What is stomatitis
Stomatitis (mucositis) is a disease that is accompanied by damage to soft tissues in the oral cavity.
It can be either an independent disease or a complication of various pathological processes, for example, measles, influenza, scarlet fever, etc. Until recently, stomatitis was considered a childhood disease. Today it is becoming more common in adults too. This trend raises questions about whether stomatitis is transmitted and, if so, how to protect yourself and your child. It all depends on the form of manifestation of the disease
What can you eat if you have stomatitis?
Inflamed mucous membranes and ulcers in the mouth make it impossible to eat as usual. Therefore, during illness you have to change your eating habits. This is necessary to reduce discomfort, reduce inflammation and restore normal microflora. Warm food with a soft consistency that does not irritate the mucous membrane is recommended. If you have stomatitis, you can eat:
- warm fermented milk products (ryazhenka, kefir)
- compotes and jelly from fresh berries or dried fruits
- liquid porridge
- meat and fish, steamed and pureed
- soups with lean broth
- cottage cheese dishes
If a child suffers from stomatitis, the diet depends on the age of the child and the form of the disease. Give your baby warm drinks more often, which soften the mucous membrane and reduce the process of intoxication, especially after feeding. This can be a chamomile decoction or even simple boiled water. And if stomatitis occurs in an infant, then pay increased attention to sterilizing bottles and nipples and treating the breast before and after feeding. Regardless of the patient’s age, the stop list for patients with stomatitis includes:
- bread
- juices, berries and fruits
- smoked products
- spicy and highly salty foods
- chips and crackers
- fried fish and meat dishes
If you have stomatitis, you will have to temporarily change your usual diet in favor of liquid or semi-liquid foods. At the same time, you should not even eat soft bread or cookies, as they can injure the inflamed mucous membrane.
Symptoms of stomatitis
Stomatitis can be recognized by the following signs:
- ulcers, wounds, erosions and rashes on tissues;
- red color of the mucous membrane;
- plaque on the tongue, inner surface of the cheeks, palate;
- unpleasant taste;
- swelling of tissues;
- heavy salivation;
- bad breath;
- itching and burning – in some cases;
- discomfort and pain;
- bleeding gums – occasionally;
- increased body temperature;
- lymphadenitis.
Symptoms in children are always more pronounced. The child often feels severe pain. Adults tolerate the disease easily. Its symptoms usually do not cause severe discomfort.
When the first symptoms appear, you should immediately consult a doctor to protect yourself and, possibly, others.
Treatment of viral stomatitis in children
The course of treatment for viral stomatitis in children depends on the timeliness of visiting a doctor, as well as the age and state of the child’s immunity. It may include:
- Rinse
As a rule, the dentist recommends treating the mucous membranes of the oral cavity with anti-inflammatory drugs. Also, for viral stomatitis in children, you can use decoctions of certain plants (calendula, chamomile, sage) or an infusion of oak bark. For small children who do not know how to rinse their mouths, irrigation can be done using a regular rubber bulb.
- Treatment with ointments and oils
After rinsing, for the treatment of viral stomatitis in children, sea buckthorn oil or vitamin A (in oily form) is usually used, which is used to lubricate the aphthae. If viral stomatitis in children is caused by herpes, the doctor will prescribe a special ointment. To treat the oral cavity with oils and ointments, you must use cotton swabs.
- Antipyretic and painkillers
Since the disease occurs with an increase in temperature and causes very painful sensations in the baby, the doctor prescribes appropriate medications. For example, for viral stomatitis in children, drugs such as Nurofen and paracetamol can be used.
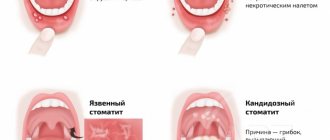
Types of disease
Stomatitis has different forms, depending on which the doctor determines whether it is contagious or not, and also prescribes appropriate treatment.
Allergic stomatitis
This is a common form of the disease that is difficult to treat. From the name it is clear that the cause of its development is an allergy, but it is necessary to find out what exactly it is. These could be medications, food, materials used for prosthetics. The disease is accompanied by the appearance of ulcers, which provoke pain.
