04.05.2018
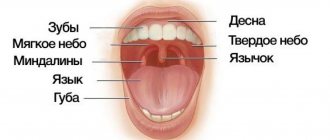
The oral cavity connects the body with the environment and can therefore be subject to a variety of negative influences. Such influences include the influence of too hot or too rough food, the influence of pathogenic microorganisms. In such cases, the first protective barrier is the mucous membrane, which lines the entire oral cavity and has, in addition to protective ones, many other functions. The mucous membrane is well supplied with blood, and its cells divide quickly and frequently. Therefore, wounds on the mucous membrane heal faster than on other parts of the body. However, for a number of reasons, the mucous membrane can be subject to inflammatory processes called stomatitis. Stomatitis is considered separately from such inflammatory processes in the oral cavity as gingivitis (inflammation of the gums; they have their own characteristics) and periodontitis (inflammation of the periodontium). The causes of stomatitis are very diverse.
Infectious causes
Stomatitis can be caused by infection with viruses or bacteria. In these cases, stomatitis is usually considered as an independent disease.
This is especially true for infection with herpes simplex viruses, which leads to very painful inflammation of the mucous membrane. There are two types of herpetic stomatitis - acute herpetic stomatitis (with primary infection) and recurrent herpetic stomatitis (which can pass through the acute stage or manifest itself as a general infection of the body in the presence of provoking factors). Herpetic stomatitis can lead to an aphthous form, in which erosions, aphthae, and even painful ulcers appear on the mucous membrane.
A specific type of stomatitis is chronic recurrent aphthous stomatitis, which begins almost immediately with the formation of aphthae, and the nature of which is not yet clear. But viral and bacterial infections and vitamin imbalances are also suggested as initiating factors.
The specific infection that causes stomatitis includes a fungal infection (fungi of the genus Candida) and the disease itself is called candidiasis (thrush). Thrush is characterized by the formation of whitish dots on the mucous membrane, and as the fungal infection multiplies, a whitish coating. Candidiasis develops, as a rule, as a result of violations of hygiene rules, physiological disorders in the body, and the use of certain medications. It is often observed in children and its danger cannot be underestimated. This infection, which initially appears on the oral mucosa, can be spread to all organs and systems of the body, and in this case already poses a significant threat to health.
Purely bacterial causes of stomatitis are less common. As a rule, bacterial infections affecting the oral mucosa accompany viral types of stomatitis (for example, streptostaphylococcal lesions).
Change in structure with fluid accumulation
With such lesions, the structure of the mucous tissue changes so that a cavity filled with liquid is formed inside.
Bubbles and bubbles. They are formed in the epithelial layer or under it, filled with serous or hemorrhagic contents, and can be grouped. The cavity is closed by a thin layer of epithelium, which can break through. Bubbles can group and break quickly. Bubbles form and last longer. Both types of lesions provoke the formation of healing ulcers on the surface of the mucous membranes. They arise due to damage by viruses, traumatic injuries, and disturbances in tissue nutrition.
Ulcers. They can form from blisters or on unchanged mucosa. The cavity is filled with purulent exudate (whitish, yellowish, greenish contents with a pungent odor). They can be deep or superficial, often painful. Indicate an inflammatory process, appear after traumatic damage to the mucous membrane, due to infectious, viral diseases.
Cysts. A formation with dense walls that form a cavity. It is filled with transparent contents (can become purulent, serous, bloody). Appear due to blockage of gland ducts on the mucous membranes or as a symptom of periodontal diseases.
Other causes of stomatitis
In addition to infections, there is a whole range of other causes that can cause inflammation of the oral mucosa: • allergic reactions of a local and general nature (for example, to certain foods, medications, filling materials, oral care products) • the presence of soft and hard dental plaque, multiple caries • incorrectly installed dentures or orthodontic devices (braces) • irritation and trauma to the mucous membrane (mechanical injuries, burns) • deficiency conditions in the body (vitamins A, B and C, iron, folic acid); • intoxication with nicotine, alcohol, metal compounds.
Stomatitis can be manifestations and side effects of common infectious diseases (measles, diphtheria) or internal and general diseases and pathologies (blood and skin diseases, hormonal fluctuations, metabolic disorders).
Inflammation of the oral mucosa occurs especially often when the body's immune system is weakened and due to insufficient oral hygiene. The danger of stomatitis may also be associated with increased and constant dryness of the mouth, in which the protective functions of the mucous membrane are sharply weakened. The salivary glands produce on average up to 1.5 liters of fluid per day, and its deficiency leads to an imbalance in the acidity of the environment, an imbalance of inorganic components and, ultimately, has a depressing effect on the immune defense of the mucous membrane.
3. Symptoms and diagnosis
Iron deficiency anemia is characterized by dullness of taste, pallor of the mucous membrane, painful reaction of the mucous membrane to sour or spicy foods, various false sensations (tingling, tingling, etc.), swelling and, less often, bleeding of the tongue, as well as inflammation along the red border of the lips (cheilitis) and multiple caries.
With hypoplastic anemia, hemorrhagic foci, swelling and cyanosis of the interdental papillae, and a tendency to expose the periodontal pockets are observed; in more severe cases, erosions or ulcers and areas of local necrosis appear on the oral mucosa.
