Causes of pain in the face and head
Headaches that radiate to the face can have different origins. In some cases it is primary (migraine, cluster pain, tension headache), in others it is one of the symptoms of diseases of the nervous system, musculoskeletal system, heart and blood vessels. It is important to take into account the exact localization of painful sensations, their nature and intensity, and the conditions of occurrence.
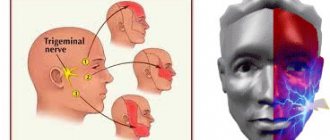
Trigeminal neuralgia
The trigeminal nerve is a paired nerve and represents the fifth pair of cranial nerves. In the temporal region it is divided into 3 main branches: the ophthalmic, maxillary and mandibular nerves. They provide facial skin sensitivity, motor activity of the facial and masticatory muscles. When the trigeminal nerve becomes inflamed or damaged, an acute headache begins, which spreads along the nerve fibers. It is so intense that during the period of exacerbation of trigeminal neuralgia, patients cannot touch their face, eat food, turn or tilt their head.
The cause of neuralgia is inflammation of the nerve or its mechanical damage. There are also several factors that can contribute to the development of acute pain:
- viral respiratory diseases, as well as herpes virus infection;
- neoplasms in the cerebellopontine region of the brain;
- dental diseases, including stomatitis, periodontitis and others;
- acute purulent inflammation of the paranasal sinuses (sinusitis);
- atherosclerosis is a disease in which arterial blood flow deteriorates and the supply of oxygen to brain tissue decreases;
- bruises, injuries in the facial area, which are accompanied by damage to nerve fibers.
Headache with trigeminal neuralgia can spread to any part of the face. It is sharp, throbbing, and can be confused with pain caused by dental problems. In some patients, the disease is chronic and worsens at regular intervals. More often this happens in the winter and in the off-season - inflammatory reactions are caused by a sharp drop in temperature and the effect of a viral infection. During an attack, additional symptoms are also felt: increased lacrimation in response to bright lighting, cold weather and decreased sensitivity of the facial skin, involuntary contractions of the facial and masticatory muscles.
In most cases, treatment of trigeminal neuralgia is carried out with medication. The doctor prescribes antibiotics, antiviral and anti-inflammatory drugs. To make you feel better, you will need painkillers. Some patients require surgery to destroy the trigeminal nerve root or remove pathological formations that exert mechanical pressure on the nerve. Physiotherapy is also useful as treatment and rehabilitation.
Cluster pain
Main article: Cluster headaches
Cluster headaches are the least common type. They are characterized by a very high degree of intensity and do not have an exact cause. An attack consists of a series of pain sensations in the area of the projection of the brain onto the human skull. It is so acute that the person cannot continue to carry out daily tasks during this time, and conventional over-the-counter analgesics are ineffective.
Cluster headaches have several features:
- first appears in adulthood, most often from 20 to 30 years;
- has no warning symptoms, begins abruptly, at any time of the day;
- extends only to one half of the head;
- accompanied by deterioration of vision, constriction of the pupil, increased heart rate, redness of the skin;
- the period lasts from several days to several months - during this time the patient experiences on average 1-3 headache attacks per day, often at the same time.
Cluster pain is more common in women . There is no hereditary predisposition, since the disease in most cases is found in only one family member. After the end of the exacerbation period, a long-term remission is observed. It can last up to 3 years, during which the pain does not bother the patient. A seasonal course of the disease is also possible if it appears only at certain times of the year.
Migraine
Main article: Chronic migraine
Migraine is one of the types of primary headaches. It is often one-sided and affects only one half of the head. Painful sensations can be of varying degrees of intensity, but most often acute. The exact cause of migraine is unknown. It often develops in response to factors such as changes in weather and atmospheric pressure, stress and emotional tension, intense physical activity, disruption of the daily routine, as well as smoking and frequent alcohol consumption, poor diet, and hormonal changes.
Migraine is a one-sided headache. There are several theories of its origin - doctors explain its appearance by vascular, nervous, and hormonal disorders. Migraine can occur in different ways, but the classic form includes several stages:
- The initial stage is prodromal. It begins a few days before a headache attack. During this period, a person’s mood often changes, irritability and fatigue appear, concentration and performance deteriorate. This symptom complex does not occur in all patients, but its appearance accurately indicates the onset of migraine.
- Aura (Main article: Migraine with aura) is the period several hours before an acute headache. It is typical for migraine, but also does not necessarily occur. Its cause is considered to be spasmodic contraction of brain vessels and deterioration of its blood supply. The aura is manifested by increased sensitivity to sunlight, the appearance of bright circles and dark spots before the eyes, as well as hearing impairment and severe fatigue.
- The immediate attack of headache lasts several hours, but in some patients it may not stop for up to several days. It is acute, one-sided, and intensifies in the presence of external stimuli (bright light, loud sounds). Painful sensations are concentrated in one half of the head and can spread to the face and neck. Symptoms such as lacrimation, nausea and vomiting, and dizziness are also typical.