Viral stomatitis
The most common type of viral stomatitis is herpetic stomatitis, the causative agent of which is the herpes virus. There are other forms that are provoked by adenovirus, enterovirus, etc. They are often found in children under 5–6 years of age, but are also common among older age groups. A feature of viral stomatitis is its erosive spread, when one ulcer appears next to another. Herpes mucositis may cause complications such as fever, nausea, vomiting and diarrhea.
This form of the disease is transmitted to others by contact and airborne droplets. If it is diagnosed, for example, in someone in kindergarten, then quarantine must be introduced. Infection occurs through dishes and toys, so the disease can quickly spread from child to child.
The virus spreads from nursing mothers to children if hygiene rules are violated. Adults become infected even through handshakes. Sneezing also causes the disease to develop.
Aphthous stomatitis
This form is common among adults. It develops against the background of a weakening of the body’s immune forces, so aphthous stomatitis is a common occurrence in spring and autumn. With this type of disease, characteristic aphthae appear - small ulcers. They can be single or group. Aphthous mucositis is not spread from person to person.
Fungal stomatitis
The disease manifests itself in children and adults, mainly in infants and women. It is provoked by fungi of the genus Candida, which are activated in the oral cavity when the immune system is weakened. The cause of fungal stomatitis can be long-term use of antibiotics. In addition to ulcers, its characteristic feature is a cheesy coating on the tongue, palate and inner surface of the cheeks.
Bacterial stomatitis
This type of disease is diagnosed when the oral cavity is affected by microorganisms, most often streptococci, staphylococci. The manifestation of bacterial stomatitis is provoked by tuberculosis, as well as sexually transmitted diseases, for example, gonorrhea, syphilis. More often, children whose immunity is not strong enough suffer from it. But everyone must be careful. The disease is transmitted from children to adults through dishes, toys, and damage to the mucous membrane.
This form is characterized by swelling in the oral cavity, redness of the mucous membrane and hardening of the palate, as well as an unpleasant odor, ulceration and cracks. Symptoms of intoxication may appear: vomiting, weakness, rapid pulse.
Other forms of stomatitis
In addition to the above types of disease, the following can also be distinguished:
- chemical stomatitis - occurs as a result of burns to the oral cavity with alkaline substances or acid;
- traumatic - ulcers are formed as a result of impact and disruption of tissue integrity;
- radiation – develops as a result of radiation.
Such forms are non-contagious and therefore do not pose a danger to other people.
Causes of aphthous stomatitis
Aphthous stomatitis can be an independent disease or develop as a result of complex causes. Among them:
- Using aggressive agents that dry out the oral cavity (for example, sodium lauryl sulfate) during daily oral hygiene. The mucous membrane becomes more vulnerable, especially to sour and pungent tastes, and ulcers easily form on it.
- Mechanical damage to the oral cavity. Accidental biting of the inner surface, scratches from fillings and dentures, sharp chips of a tooth, rough traumatic food violate the integrity of the mucous membrane, and the resulting ulcer can serve as the beginning of the disease.
- Nervous tension and stress.
- Unbalanced nutrition, diets, nutrient and mineral deficiencies. Particularly critical is the lack of iron, zinc, folic acid, selenium, and vitamins B and C.
- Allergy to food. Products with gluten (flour), apples, tomatoes, chocolate, seafood and some food additives are critical.
- Menstrual cycle in women. Codependency with aphthous stomatitis is observed in only 10–15% of cases.
- Genetic predisposition.
- Chronic blood diseases, gastrointestinal tract, immunodeficiencies.
- Long courses of taking nonsteroidal drugs, medications for arrhythmia and high blood pressure.
