac Schour, Joseph Weinmann).
Currently, the study of the role of microorganisms and the immunological response is the focus of many research groups: Robert Genco, Roy Page, Sigmund Socransky, Max Listgarten, Walter Loesche, Jorgen Slots. Knowledge about the biological and clinical aspects of periodontology is presented at international conferences, among which significant were the conferences held in 1951, 1966, 1977, 1989 and 1996 by the American Academy of Periodontology (AAP), which was founded in 1914 and has become a leader among other organizations and has monthly scientific publications in the form of the “Journal of Periodontology”.
Scientific evidence in the field of periodontics is covered in the journals Journal of Periodontal Research, Journal of Clinical Periodontology, Periodontology 2000, International Journal of Periodontics and Restorative Dentistry. Among publications in other languages, the Journal de Parodontologie (France), Periodoncia (Spain) and the Japanese Association of Periodontology (Japan) deserve mention.
Periodontics was recognized as a specialty of dentistry by the American Dental Association in 1947. Training in periodontics began at several universities (Columbia, Michigan, Tufts) in the late 1940s. At first these were one-year and then two-year training programs. Currently, more than 50 periodontal programs exist at universities and all have a three-year duration. However, in Russia, periodontology has not yet been identified as a specialty, although new horizons are opening up for it.
Classification
According to the number of units affected by pathology:
- Catarrhal (localized) – 1-3 units in the affected area;
- Generalized – the entire dentition is affected.
According to the severity of generalized periodontitis (ICD code K05):
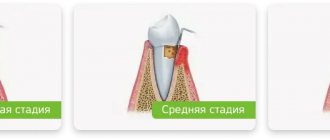
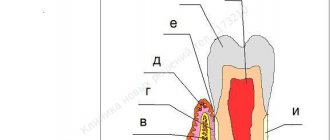
- Generalized mild periodontitis (ICD 10 code K05.3). This clinical diagnosis is made when the depth of the pockets in the gingival tissue is less than 3.5 mm, and less than 1/3 of the root is resorbed.
- Average. The subgingival depressions are 3.5-5 mm, and the bone is sclerosed at 50% of the root length.
- Severe degree. This stage is indicated by the depth of periodontal changes greater than 5 mm and resorption of more than 1/2 of the root.
Differential diagnosis according to pathogenesis:
- acute - more than one annual exacerbation;
- chronic generalized periodontitis (according to ICD K05) is an ongoing pathological process;
- exacerbation of chronic periodontitis – pain, discomfort, activation of the inflammatory process.
Indications
Vitamins A and C are especially important for patients with periodontitis. It is necessary to include more fruits, vegetables and herbs in the diet. At an early stage, when the teeth are not yet loosened, you can eat the fruits in solid form. This will ensure the necessary load on the dental system. It is necessary to chew on both sides, and not just one, so that all areas of the teeth work actively. It is useful to include the following products in the menu:
- seafood;
- apples;
- Bell pepper;
- avocado;
- dill, parsley;
- black currant berries;
- carrot;
- peanut;
- citrus.
The diet must include dairy products, which are a source of calcium. The patient needs to consume more milk, sour cream, cottage cheese, and different types of cheese. Vitamin A, which promotes epithelial regeneration, is found in pork and beef liver, pumpkin, apricots, broccoli and spinach. Zinc, which is present in lentils, peas, and seafood, is useful for bone tissue. If you have periodontal disease, it is better to drink green tea or natural juices.
Symptoms
The initial symptoms of the inflammatory process in periodontal tissues are the following:
- swelling of the gum tissue;
- severe bleeding during and after cleaning;
- throbbing severe pain.
As the pathology spreads, symptoms intensify:
- enlarged and painful lymph nodes;
- unpleasant odor from the mouth;
- mobility of dental units;
- increased sensitivity of tooth enamel;
- pain when biting and chewing food;
- deterioration of the general condition of the body;
- purulent discharge from periodontal pockets.
Chronic generalized periodontitis (beyond exacerbation) is characterized by:
- reddish color of gum tissue;
- exposure of tooth roots;
- Bone resorption is visually determined on the Rg image.
