The formula will help determine the condition of the mouth
To determine the condition of the oral cavity in medicine, there are about 80 different hygiene indices, based on the principle of staining the enamel with a special solution and identifying dental plaque.
According to the parameters they define, indices can be classified into 4 groups, assessing:
- area affected by plaque;
- thickness of plaque on teeth;
- mass of plaque;
- other parameters of dental plaque (chemical, physical and microbiological).
Determination of the oral hygiene index: interpretation of results
The culmination of the study was the correlation of the resulting number with the index table. If the patient’s figure was close to one to one and a half, then oral care can be considered good. From one and a half to two - the patient takes satisfactory care of his teeth; from two to two and a half, hygiene was considered unsatisfactory. Figures over 2.5 were considered poor (2.6–3.4) and very poor (3.5–5) results. In this way, it was possible to assess whether there was plaque and how well the patient cleaned it off.
Determining the oral hygiene index is not the only method; similar calculations are applied to other parameters, in particular to dental calculus.
CPU in dentistry
Dentists should use these calculations during the initial examination of the patient. So, for example, the average values of the indices KPU, kp. KPU+KP of teeth and cavities in dentistry allows you to determine the intensity of carious lesions. These abbreviations contain the following meanings:
- K – carious permanent teeth;
- P – permanent teeth in which a filling is installed;
- U – extracted molars;
- j – temporary teeth affected by caries;
- p – filled temporary teeth.
- According to the World Health Organization, the average CP index for children 12 years old should be from 2.7 to 4.4, and for citizens aged 35-44 years 6.3-12.7.
Silnes-Lowe Index
Using such an index, it is possible to estimate the thickness of plaque deposits near the gums in four areas of tooth enamel: vestibular, lingual, distal, mesial. The surface is dried, and then the tip of the probe is used to move along it near the gingival sulcus. A clean probe allows you to talk about zero points. When the coating is invisible, but sticks to the device, they set it to one. If the plaque is thin or medium, you can give it a 2. When the plaque clearly affects the areas near the gums and between the teeth, you can give it a three.
Silnes-Lowe Index
Important! The general index is the indices of specific teeth obtained as a result of the study, divided by their number in the mouth.
Simplified index (IGR-U)
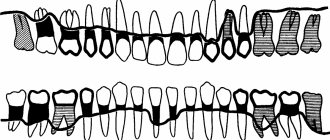
The Green Vermillion Hygiene Index measures plaque and tartar on the surfaces of the 2 upper first molars, 2 lower first molars and 2 upper incisors.
Ratings are given as follows:
- 0 – no plaque;
- 1 – no more than 1/3 of the tooth surface is covered with plaque;
- 2 – plaque affects from 1/3 to 2/3 of the tooth;
- 3 – dental plaque covers more than 2/3 of the surface.
The simplified hygienic index is calculated by adding the plaque index and tartar index on 6 teeth.
Silness-Lohe method
In periodontics, preference is often given to the Silness-Lohe technique, which is based on determining the amount of soft plaque in the gingival zone. The essence of the method is simple: the dentist runs the end of the probe along the neck of the tooth, capturing the gingival groove. If the instrument does not capture plaque at all, a score of 0 is given. If the amount of plaque is small - 1. If a thin layer of plaque is noticeable near the neck of the tooth, and a significant amount is retained on the probe - 2. If a large amount of plaque and food is visually determined in the area where the gum adjoins the tooth. residues - Z. The indicators of all teeth are added up, the result is divided by the number of teeth.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
PMA – papillary-alveolar-marginal index
When calculating the PMA index, a solution of iodine or Lugol is used, which is applied to the gums and the degree of tissue inflammation is determined by the reaction to the irritant.
The evaluation criteria are:
- 1 – if the papilla (P) is inflamed;
- 2 – in case of inflammation of the marginal edge (M);
- 3 – inflammation of the alveolar part of the gum (A).
