Probably one of the most terrible pains a person can experience is toothache. When a tooth hurts, it is almost impossible to endure, and then even the most ardent dentist-hater goes to “surrender” to the doctor. But not everyone knows why teeth hurt and how to avoid these unpleasant sensations. Together with the dentist-therapist of the StilDent clinic, Elena Gennadievna ZIBNITSKAYA, we will look at the most common causes of toothache.
The most common causes of toothache are caries, pulpitis, periodontitis and pericoronitis.
Caries
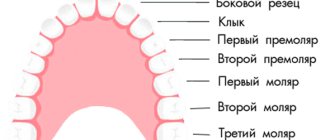
This is a disease of the hard tissues of the tooth, leading to the destruction of enamel and dentin. First of all, caries affects the natural depressions on the teeth (fissures), as well as areas where plaque accumulates in large quantities - these are the interdental spaces and the gingival area. With caries, the hard tissues of the tooth demineralize and soften, and subsequently a defect in the form of a cavity forms on the tooth.
Caries has several stages, the process can be initial, superficial, medium and deep. At first, caries is almost asymptomatic - the main inconvenience that a person experiences is associated with food getting stuck in carious cavities. Another symptom of caries, which is usually not paid much attention to, is short-term pain from chemical, mechanical, and temperature irritants. Simply put, damaged enamel no longer protects the tooth from the effects of hot tea or ice water or from mechanical stress, and at this moment we experience pain. But because it only lasts a few seconds, we usually don't take it seriously.
When the process reaches the last stage - deep caries, the unpleasant sensations become difficult to ignore. With deep caries, the patient experiences pain when food and liquid enter the damaged area, pain when brushing teeth (irritation from paste and brushes), pain from any external irritants, temperature, chemical, mechanical. Once the irritant is removed, the pain subsides until the next episode. At this stage, the quality of life is already significantly reduced. But if a person continues to stubbornly endure and does not go to the doctor, the nerve of the tooth (pulp) is gradually involved in the inflammatory process, and pulpitis begins.
Therapy and rehabilitation
Treatment of the disease is carried out by two methods - conservative and surgical. The choice of method depends on the form of the disease, its severity, and the course of the disease. In the early stages of development of the pathological process, conservative treatment is possible by prescribing a complex of drugs:
- broad spectrum antibiotics
- anti-inflammatory;
- painkillers;
- antipyretic.
IMPORTANT! Conservative treatment requires careful compliance with all doctor’s instructions until the process is completely eliminated. Otherwise, there is a risk of the disease becoming chronic.
Purulent periostitis is treated by wide opening of the purulent sac with dissection of the periosteum to the bone. At the same time, the issue of treating the tooth that caused the inflammatory process is being resolved. Most often, such a tooth is removed. After removing the pus, medications are prescribed, including antibiotics, anti-inflammatory and painkillers. Additionally, physical therapy may be prescribed: UHF, microwaves. The patient is recommended to frequently rinse the mouth with a solution of baking soda or sage tincture.
Simple periostitis requires complete rest of the injured area and treatment with physiotherapeutic procedures. All other types are reduced to treating the underlying disease or eliminating the focus of fibrous tissue growth.
IMPORTANT! Under no circumstances should you treat flux yourself. It is especially not recommended to pierce a purulent sac: there is a high risk of infection in neighboring tissues.
To speed up the treatment and recovery processes, you can resort to traditional medicine methods.
Pulpitis
This is an inflammation of the pulp (nerve) of the tooth, the process is usually accompanied by acute pain. Pulpitis occurs as a reaction to constant exposure to irritants that enter the pulp through a carious cavity, as well as due to the influence of microorganisms and toxins on the nerve of the tooth. Irritation of the pulp leads to a change in blood flow, which provokes increased pressure on the nerve fibers.
At the initial stage, pulpitis manifests itself as mild pain, which goes away when the irritant is removed. At this stage, the inflammation goes away on its own if the irritant is removed - that is, caries is cured and the tooth is filled, isolating the pulp from external influences.
If you do nothing, the inflammation gradually intensifies and the pain increases. The stage of acute pulpitis begins, irreversible changes occur in the pulp. Pain is easily caused by any irritant. The “don’t eat, don’t drink, keep your mouth closed” option doesn’t save you from pain. Very often, toothache worsens at night.