Ways of transmission of stomatitis
Let's summarize. Viral, bacterial and herpetic forms of stomatitis are contagious. Knowing how the disease is transmitted, you can protect yourself and your loved ones. Ways of transmission of infection:
- airborne - sneezing, coughing;
- household items - common dishes, linen, personal items;
- toys, raw pacifiers, rattles;
- dirty hands;
- unwashed food;
- biological fluids - through saliva, blood, breast milk;
- Pets can carry the virus.
It is possible to catch the infection anywhere – from the street to your own home. You can get infected from both a child and an adult.
Is stomatitis contagious?
There are many causes of stomatitis, but not all types of the disease are contagious. Infection of another person can occur in the presence of the following forms:
- Viral stomatitis, regardless of the causative agent of the disease.
- Stomatitis caused by a fungal infection.
- The bacterial form is transmitted mainly to children and adults with weakened immune systems.
Important! Stomatitis is not contagious to others if it occurs due to mechanical damage to the mucous membrane, burns, chemical or radiation therapy, friction of the prosthesis and exposure to other external factors.
Infection with a viral form
Viral form of stomatitis
The main causative agents of this form of stomatitis are influenza, chickenpox and herpes viruses; Adenoviruses and enteroviruses can also provoke the disease. This species is considered the most contagious, since it can be transmitted to adults and children in all ways. The clinical picture of infection with the viral form is as follows:
- The appearance of pain and physical discomfort in the oral cavity.
- Increased body temperature, development of a febrile state.
- Formation of small blisters on the surface of the tongue and gums; rashes tend to merge.
- Formation of open wounds covered with plaque; their appearance occurs after the bubbles burst.
- The appearance of local hemorrhages on the mucous membranes of the oral cavity.
- Skin lesions and dysfunction of internal organs occur in the later stages in the absence of adequate treatment.
Is the bacterial form transmitted?
Bacterial form of stomatitis
This species is contagious. With stomatitis, the causative agent of which is a bacterial infection, the following symptoms are observed:
- Redness, loosening and swelling of the mucous membranes of the oral cavity.
- Localization of cracks and ulcers on the hard palate, gums and sublingual area.
- Bad breath that does not go away after brushing your teeth.
- Feeling of nausea, fever, general weakness and increased heart rate are symptoms that occur in severe forms of the disease.
Is it possible to get infected with a fungal form?
Fungal form of stomatitis
This disease can be transmitted. Signs of a fungal form
stomatitis are the following symptoms of the disease:
- Redness of the mucous membranes of the oral cavity, loosening of their structure and the appearance of local swelling.
- Formation of white plaque on the affected areas.
- Ulcerative lesions and crack formation, accompanied by pain.
Spread of aphthous stomatitis
Aphthous stomatitis
Aphthous stomatitis can be contagious or non-contagious, since this form of the disease occurs for various reasons.
Its main feature is not the type of pathogen, but the specificity of its course: the patient develops round erosive lesions with a white, gray or yellow tint on the mucous membranes.
Most often they occur in childhood and arise for the following reasons:
- Receiving mechanical injuries.
- Vitamin deficiency.
- Consequences of diseases of the digestive system.
- Emotional turmoil, frequent stress.
If the cause of aphthous stomatitis is a viral infection, other symptoms are observed, including redness and inflammation of the tonsils.
Traumatic stomatitis
Traumatic stomatitis
Traumatic stomatitis is not contagious to other people; depending on its causes, the following types are distinguished:
- The mechanical form occurs when the gums are rubbed with dentures, accidentally biting the mucous membranes, damaged by dental formations, chips and foreign objects, or a fall.
- The chemical form is a type of burn; it can be caused by ingestion of caustic chemicals, systematic consumption of alcohol-containing products, and active smoking.
- The physical form is a consequence of a thermal burn and can occur at any age as a result of too hot liquid entering the mouth.
Bacterial stomatitis
The bacterial form often occurs against the background of an underlying disease. Risk factors:
- Pharyngitis.
- Laryngitis.
- Rhinitis.
- Chronic tonsillitis.
- Angina.
When the immune system is significantly weakened, bacteria begin to multiply rapidly. Staphylococcus and streptococcus are common. Bacteria lead to the appearance of a purulent rash. The bubbles open, erosions and ulcers form.