Formula RMA = Sum of points/n*3 (in percentage), where n is the number of teeth (up to 6 years – 20 teeth; 6–12 years – 24 teeth; 12-14 years – 28 teeth; over 15 years – 30 teeth) .
If the value is less than 30%, then the degree of damage is mild, 31-60% is moderate, 61% or more is severe.
Methods used
The objects of index assessment are destructive and inflammatory processes developing in periodontal tissues, the existence of deposits, periodontal pockets, tooth mobility, etc.
There are many research methods, but not all of them receive equal attention from doctors. The most accurate and frequently used research techniques are the following methods.
Papillary-marginal-alveolar index (PMA)
Refers to the basic group of indicators. It was first proposed in 1948 by Massler M. and Schur D. to obtain complete information about gingivitis - to identify its presence, study the severity and depth of penetration. Can be expressed as a percentage (1960 Parma S.) or in absolute numbers.
To detect pathology, the marginal or alveolar gingival zones and interdental papillae are studied.
During the study, the surface facing the lips and cheeks (i.e., vestibular) is covered with a solution with an iodine component. Inflamed areas turn dark brown.
To indicate the presence/absence of a disease, to assess the intensity of the disease, the following encoding is used:
| Code | Result |
| There is no disease. | |
| 1 | Only the gingival papilla is inflamed. |
| 2 | The pathological process occurs on the marginal surface and in the papillae. |
| 3 | The inflammation also spread to the alveolar zone. |
After analysis, the index is calculated using the expression:
RMA = sum of examined elements X per 100: per 3 X per n ( n – number of examined teeth).
The coefficient n is determined by the age of the patient being examined:
- n = 24 – 6-11 years;
- n = 28 – from 12 to 14 years;
- n = there is no exact coefficient, but a number is indicated equal to the number of teeth present in the jaw row.
Explanation of the PMA indicator:
- less than 30% - there is a mild form of inflammation;
- from 31% to 60% - average;
- over 60 – severe.
For the purpose of prevention, this index is used:
- when the disease is detected at an early stage of development;
- to examine the quality of periodontal tissues in dental patients;
- in the treatment of gingivitis/periodontitis in order to assess the severity of the condition and the effectiveness of the therapy.
Measuring periodontal pocket depth
The purpose of the examination is to assess the level of periodontal damage. The presence and parameters of pockets are visualized. The examination is carried out with a probe, a periodontometer and a calibrating stroker with a special scale.
The number of measurements is determined by the group of elements being studied:
2 measurements are taken - for large chewing units from their palatal, lingual and buccal sides and 1 each from the medial and distal sides, 4 measurements - for incisors, small chewing and canines.
Interpretation of pocket measurements:
- Their depth is no more than 2 mm - normal condition.
- This value reaches 3.5 mm - the form of pathology is mild.
- Reaches 4 mm, there is destruction of interdental septa and bone pathology to a moderate degree.
- Exceeds 5 mm – severe form of periodontitis.
This is interesting: How long can you keep arsenic in your tooth: advice from a dentist
Index PI
PI, or Russell's periodontal index, was proposed in 1956 and is intended to establish the stage of development of gingivitis, but also for periodontitis:
- pocket formation, tooth mobility;
- establishes the severity of bone destruction of the tooth, i.e. its loss.
When calculating the periodontal index PI, the index values are summed up and the quotient is obtained taking into account the examined teeth.
The scoring criteria are as follows:
- no signs of pathology – 0 points – no pathological changes, i.e. its intact state;
- 1 - mild gingivitis (the tooth is preserved almost completely, because the inflammation did not cover the perimeter of the tooth);
- 2 - gingivitis has spread circularly, but the tooth-gum connection is not broken;
- 4 – resorption of the tooth septa has begun (this can only be detected on an x-ray);
- 6 - the gum is inflamed, there is a gum pocket, but the tooth is not loose and is fully functional;
- 7 - resorption of the interdental septum has reached the length of the root;
- 8 - periodontal tissues are destructured and the chewing function of the tooth is not performed (the tooth is loose, may be displaced), resorption exceeds the length of the root, and the formation of an intraosseous pocket is possible.