Pain in acute pulpitis can be very different:
- Sharp or blunt
- Pulsating or constant
- Localized or spilled
- Short or long term
If you continue to ignore your condition and do not consult a dentist, then the next stage is complications that are likely to develop with acute pulpitis, including purulent pulpitis.
Will painkillers help?
If a very severe toothache does not go away, and massage and other non-drug methods do not help, you will have to take painkillers. There are 4 groups of drugs that are used against toothache:
Based on ibuprofen, ketoprofen, nimesulide and ketorolac:
considered one of the best for eliminating acute toothache in the jaw, they are considered non-steroidal drugs. However, these are still not completely harmless substances, since they put a strain on the kidneys and liver.
Based on paracetamol:
do not relieve inflammation, but block pain impulses sent to the brain. That is, the tooth hurts, but the person feels the pain less intensely.
Based on analgin and aspirin:
can slightly reduce pain due to the anti-inflammatory effect. However, aspirin reduces blood clotting, so you should not drink it to reduce pain after tooth extraction.
Antibiotics:
have antimicrobial properties, but are unable to quickly relieve pain. They allow you to reduce inflammation during toothache only after a long course, and after that the pain will return. Therefore, you should take antibiotics only if you have been without access to places where you go for toothache for a long time, and there is nothing other than antibiotics in your first aid kit.
It is important to understand that none of these drugs will get rid of the cause of toothache - after taking them, the intensity of the discomfort will only decrease temporarily. Many, well aware of this, continue to ignore the problem, switching to regular medication. Under no circumstances should you do this, since you will not only not eliminate the problem, but you will acquire a lot of new ones - painkillers have many limitations and negatively affect other human organs.
Chronic pulpitis
In the most patient patients, acute pulpitis can become chronic. The pain becomes less acute and constant, sometimes subsides for a long time. If the carious cavity is difficult to access by irritants, chronic pulpitis can be almost painless.
Symptoms of chronic pulpitis
- Pain in the cold
- Pain when eating hot food
- Pain during temperature changes (for example, when you leave the house on a cold street)
- Prolonged aching pain if the carious cavity is clogged with food debris
Chronic pulpitis can worsen at any time and give you all the unforgettable sensations of acute pulpitis.
If chronic pulpitis is not treated, it can develop into periodontitis.
Prevention
Flux is easier to prevent than to treat. Prevention methods are simple and known to almost everyone. They consist of timely treatment of carious teeth, timely removal of the gum hood from wisdom teeth, the correct choice of toothbrush and toothpaste, and timely replacement of oral hygiene products. It is recommended that you visit your dentist at least twice a year and have your teeth professionally deep cleaned to remove plaque at least once a year.
IMPORTANT! Don’t forget about strengthening your immune system and giving up bad habits.
Dental flux is an unpleasant disease that requires treatment by specialists at an early stage of development. Self-medication in case of periostitis is unacceptable. With a favorable course and initial stage of development, conservative treatment is possible, but most often they resort to the surgical method.
Acute periodontitis
Periodontitis is an inflammatory process in periodontal (periodontal) tissues in the area of the apex of the tooth root. Often, inflammation involves the cementum and dentin of the tooth root, as well as the alveolar bone. Periodontitis in most cases occurs due to damage to the pulp, that is, pulpitis.
Symptoms
- The pain is constant, throbbing, with clear localization
- The pain intensifies from any touch to the tooth, including when chewing
- Pain may spread to part of the face
- Headache
- General weakness
- Temperature increase
- Cheek swelling
- Pain in the gum, redness and swelling in it
- Submandibular and chin lymph nodes are enlarged
- Possible discharge of pus from the root canal
What to do if you have a toothache?
The answer to the question: “What is better for toothache?” - can be only one. This is a visit to the dental clinic. However, the time and place do not always allow this to be done without delay. In this case, you can try to relieve the pain yourself. Here are some first aid options for toothache:
- If discomfort occurs when eating food, brushing your teeth or rinsing with warm water/soda solution will help against toothache and swelling of the gums. You can also use a decoction of chamomile, mint, oregano, St. John's wort and sage.
- Refrain from chewing food with a sore tooth.