- Resolution stage – lasts 1–2 days. Some patients feel better immediately after the headache ends, but resolution may be slow. Symptoms include weakness, decreased alertness, and increased sensitivity to bright lights and loud noises.
According to statistics, migraines are more common in middle-aged women. To treat it, a set of medications is prescribed that help reduce pain and shorten its duration. If attacks occur frequently and do not stop for 3–5 days or more, hospital treatment may be necessary. The procedures are aimed at preventing complications: dehydration, cerebral edema, seizures, heart attack and stroke.
Somatogenic facial pain
Pain in the face and head can be somatogenic (secondary), that is, associated with diseases of other organs and systems. They are less intense than cluster pain, migraine and facial neuralgia, but also affect performance and can cause complications. Common causes of pain in the face are dental diseases, inflammation of the paranasal sinuses, and ophthalmological problems.
- Toothache – often spreads to the scalp, skin, muscles and nerves of the face. It is often associated with inflammatory processes and dental caries. Symptoms such as pain in the jaw joints, pain when chewing, or eating cold or hot food and drinks also occur. To make you feel better, consultation with a dentist, medication, and, if necessary, surgery are recommended.
- Joint pain is another type of somatogenic pain. They are often triggered by arthritis or arthrosis of the temporomandibular joint, its deformation or injury. In addition, soreness may be a sign of a malocclusion, tooth loss, or discomfort when wearing dentures.
- Inflammation of the paranasal sinuses is a group of dangerous diseases. The sinuses (sinuses) are cavities formed by the bones of the skull. Normally, they are empty, filled with air and necessary for proper breathing. Their inflammation is accompanied by the appearance of aseptic or purulent contents, an increase in body temperature, a sharp deterioration in health and nasal congestion. The most common type of sinusitis is sinusitis. It develops as a result of hypothermia, the proliferation of a viral, bacterial or fungal infection, head injuries and bruises.
- Eye diseases also cause headaches. When diagnosing pain, glaucoma may be detected - increased intraocular pressure. This is a dangerous condition that requires immediate treatment. Increased pressure causes compression of blood vessels and nerves, and over time can lead to poor vision and even complete blindness.
If a patient complains of pain in the face and head, a comprehensive examination is prescribed. The scheme will include general diagnostics, as well as consultations with specialized specialists: ophthalmologist, otolaryngologist, dentist and others.
Other reasons
Soreness is a symptom of a number of disorders that do not necessarily indicate dangerous diseases. Headaches can occur periodically in a healthy person, and then go away on their own or after taking painkillers. Doctors identify a number of reasons that can cause deterioration in health:
- stress, nervous tension;
- sleep disturbances caused by insomnia, moving to regions with a different time zone, irregular schedules, or working at night;
- poor nutrition, an abundance of fatty foods, flour products, spices and sweets in the diet;
- intense physical activity;
- sudden changes in weather, temperature or atmospheric pressure;
- hormonal changes.
Doctors recommend calling for a full examination if headaches continue for several days or more. Also dangerous are acute pains that affect performance and are accompanied by additional symptoms: nausea, vomiting, impaired coordination of movement, and memory impairment.
Causes of prosopalgia
An inflammatory reaction can act as an etiofactor of facial pain. Most often, prosopalgia of inflammatory origin occurs with sinusitis. It can be observed in otitis media, ophthalmological diseases (iridocyclitis, uveitis, conjunctivitis, keratitis, corneal ulcer), TMJ arthritis, and have an odontogenic etiology (pulpitis, periodontitis). Prosopalgia can occur with inflammatory lesions of the vessels of the facial area, for example, with Horton's disease. Often, neurogenic prosopalgia has an inflammatory etiology with neuralgia of the glossopharyngeal nerve, trigeminal nerve, Oppenheim syndrome, ganglionitis of the pterygopalatine ganglion, ganglioneuritis of the geniculate ganglion.
On the other hand, neurogenic prosopalgia may have a compression genesis, i.e., arise as a result of compression of nerve trunks or nodes due to changes in the relative position of the anatomical structures of the facial area, narrowing of bone and intermuscular nerve canals, development of tumor formations, etc. Compression etiology may have vascular prosopalgia, for example, carotidynia due to compression of the carotid artery.
The reflex mechanism of pain syndrome is often realized in odontogenic and neurogenic facial pain. The cause of prosopalgia in such cases is pathological reflex impulses coming from chronic infectious foci. An example is neuralgia of the ear ganglion. Myogenic prosopalgia of reflex genesis occurs with myofascial syndromes in the neck and shoulder girdle. Other causes of myogenic prosopalgia may include TMJ dysfunction (Costen syndrome), bruxism, and myofascial syndrome in the masticatory muscles.
Prosopalgia of psychogenic origin often occurs in suspicious, emotionally labile people against the background of overwork, chronic psycho-emotional discomfort, or as a result of an acute stressful situation. Often, psychogenic prosopalgia is observed in persons with hysterical neurosis, neurasthenia, and depressive neurosis. It can occur as part of psychiatric diseases such as schizophrenia, psychopathy, manic-depressive psychosis.