When determining the PI index, all teeth except 8 are examined.
The periodontal index PI determines the degree of plaque on the enamel and refers to periodontitis indices. There are 4 degrees of plaque - from 0 to 3. Zero degree - there is no plaque, the last, third degree - the plaque is pronounced.
The periodontal index PI is obtained by dividing the scores for all teeth by the number of teeth examined. Based on the results of such an examination, we can talk about the degree of gingival inflammation according to an 8-point system, starting from 1.5 points. The last degree is the most difficult.
Complex periodontal index (CPI)
It is used to assess the condition of the periodontium from the initial stage of the disease to its severe manifestations. Designed to determine the health of various age categories of the population:
- 3-5 years;
- 9—14;
- from 15 years old.
All units in the row and their surrounding tissues are checked. The presence of looseness, bleeding, deposits, and the presence of periodontal pockets are observed.
All tissues are examined instrumentally, visually and by palpation. The number and number of elements to be inspected are determined based on the age of the person being examined. So,
- at the age of 3-5 years, numbers are examined: 55, 75, 51, 65, 85;
- 9-14 years –46, 16, 36, 11, 26;
- over 15 years old – 31, 17/16, 11, 47/46, 26/27, 36/
Based on the obtained material, the periodontal condition is coded by the following designations:
| Encoding | Result |
| There is no pathology. | |
| 1 | There is a raid. |
| 2 | Slight bleeding was noted. |
| 3 | A stone has been discovered. |
| 4 | Pockets identified. |
| 5 | The teeth are mobile. |
When calculating KPI, 2 indicators are determined: individual, average:
- KPI in. = sum of codes / per number of units inspected
- KPI environment . = amount of KPI in. /by the number of teeth examined.
Decoding the KPI for different forms of pathologies looks like this:
- up to 2 – the degree of damage is mild;
- up to 4 – average;
- more than 4 – severe.
CPITN Index
The periodontal index CPITN is always considered a marker of the need for treatment of periodontal diseases. It has been used since 1982 and is recommended by WHO. To identify the indicators of this index, the division of the dentition into 3 sextants is used - frontal and 2 lateral. Not all teeth are examined, but only selective ones. It is necessary to examine the tissues around the numbers - 17, 16, 11, 26, 27, 37, 36, 31, 46 and 47. These units, that is, these 10 teeth, give a complete picture of the condition of both jaws. The most periodontally diseased tooth is taken from each sextant. Bleeding gums, the prevalence of tartar and the severity of periodontal pockets are determined.
Research is carried out with a special probe; each tooth is examined for the presence of these disorders. They are registered and analyzed by codes:
- no signs of disease – 1 point;
- if during the examination blood appeared immediately or after 30 seconds. – this is 2 points;
- the presence of tartar (mineralized deposits) - above and below the gum;
- overhanging filling - they delay the plaque that appears - this is 3 points;
- detection of a gum pocket up to 5 mm deep – 4 points;
- if the depth of the periodontal pocket is up to 6 mm or more - 5 points;
X points – there is not a single tooth in the sextant or only 1 (moreover, 8 molars are not included in this calculation).
Next, the amount for each tooth is divided by 6 and the CPITN indicator by code is obtained:
- 0—no treatment required;
- 1 - correction and control of oral hygiene individually for a given patient;
- 2 - professional cleaning and elimination of the above factors delaying plaque on tooth enamel; familiarization with proper oral hygiene;
- 3 — the need for curettage (removal of plaque);
- 4 - comprehensive periodontal treatment.
Pakhomova
Involves applying Lugol's solution to the teeth being examined. The procedure involves 6 frontal teeth of the lower jaw, all 1st molars, 11 and 21 teeth.