Chronic generalized periodontitis
Chronic generalized periodontitis (according to ICD 10-K05) affects the soft tissue and bone structures of all or more dental units. The frequency of occurrence is 5 times higher than carious lesions and its possible complications. Also, a generalized process can most likely lead to complete edentia (lack of teeth). The long-term location of the infectious process in periodontal tissues, without proper treatment, negatively affects the body's immune defense and can contribute to the development of rheumatoid arthritis, heart disease, etc. Generalized periodontitis has a different etiology.
Diagnostics
To determine the disease and its severity, various diagnostic methods are used. For generalized periodontitis, differential diagnosis includes an extensive consultation examination to draw up a medical history (formation plan):
- collection of complaints (mobility of units, discomfort when chewing, periodic sharp pain in the attached gum);
- visual and instrumental examination (gingival pockets, recession of gingival tissue, dental plaque, reddish gums);
- determination of the color, shape and structure of gum tissue;
- finding out what condition the dental units are in: percussion, palpation, degree of mobility;
- determination of hygiene indices;
- RG images.
Sometimes, a specialist may prescribe a blood test to clarify the etiology.
Diagnostic measures should take into account not only all the symptoms of the pathology and the patient’s complaints, but also the mandatory performance of an X-ray. Basically, in case of periodontitis, it is recommended to perform an OPTG (orthopantomogram) - a panoramic image. In such an extensive image, all dental structures and the degree of bone damage in each unit are immediately visible.
Mild degree
As usual, mild degrees are not given any importance. A subgingival pocket is formed near the dental unit, where microorganisms accumulate. There are signs of periodontal inflammation, and on the Rg image there is destruction of bone tissue by 1/3 of the root, gum pockets up to 3.5 mm. In the cervical area of the teeth, hard deposits are observed, the gums are loose, slightly inflamed and swollen. There is slight bleeding when cleaning, and discomfort when chewing solid food. Mobility and movement of teeth is not observed at this stage.
Degree of tooth mobility
With periodontitis, teeth gradually become loose. Depending on their mobility, there are 4 degrees of the disease:
- 1st degree, when the tooth moves no more than 1 mm to the adjacent tooth, in the bucco-lingual and vestibulo-oral directions;
- 2 degree, in which mobility is observed in the same directions as in the first degree, but only by more than 1 mm;
- 3rd degree. Teeth become mobile in any direction, including vertical;
- 4th degree. Mobility is observed in all directions, and the tooth can even rotate around its axis.
Average degree
With moderate severity, periodontal pockets up to 5 mm are observed. The x-ray shows damage to the bone septa on half the root. In the oral cavity, upon examination, there is a sufficient number of dental deposits, mobility of teeth I-II degrees, inflammation of the gums. A small amount of pus may ooze from under the gums. When the process worsens, slight mobility and displacement of units occurs.
Patients complain of pain in the gums; pain and bleeding when eating; the necks of the teeth are exposed; a reaction to cold and hot food is formed.
Severe degree
Chronic generalized severe periodontitis, as diagnosed, is determined by deep periodontal pockets over 5 mm and 2/3 of the tooth root being exposed. With this degree of pathology, great swelling, bleeding and hyperemia of the gums occurs, and eating is quite painful. In periodontal pockets there is a large accumulation of pus and microorganisms in the form of dental deposits. Patients have complaints of pain, itching, burning and pulsation in the gums. It is impossible to carry out high-quality hygienic cleaning on your own; a persistent unpleasant odor persists for a long time. In the absence of proper therapy, severe suppuration and mobility of grade III-IV units are observed, up to prolapse. Complications may develop in the form of abscess formation of foci of infection and periodontal disease.
Also, this pathology is manifested by a violation of the general condition of the body. A person is worried about weakness, fever, and in connection with this, fatigue. Regional submandibular lymph nodes enlarge and become painful on palpation.
Surgical intervention
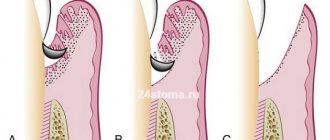
When the depth of the periodontal pocket exceeds 5 mm, doctors decide on surgical treatment. In this case, a flap operation is performed - gingivectomy. It is carried out according to the following scheme:
- The gum is dissected, after which the gum flap in the area of the periodontal pocket is turned away.