In some cases, prosopalgia is iatrogenic. Thus, Oppenheim syndrome can occur after ophthalmological operations; tooth extraction and other dental interventions can trigger the development of dental plexalgia or atypical odontalgia. One of the causes of neurogenic facial pain is damage to nerve structures during operations in the facial area. In addition, a number of facial pains do not have a clearly established etiology. For example, cluster headache, atypical prosopalgia, chronic paroxysmal hemicrania.
Diagnostic methods
For effective treatment, it is important to determine the exact cause of the headache and facial area. It is impossible to carry out diagnosis on your own, since it requires the use of precise equipment and laboratory tests. The complex may include the following activities:
- blood tests - prescribed to determine inflammatory processes, bacterial infections and various diseases of the heart and blood vessels;
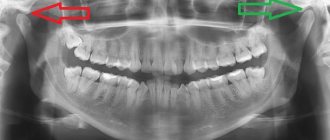
- X-ray is one of the examination methods for suspected diseases of the teeth and temporomandibular joint;
- MRI, CT scan of the brain;
- ophthalmological examinations aimed at diagnosing vision and measuring intraocular pressure;
- assessment of the condition and conductivity of the vessels of the neck and head - carried out by radiography using a contrast agent.
The Clinical Brain Institute offers headache diagnostic programs. The set of measures is selected individually, based on the results of the inspection. To obtain accurate data, it is important to notify the doctor about all conditions for the occurrence of pain, their nature and intensity, and also undergo the prescribed examinations.
Classification of prosopalgia
Facial pain is classified primarily by mechanism of development. Prosopalgia is distinguished:
- vascular
- neurogenic
- myogenic
- psychogenic
- symptomatic
- atypical
- painful ophthalmoplegia
Vascular facial pain
includes:
- bundle cephalalgia
- paroxysmal hemicrania
- Horton's disease
- idiopathic sudden cephalalgia (ISH)
- SUNCT syndrome.
Neurogenic prosopalgia
includes:
- trigeminal neuralgia
- neuralgia of the glossopharyngeal nerve
- ganglionitis and ganglioneuritis of the nerve ganglia of the facial region.
Symptomatic facial pain
. Depending on the etiology, symptomatic prosopalgia is divided into
- ophthalmogenic
- odontogenic
- otorhinogenic
- viscerogenic.
To atypical
include pain that does not fit into the clinical picture of any of the types of prosopalgia specified in the classification. They are often caused by a combination of several pathogenetic mechanisms and have a psychogenic component.
Treatment of headaches and facial pain
The treatment regimen for headaches and pain in the face is selected individually. It will include measures to eliminate the underlying disease, as well as to relieve symptoms. Based on the diagnostic results, the doctor may prescribe the following methods:
- drug treatment - may include anti-inflammatory and painkillers, antibiotics, drugs to improve cerebral circulation;
- physiotherapy – carried out to stimulate blood circulation and innervation in the face and head;
- diet for blood vessels - includes simple foods, with a minimum amount of fried foods, animal fats, fast food and spices;
- surgical intervention - most often prescribed for mechanical compression of nerves and blood vessels, in the presence of neoplasms and dental diseases, as well as for clearing the contents of the paranasal sinuses.
Doctors at the Clinical Institute of the Brain will select appropriate treatment tactics based on the results of a general examination. For most patients, it is enough to take medications, follow a diet and adjust their daily routine to improve their health. However, for some diseases surgical intervention is indicated.
INFECTIOUS PAINS
Subcutaneous infections on the face are most often caused by staphylococcus. If the immune system is weakened, bacteria are activated: a boil forms under the skin. It can ripen for several days, and all this time it causes pain on the skin. Without treatment, the process of boil maturation is delayed, and the infection finds more and more new foci. Infection of the facial nerve is an extremely undesirable complication. A typical sign is a distorted face, swelling is visible at the site of the boil. In this case, an integrated approach is required: not only to eliminate the infection, but also to restore the damaged nerve and strengthen the immune system.
IF SUCH SYMPTOMS OCCUR, IT IS IMPORTANT TO SEE A DOCTOR IMMEDIATELY!
Prevention methods
Timely prevention is the key to good health at any age. It is important to form the right habits that will have a positive effect on the health of the heart and blood vessels, teeth and other organs. Doctors recommend:
- eat right, get enough vitamins and microelements;
- give up bad habits - smoking and drinking alcohol affect the condition of blood vessels;
- normalize your daily routine and devote enough time to rest;
- carry out moderate physical activity to train the heart muscle.
At the Clinical Brain Institute you can undergo an accurate and high-quality diagnosis of headaches and pain in the face. There is modern equipment here that can be used to determine the causes of pain. Doctors will also select an effective treatment regimen for use at home or in the hospital of our center.