The quality of hygiene is assessed according to the degree of staining:
| Grade | Degree of staining |
| 1 | Lack of color upon application |
| 2 | Staining 1/4 crown |
| 3 | Staining 1/2 crown |
| 4 | Staining 3/4 crowns |
| 5 | Staining the entire surface of the tooth |
The overall score is calculated by summing the scores for each tooth examined and dividing by 12.
Periodontal Hygiene Index
1. Periodontal index of oral hygiene Green-Vermillion (Oral Hygiene Index-Simlified, Green-Vermillion, 1964). Allows you to detect not only plaque, but also tartar. Method of determination. The vestibular surface of teeth 16, 11, 26, 31 and the lingual surface of teeth 46, 36 are stained with an iodine-containing solution. On the corresponding surfaces of the teeth being examined, the plaque index (Debris-index) and the tartar index (Calcuius-index) are determined and expressed in points:
Dental plaque (DI): 0—no plaque; 1 - dental plaque covers no more than 1/3 of the surface of the tooth crown; 2 - dental plaque covers from 1/3 to 2/3 of the tooth surface; 3 - plaque covers > 2/3 of the tooth surface.
Dental calculus (CI) : 0 - no dental calculus detected; 1 - supragingival tartar covers less than 1/3 of the tooth crown; 2 - supragingival tartar covers from 1/3 to 2/3 of the tooth crown or there is subgingival tartar in the form of separate lumps; 3 - supragingival tartar covers 2/3 of the tooth crown and/or subgingival tartar surrounds the cervical part of the tooth.
Evaluation of results. Using OHI-S, the level of oral hygiene is determined according to the following criteria: 0 - 0.6 points - good level of hygiene; 0.7 - 1.6 points - satisfactory; 1.7 - 2.5 points - unsatisfactory; more than 2.6 points - bad.
2. Periodontal plaque index Silness-Loe (PI Silness-Löe, 1964). Characterizes the thickness of dental plaque in the gingival area. No special staining is performed to determine it. Method of determination. After thoroughly drying the surface of the teeth, the tip of the probe is passed into the cervical part of the tooth, slightly touching the gingival groove on the buccal and lingual sides. The results are assessed in points: 0 - plaque near the cervix is not detected by the probe; 1 - plaque is not visually detected, only when the tip of the probe moves; 2 - significant accumulation of dental plaque, determined both visually and during probing; 3 - intensive deposition of dental plaque on the surface of the tooth, gum pocket, gingival margin, food residues are determined
Ramfjord's teeth are examined (16, 21, 24, 36, 41, 44). The sum of the indicators is divided by the number of teeth examined.
Silnes Low
A method for assessing oral hygiene without the application of coloring materials.
The dentist examines the oral cavity using a probe to determine the amount of plaque.
Based on the amount of plaque detected, the appropriate assessment is made:
- 0 – no plaque;
- 1 – thin layer of deposits, invisible without the use of a probe;
- 2 – visually noticeable plaques;
- 3 – plaque covers the crown.
Using the Silnes-Low method, the hygiene index of an individual unit, a group of several teeth or the entire oral cavity is calculated.
Gingivitis Index (IG)
Needed to identify the area of formation and the extent of gingivitis. To do this, elements numbered 32, 16, 12, 36, 24,44 are analyzed from four surfaces.
Grades are given based on the following criteria:
| Grade | Result |
| There is no pathology. | |
| 1 | The shade of the gums and its structure are slightly changed, there is no bleeding. |
| 2 | The color is greatly changed, there is swelling and slight bleeding. |
| 3 | Severe inflammation, bleeding with minor gum injury, swelling. |
Based on the data obtained, the average indicator is derived by dividing the sum of assessments for each unit by the number of items examined.
This is interesting: Definition of black hairy tongue, symptoms, causes and treatment methods
The value of IG is deciphered as follows:
- up to 0.1 – pathology is in the initial stage;
- up to 2 – disease in the middle stage;
- up to 3 – severe form of gingivitis.
CSI
Determining the CSI index allows you to find out the amount of tartar and accumulated plaque in the area where the teeth come into contact with the gums.