- Next, the tooth root is cleaned and destroyed tissues and microorganisms are removed from the pocket.
- Then the tissues are washed with an antiseptic, after which the gum flap is returned to its place and sutures are applied.
The duration of the operation can be from 1 to 3 hours, it is performed under local anesthesia. During the process, the doctor can also straighten the bone tissue if inflammation has already spread to it. Depending on the nature of tissue damage, other operations may be performed:
- Gingivoplasty is a soft tissue transplantation. It is carried out when they are completely atrophied, when the tooth is completely exposed and visually becomes longer. To cover the defects, tissues from the palate are used. This helps stop the deepening of the periodontal pocket.
- Osteoplasty. It is carried out in case of destruction of bone tissue by inflammation, which can no longer hold the tooth in its place. During the operation, a graft made of bone tissue or synthetic material is used.
Another surgical method for treating periodontitis is splinting mobile teeth. This procedure allows you to keep them in place and save them from spontaneous removal. Splinting today is carried out in different ways:
- A horizontal bar and fiberglass tape are placed over several teeth. Then everything is filled with a light composite, as a result of which the dentition is connected.
- On the teeth, the upper part of which is previously ground down, crowns are put on, welded together.
- A clasp prosthesis is placed on the jaw, which allows you to evenly distribute the load on both the teeth and gums, and when installed on the upper row, on the upper palate.
Treatment
When the pathological process has taken the form of chronic generalized periodontitis, it is more difficult to carry out effective treatment. It is important to address the underlying cause of the disease. In this regard, the generalized form of periodontitis requires consultation with dentists in related fields to identify the source of the pathology. The general dentist/periodontist can provide recommendations for consultation with an endocrinologist, hematologist, immunologist, etc. After general interaction and identification of the cause of periodontitis, the attending physician prescribes the necessary therapy.
Treatment of the pathological process consists of the following measures:
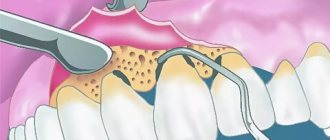
- Professional oral cleaning and hygiene training. A specialist removes soft and hard dental deposits, including those under the gums. The tooth enamel is polished with special brushes with paste and coated with a protective gel with fluoride. Oral care products are selected and instructions on their use are provided.
- Treatment of associated dental problems. To cure periodontitis, it is important to treat caries, pulp disease, and pathological processes in the gums and bones.
- Drug therapy. Oral baths with solutions, application ointments, NSAIDs and painkillers, and sometimes antimicrobial drugs are used.
- Removal of subgingival pockets by a dental surgeon. In case of moderate and severe severity, it is possible to perform open and closed curettage of pockets, as well as gum plastic surgery.
- Treatment using orthopedic structures. As part of complex measures, temporary splinting of mobile units is performed with an orthodontic retainer or fiberglass; selective grinding of the chewing surfaces of teeth; prosthetics of large dental defects to redistribute chewing pressure.
- Physiotherapeutic manipulations. Many physiotherapy procedures have a positive effect on recovery: UHF, infrared radiation, magnet and laser therapy, electrophoresis, direct and alternating current, vacuum and acupressure massage, paraffin therapy, mud therapy.
For effective treatment of pathology and the occurrence of remission of the process, it is important to fully comply with the specialist’s instructions.
Advantages of treatment at JSC "Medicine"
By contacting JSC “Medicine” (clinic of Academician Roitberg), you can be sure that the examination will be carried out as completely as possible and exclusively using high-precision equipment. From the first contact to receiving test results, no more than a day passes. Also, each patient of the clinic is provided with:
- an accompanying person to move around the clinic;
- personal physician-supervisor who will monitor the progress of diagnostics and treatment processes;
- written recommendations regarding treatment and all necessary information regarding prescribed medications.
At the clinic of JSC "Medicine" you will not waste your personal time in line. Our medical center provides services at an international level of quality, and if controversial issues arise, the administration is always ready to consider any requests.