- For some time, severe toothache can be pacified by applying a piece of ice to the sore tooth.
- Acupressure of the hands in the area where the bones of the index and thumb touch will help reduce the intensity of pain. Nerves pass through this zone, and massage helps to “deceive” them, switching attention to another stream of information.
Important!
Often, with the most severe toothache in an adult, it is recommended to apply honey or cotton wool soaked in strong alcohol to the tooth so that under their influence the nerve stops sending pain impulses to the brain. But can such a compress eliminate toothache? Depends on the specific clinical case. Sometimes this is really a solution, and sometimes this method can provoke even more severe inflammation.
Before and after dental treatment at the Ilatan Clinic. Works by Zarivny S.S.
Chronic periodontitis
Chronic periodontitis sometimes develops asymptomatically, or acute periodontitis can progress to this stage. Chronic periodontitis develops when the pulp dies, and favorable conditions are created in the tooth for the development of microorganisms. Sometimes chronic periodontitis can appear after a tooth injury.
Symptoms
- Changing the color of tooth enamel
- The presence of a fistula on the gum
- Painful sensations when chewing solid food
Chronic periodontitis can have many very serious complications: granuloma, root cyst, pathological fracture of the lower jaw, periapical abscess, phlegmon and others.
Etiology and pathogenesis
The development of periostitis most often occurs with inflammatory diseases of the oral cavity and teeth, pulpitis and periodontitis. Also, the development of purulent inflammation of the periosteum can occur after jaw fractures, injuries and wounds of the soft tissues of the cheek, after treatment with anesthesia. Through damage to the dental tissue, gums or cheeks, the pathogen enters the jawbone, causing inflammation.
Acute periostitis can develop as a result of acute or chronic periodontitis, with suppuration of odontogenic cysts, and difficulty in teething. The process begins with the inner layer of the periosteum, gradually spreading to all other layers. Periostitis occurs when the focus of primary infection of the tooth canal or gum is blocked and its contents penetrate into the periosteum. The exudate penetrates through small holes in the alveolar plate through the channels.
Less commonly, flux develops in diseases of the pharynx (sore throat, pharyngitis, laryngotracheitis) or in the presence of a focus of infection in the body, from where it can be transferred to the periosteum with the blood or lymph flow.
When examining purulent contents during purulent periostitis, staphylococci (Staphylococcus aureus is one of the main causes of flux development), streptococci, various types of bacilli and putrefactive bacteria are often found.
Reference! 25% of all pathogenic microflora during flux are aerobic bacteria, the rest is anaerobic forms.
General factors influencing the development of the disease:
- weak immunity;
- hypothermia;
- stressful situations;
- poor oral hygiene;
- carious processes in teeth;
- old fillings;
- frequent medical interventions;
- bad habits.
Forms of periostitis
Depending on the cause of the flux and its course, we talk about its forms:
- Acute: simple – occurs as a result of a bruise of the face, with fractures and injuries of the jaw bones;
- purulent – penetration of periodontal infection to the periosteum;
- tuberculosis - when Koch's bacillus is carried into the periosteum and bone tuberculosis;
- syphilitic - as a complication of congenital or acquired syphilis.
- ossifying – chronic form with the development of compactions in the form of bone tissue;
Pericoronitis
This is difficult eruption of wisdom teeth (eights). When a tooth cannot erupt normally, inflammation of the surrounding soft tissue and periosteum behind the dental socket begins. Inflamed gums are constantly injured when chewing, which further aggravates the process.
The inflammatory process can gradually lead to the development of purulent pericoronitis.
Symptoms:
- Constant pain that gets worse when chewing
- Pain radiates to the ear and temporal region
- Pain when opening the mouth
- Enlargement and tenderness in the submandibular lymph nodes
- Sharp pain when pressing on the gums, purulent discharge is possible
- Increased body temperature
In the future, the pain continues to intensify and the body temperature rises. The patient's health deteriorates significantly, and retromolar periostitis may develop.
Symptoms of tooth inflammation
Inflammation is the body's response to bacterial attack. Tissues begin to produce immune cells, signaling the hematopoietic organs that more white blood cells are needed. As a result, the vessels dilate, and the place where the microbes have penetrated swells and turns red. Nerve endings connect the pain syndrome so that we react as quickly as possible.