The condition of the anterior incisors is analyzed. Each tooth is examined from the lingual, medial and vestibular sides. The examination is carried out using a dental probe.
Each surface is scored by:
- 0 – no deposits;
- 1 – deposits 0.5 mm wide;
- 2 – deposits 1 mm wide;
- 3 – plaque more than 1 mm.
To determine the index, it is necessary to add up the sum of ratings for each examined surface and divide by the number of teeth. The maximum value is considered to be CSI 16.
Simplified Gingival Sulcus Bleeding Index
The technique involves identifying the presence of bleeding only based on the patient’s responses. The manifestation of this symptom cannot be verified by probing or visually.
The patient is asked about the possible appearance of blood in various situations, and based on the answers, a coefficient of the degree of inflammation is set.
Typically, a simplified index is used during treatment to analyze its results. Such an examination provides only a rough estimate of the condition of the gums.
Navi indicator
The method involves examining the anterior incisors from the lips. Before starting the procedure, the patient is required to rinse his mouth with a fuchsin solution. This substance colors soft deposits, allowing you to assess the degree of contamination.
Hygiene rating:
- 0 – no deposits;
- 1 – presence of deposits in the area between the gum and tooth;
- 2 – the presence of a noticeable strip of plaque above the border of the tooth and gum;
- 3 – 1/3 coating;
- 4 – 2/3 coating;
- 5 – the tooth is covered with deposits by more than 2/3.
To give an overall assessment, calculate the arithmetic mean for all examined teeth.
Sulcular bleeding (SBI) according to Muhlemann and Son
SBI - will show the early stages of periodontitis and gingivitis. Externally, the oral mucosa may look healthy, but there may be hidden bleeding. With these pathologies, bleeding is possible even with minor damage.
The dental examination technique is carried out as follows: without pressure, a button probe is passed along a certain gum line and the bleeding reaction is observed.
There are 3 degrees of bleeding severity:
- 0 – bleeding did not appear at all;
- 1 – blood appears only in the second half of a minute;
- 2 – blood appeared immediately or within 30 seconds;
- 3 – blood is visible when brushing teeth and when eating.
Tureski
When calculating the Turesky index, the entire dentition is examined. The procedure involves applying a fuchsin solution, after which the appearance of deposits on the lingual and labial surfaces of the teeth is analyzed.
The score is calculated as follows:
- 0 – no plaque;
- 1 – the appearance of individual deposits in the neck of the tooth;
- 2 – presence of deposits 1 mm thick;
- 3 – deposit of 1 mm but less than 1/3 of the surface;
- 4 – plaque on 2/3 of the tooth;
- 5 – deposits cover from 2/3 to all crowns.
The Turesky Index is calculated by adding the scores for each individual tooth and dividing by the number of teeth examined.
Approximal Plaque Index (API)
The procedure involves applying a dye
The approximal surface is the area of contact of the enamel with the tooth located behind it.
The need to inspect the area presented is due to the fact that it requires careful care, which can be difficult to achieve through routine hygiene procedures.
If the amount of plaque exceeds the permissible level, the patient is prescribed professional cleaning.
The procedure involves applying a dye. After this, it is determined how many teeth the color changes.
The API index rating does not provide a pollution rating. The assessment is the presence of a reaction to the dye or its absence.
To determine the index, it is necessary to divide the number of stained teeth by the number of all teeth in the patient’s oral cavity. The resulting figure is multiplied by 100.
Evaluation of results:
| Grade | Hygiene level |
| Less than 25% | Optimal |
| 26% – 39% | Sufficient |
| 40% – 69% | Moderate |
| 70% – 100% | Unsatisfactory |
Flying Rate by Quigey and Hein
Determining the plaque index involves applying a fuchsin solution to 12 front teeth on both jaws. The survey includes numbers 12, 13, 11, 21, 22, 23, 31, 32, 33, 41, 42, 43.
After applying the solution, the vestibular surface is examined. The plaque index depends on the degree of surface staining.