Children transmit the disease to each other through household and contact routes. Toys and personal items become a breeding ground for pathogenic bacteria. One bath towel in a family for several members contributes to the fact that stomatitis will be detected immediately in a brother and sister or in a grandson and grandmother.
Transmission of bacterial stomatitis is not uncommon in children's groups. Adults become infected less frequently. For bacteria to get inside and begin their destructive activity, there must be damage to the skin or mucous membrane.
The slightest scratch may be enough if the body's defenses are reduced. But if an adult has a strong immune system, there is little chance of contracting bacterial stomatitis. The exception is representatives of the older age group. They experience an age-related decline in their defenses.
How to treat
Most often, the treatment procedure is limited to local exposure to the affected areas of the mucous membrane and soft tissue. Severe and painful lesions are treated with painkillers and antiseptic drugs, and applications with wound healing and anti-inflammatory agents are prescribed.
Viruses cannot be treated with antibiotics! Do not self-medicate or take potent drugs under any circumstances, they can only worsen the situation. To speed up recovery, your doctor may prescribe you medications containing human interferon (Viferon, Anaferon, etc.).
Also, for viral stomatitis, treatment can be aimed at eliminating local rashes using antiviral ointments (oxolinic, Zovirax, acyclovir and others). To increase the overall level of immunity, you will most likely be prescribed echinacea-based drugs, vitamins and immunomodulators.
At home, to speed up the healing of ulcers and sores, you can use herbal decoctions (sage, calendula, chamomile), oak bark for rinsing, and Tantum Verde spray for pain relief. Applications with retinol acetate and sea buckthorn oil are also very useful.
Among other things, diet is very important, without which treatment may not give the expected results. All foods consumed should be neutral in taste (no salt, acid, sugar or spices), in puree or porridge form, and lukewarm (hot and cold drinks and food are excluded). Under no circumstances should you refuse to eat because of pain.
Herpetic stomatitis
The disease is caused by the herpes simplex virus type 1. This form of stomatitis is contagious. The main symptoms include: headache, fever, weakness, ulcers on the oral mucosa, and enlarged regional lymph nodes.
Symptoms of stomatitis appear after contact with a virus carrier under the influence of unfavorable internal and external factors. The main cause of herpes stomatitis is considered to be weak immunity, but there are other factors: changes in the composition of saliva, systematic trauma to the mucous membrane, psycho-emotional stress.
The virus is highly contagious and spreads quite quickly in children's groups. It is transmitted by airborne droplets and contact: through toys, dishes, towels and hygiene products. Visible damage to the mucous membranes and skin of the face occurs, and a blistering rash appears.
IMPORTANT: The lack of adequate therapy at the initial stage can complicate the course of herpetic stomatitis by the addition of a secondary infection, resulting in deeper tissue damage and a deterioration in the patient’s well-being.
Types and routes of infection
The ways of transmission of the disease, depending on its type, are clearly demonstrated in the table:
| View | Contagiousness | Path of infection |
| Viral | Yes | Infection can occur in the following ways:
|
| Bacterial | Yes | Children:
Adults:
|
| Fungal (candida) | Yes | There is no airborne transmission; infection can occur by sharing dishes and cutlery with an infected person. Factors that increase the risk of infection:
|
| Aphthous | No | Aphthous stomatitis is contagious only when accompanied by a viral infection: in this case, the routes of infection are the same as for the viral form. |
| Traumatic | No | There is no person-to-person transmission. |
How the disease is transmitted
Any virus can be picked up in three possible ways: airborne, contact and directly through the blood. Thus, you can become infected anywhere - at work, in a cafe through poorly washed dishes, in children's groups (kindergartens, clubs and schools through toys and common objects), in entertainment centers (slot machines), in large supermarkets (pen carts and baskets), in public transport (handrails), in clinics and hospitals.