B12-folate deficiency Addison-Biermer anemia is characterized by a yellowish-pale tint of the mucous membrane, glossitis (inflammation of the tongue), and in some cases, pinpoint hemorrhages on the mucous membrane.
As for leukemia, their existing classifications (based on etiological, cytogenetic and other criteria) include several dozen clinical forms, the analysis of which is beyond the scope of this material. Even the traditional division in medicine according to the type of course - into acute and chronic leukemia - in this case takes on a slightly different meaning: in fact, these are two different diseases, and they never transform into each other.
If we do not touch upon the main symptoms and limit ourselves only to changes in the oral mucosa (as in the case of anemia, see above), then acute leukemia is manifested by severe bleeding of the mucous membrane on the gums, cheeks (along the line of dental occlusion), on the upper palate, and tongue. Loose hyperplastic growth of the gums in the form of ridges that bleed at the slightest touch or spontaneously is often observed. In addition, pale necrotic areas surrounded by a bluish halo with an off-white or gray foul-smelling coating are often observed. Swallowing is difficult, eating causes pain in areas of necrotic ulceration; trophic disorders are often accompanied by activation of chronic infections (herpes, candidiasis).
Chronic leukemia, which can be latent for a long time, is also characterized by bleeding of the oral mucosa, but it is less pronounced than in acute leukemia, and hemorrhages occur mainly due to trauma or microtraumatization. A diagnostically informative sign is the combination of bleeding, cyanosis, and pallor of the mucous membranes in the absence of signs of inflammation.
In myeloid leukemia, erosive and ulcerative lesions of the oral mucosa often predominate; in chronic lymphocytic leukemia, infiltrating nodes with a loose consistency and bluish tint predominate.
If, during an examination by a dentist, orthodontist, otorhinolaryngologist, therapist or other specialist, there is a suspicion that specific changes in the oral mucosa may be caused by diseases of the hematopoietic system, a consultation with a hematologist is strictly necessary, followed by an in-depth laboratory blood test , the results of which are the most informative and decisive in making a diagnosis. As necessary, other laboratory and instrumental studies are prescribed (imaging diagnostic methods, bone marrow puncture followed by histological analysis, etc.).
About our clinic Chistye Prudy metro station Medintercom page!
Main symptoms of stomatitis
Symptoms of stomatitis depend on its type and form, are very diverse and specific. General symptoms include redness, swelling of the mucous membrane, burning and pain in the mouth (including when eating hot, sour or spicy foods), an increase (or, conversely, a decrease) in salivation, bad breath, as well as the manifestation, in depending on the severity of the disease, specific lesions - erosions, af, ulcers.
Therapy for diseases of the oral mucosa
Prevention measures:
- Visiting the dentist twice a year to promptly identify and eliminate dental problems;
- Careful observance of local hygiene;
- To give up smoking;
- Avoiding too hot and spicy foods;
- Rinsing the mouth with disinfectant solutions and herbal decoctions;
Oral hygiene should be carried out regularly. Failure to comply with basic rules can provoke the occurrence of sore throat, problems with the gastrointestinal tract and other pathologies.
The health of the oral mucosa largely depends on the condition of a person’s teeth.
To successfully cure any disease of the oral mucosa, it is necessary to suppress the factors that influenced its development. If you suspect any problems in the oral cavity, you should contact a specialist. It is categorically unacceptable to get too carried away with self-medication and resort to non-standard methods of treatment. If you do not see a doctor for a long time, a minor problem can develop into a more serious one, lead to complications and worsen a person’s overall health. In addition, some oral diseases can develop into malignant ones. You should not put off visiting a specialist and expect the disease to go away on its own. Timely diagnosis and treatment will help avoid many problems in the future.
Treatment
The primary diagnosis of the disease based on clinical manifestations is carried out by a dentist, who also carries out local symptomatic treatment based on the primary diagnosis. But in complex and unobvious cases, laboratory diagnostics are carried out, and doctors of other specialties (allergists, dermatologists, immunologists) are brought in for treatment.
Local symptomatic treatment usually involves the use of rinses with solutions of painkillers and antiseptic drugs (including herbal origin), the use of drugs for tissue regeneration (after the acute phase subsides), if necessary, the elimination of irritating and provoking factors (removal of dental plaque, hard deposits, treatment dental caries).
Local drug treatment is carried out only after an accurate diagnosis has been established (the cause of stomatitis) and usually includes treatment with antiviral, antibacterial, antifungal drugs in the form of ointments and applications.
General treatment is carried out, as a rule, in a hospital and is aimed at eliminating the internal causes of stomatitis (treatment of internal pathologies), taking therapeutic drugs according to special regimens, and physiotherapy.
Prevention
In general, it is quite difficult to avoid this disease in the presence of predisposing causes; you can only take some general measures to possibly prevent the disease or complication in the form of stomatitis.
Since the herpetic virus, especially in acute primary forms, is extremely contagious, a certain isolation of the patient is required to prevent the spread of infection by airborne droplets and contact. The difficulty here is that there is a rather long incubation period, up to 26 days, and the first signs of stomatitis may escape attention.
Other preventive measures are of a general nature and consist of proper and complete oral hygiene, regular professional cleanings in a dental clinic (removal of soft and hard plaque), timely treatment of mucosal injuries, and measures to generally strengthen the immune system.
Posted in Useful information | Tags: teeth, diabetes, care