Results of the procedure:
- 0 – no changes when applying the solution;
- 1 – change in color in the cervical area;
- 2 – color within 1 mm;
- 3 – deposits occupy from 1 mm to 1/3 of the surface;
- 4 – 2/3 plaque;
- 5 – sediments cover more than 2/3.
To calculate the index, the totality of points is summed up, and the resulting number is divided by the number of teeth examined (12).
PHP
Determines the effectiveness of hygiene measures, including the thoroughness of daily cleaning. During the procedure, 6 teeth are examined: 16, 26, 11, 31, 36 and 46. The patient rinses his mouth with a special solution containing a dye.
The rating is based on the presence of a reaction to the solution:
- 0 – no reaction
- 1 – tooth staining
If the indexed tooth is removed, the adjacent tooth is examined.
To calculate the result, the score of all examined teeth is combined, after which it is divided by 6. The code for an individual tooth is the score obtained from the examination of each area (medial, distal, occlusal, central, cervical).
Interpretation:
| Grade | Efficiency of RP hygiene |
| Less than 0.1 | High |
| 0.1 – 0.6 | good |
| 0.7 – 1.6 | Satisfactory |
| More than 1.7 | Unsatisfactory |
Oral Hygiene Performance Index (OHP) Podshadley, Haley, (1968)
Iodine index of enamel remineralization.
The active permeability of iodine in tooth tissue is known. Remineralization index (RI), which characterizes the effectiveness of the remineralization therapy used. It is assessed using a four-point system:
1 point – no staining of the tooth area;
2 points - light yellow coloration of the tooth area;
3 points - light brown or yellow staining of the tooth area;
4 points - dark brown staining of the tooth area.
The calculation is carried out according to the formula:
IR = IRNP x number of teeth with hypersensitivity / n,
where IR is the remineralization index;
RRI—remineralization index of one non-carious lesion;
n is the number of teeth being examined.
Dark brown and light brown staining indicates demineralization of the tooth area with non-carious lesions; light yellow - indicates a certain level of remineralization processes in this area of the tooth, and the absence of staining or its slightly yellow color demonstrates a good level of the remineralization process of a particular non-carious tooth lesion.
Composite Periodontal Index (CPI)
It is used for a comprehensive assessment of the condition of the gums and periodontal canal. The procedure involves performing a standard dental examination using a probe and mirror.
During the examination, the dentist notes the presence of certain symptoms, each of which corresponds to a specific score reflecting the condition of the tissues.
Criteria for evaluation:
- 0 – absence of pathological signs;
- 1 – soft deposits;
- 2 – bleeding;
- 3 – tartar;
- 4 – expansion of the periodontal canal;
- 5 – loosening of the tooth in the affected area.
The KPI index is determined by dividing the sum of indicators by the number of examined teeth. The method of examination depends on the age of the patient.
Interpretation of the CRPD:
- From 0.1 to 1 – potential risk of developing periodontitis;
- From 1.1 to 2 – mild form of periodontitis;
- From 2.1 to 3.5 – moderate severity;
- From 3.6 and above – severe form.
Ramfiord index (dental plaque)
The SP Ramford index (1957) has 2 criteria: the degree of inflamed gums and the depth of periodontal pockets. This is an indicator of periodontal disease. Unlike PI, it not only determines the depth of the pocket from the apex of the papillary triangle, but also takes into account the height of the root exposure due to gum retraction (expansion of the gingival groove with exposure of the neck and part of the root of the tooth).
The distance is measured from the enamel-cementum border to the apex of the papillary triangle. With atrophied gums, these 2 indicators are added; with hypertrophy, the difference between them is taken. The periodontium is examined on 2 surfaces - lingual and vestibular - for the amount of plaque contaminating the enamel, as well as for dental subgingival calculus.
For gingivitis, the indicators will be:
- 0 – no disease;
- 1 – locally the gum is slightly inflamed;
- 2 – noticeable inflammation of a large area of the gum;
- 3 – severe gingivitis.