It is impossible to avoid transmission of the virus, but you can prevent it from getting inside by observing basic hygiene rules: wash your hands after going outside and before eating, before leaving home during epidemics, and also in the autumn-winter period use special antiviral ointments (oxolinic, viferon and etc.), always have sanitary napkins or hand sanitizer gel with you.
Pathogens and causes of fungal stomatitis (thrush in the mouth)
The causative agent of the disease is a yeast-like fungal microflora of the genus Candida (hence the name - candidal stomatitis ), and in the overwhelming majority of cases the species Candida albicans. But in more rare cases, fungal stomatitis can also be caused by other types of fungal microflora, for example, Candida tropicalis, krusei, parapsilosis, glabrata.
Fungi of this genus (there are 150 varieties, of which about twenty can cause candidiasis), almost always present on the tissues of the oral cavity, are normally harmless, but do not benefit the body. Their reproduction is controlled by many factors: the chemical balance in the mouth, local and general immunity, and competing bacterial microflora. When these factors are suppressed, the balance is disrupted and the fungus begins to multiply intensively. Actually, candidal stomatitis is not caused by the fungus itself, but by the enzymes it secretes that destroy the components and structure of the epithelium of the mucous membrane.
Candidal stomatitis
Candidiasis, also known as fungal stomatitis, often affects people suffering from oral diseases. Fungi of the genus Candida are ubiquitous. Thrush observed in women is caused by representatives of the same genus.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
The fungus is present in small concentrations in the body, but its uncontrolled reproduction begins with loss of vitality. Factors causing candidal stomatitis:
- Hormonal changes in the body.
- Constant stress , lack of sleep.
- Long-term treatment with antibiotics .
With this form of the disease, a dense white coating is noticeable on the oral mucosa. It concentrates on the gums, on the tongue.
Children under one year of age and the elderly most often suffer from candidal stomatitis. Parapsilosia is detected in infants. This fungal stomatitis is easily transmitted through dishes, toys, and hygiene items. One of the adults can infect a child with it by kissing the baby.
At the same time, the adult does not realize that he has a fungus, since it does not manifest itself in any way. A child can suffer the disease in an acute form: with fever, refusal to eat, and lethargy.
Types of stomatitis
Stomatitis is a pathology of the oral cavity, manifested as inflammation of the mucous membrane.
Older people encounter the glabrata species.
Most adults have a small amount of albicans fungus in their bodies. It does not pose a danger as long as there is no need to fight other infections. And only long-term illnesses can push the development of candidal stomatitis.
The routes of infection are standard. A sick person can transmit the fungus to a healthy person through kissing, shaking hands, or through airborne droplets. From the hands of someone in contact with the patient, the fungus gets onto the face and mucous membranes. If immunity is reduced, the content of immunoglobulins in saliva does not correspond to the norm - the development of the disease is likely.
Candidal stomatitis is difficult to treat because it is typical for weakened patients. It is necessary to protect such people from contact with sick people.
Popular questions
The following are popular questions about stomatitis that people often ask specialists:
- When kissing, there is a risk of contracting some forms of stomatitis.
Is stomatitis contagious from kissing? There is a risk of infection with a fungal, viral or bacterial form through saliva; especially if there are wounds in the mouth.
- Is it transmitted by airborne droplets? The viral, less often bacterial, form of the disease is transmitted by airborne droplets.
- Is it possible to get infected from a child? A healthy adult can rarely become infected with stomatitis from a child; the risk increases if you have diabetes in an adult or tonsillitis in a child.
- How many days is stomatitis contagious? In most cases - 8 days.
- Is this an infectious disease? Stomatitis has a complex classification, which also includes infectious forms.
- Is it possible to die from stomatitis? Stomatitis is not a fatal disease, but the lack of treatment can lead to intoxication of the body, damage to internal organs, the transition of some pathologies to a chronic form and other complications.
When the first symptoms of stomatitis appear, it is recommended to consult a specialist for diagnosis and confirmation of the diagnosis. Timely adoption of measures contributes to rapid recovery without complications; during therapy, it is necessary to remember safety measures so as not to infect other people.