This is interesting: MTA Pro Root paste (ProRut): composition and instructions for use
Periodontitis data:
- pocket of acceptable sizes – 0–3;
- 4 – pocket depth 3 mm;
- 5 – depth 6 mm;
- 6 – depth greater than 6 mm.
The sum of the scores obtained is divided by the number of dental units examined.
This index is important for those people who cannot or cannot have an x-ray. In the elderly, it is not practical to identify this index, since there are age-related changes in the periodontium: gum retraction, involution of bone tissue.
Papillary bleeding (PBI) according to Saxer and Miihiemann
The periodontal bpe index (PBI) is needed to determine the degree of gum inflammation. A probe is used to make a groove along the interdental papillae and observe for 30 seconds.
The severity of gingivitis is 4 points:
- 0 – no blood;
- 1 – appearance of only blood spots;
- 2 – pinpoint blood appearances along the line of the furrow;
- 3 – blood fills the triangle between the teeth.
- 4 – intense bleeding.
The study of the papillae - PapillaBleeding - is carried out in the following quadrants: the gums of the 1st and 3rd quadrants from the lingual surface and the 2nd and 4th quadrants - from the vestibular side (the vestibular side is the vertical wall of the tooth from the lips and cheeks). First, each quadrant is counted, then the arithmetic mean is derived.
Gum recession index
It is determined what part of the teeth (%) has an important symptom of periodontal pathology - apical displacement of the periodontal attachment, which clinically looks like exposure of the boundary between the enamel and cementum of the tooth and exposure of the root. Gum recession index = (r/n)*100%,
where r is the number of teeth with gum recession; n is the number of teeth examined.
Gingival attachment loss index
The index is used along with the CPI for epidemiological surveys. The objective of this study is to evaluate the periodontal condition during gingival recession. Using a periodontal button probe, the distance from the enamel-cementum border of the tooth to the periodontal attachment (i.e. to the bottom of the pocket) is measured. Index codes: 0 - the enamel-cementum junction is not visible, the periodontal probe is immersed only to the beginning of the black mark (normal groove depth) or within the black mark (pocket depth no more than 6 mm). Calculation of the distance from the invisible enamel-cementum border to the bottom of the pocket: the pocket depth is less than 6 mm, including 2 mm at the edge of the free gum located above the dentogingival junction - therefore, the distance from the bottom of the pocket to the enamel-cementum border does not exceed 4 mm . 1 - a) the enamel-cement border is not visible, the entire black mark of the probe is immersed; b) the enamel-cement border is visible, from it to the bottom of the pocket 4-5 mm. 2 - the enamel-cement border is visible and, upon probing, is located at the level between the upper border of the black mark and the first ring of the probe - the displacement of the attachment is 6-8 mm; 3 - the visible enamel-cement border is located between the first and second rings of the probe - the displacement is 9-11 mm; 4 - the visible enamel-cement border is located above the second ring of the probe - the displacement is more than 12 mm. The selection of key teeth and sextant evaluation and analysis follow the same rules as when working with CPI.
PFRI
The indicator reflects the rate of plaque formation. Allows you to evaluate the conditions and factors that influence the formation of soft deposits. The diagnostic value of the method lies in the fact that it allows you to assess the risk of caries.
The rate of plaque formation is influenced by the following factors:
- Bacterial composition of the oral microflora;
- Total number of bacteria;
- Composition of salivary fluid and its quantity;
- Condition of enamel, gums, fillings;
- Quality of denture care.
Before assessing the rate of plaque formation, professional cleaning is performed.
The diagnostic procedure is performed 24 hours after cleaning. To do this, a coloring solution is applied.
The following surfaces are examined:
- Buccal;
- Lingual;
- Mesio-buccal;
- Mesio-lingual;
- Distobuccal;
- Distal-lingual.
The appearance of color is assessed as 1 point, while the absence of reaction to the solution is 0 points.
To calculate the PFRI, the total score should be divided by the number of teeth and multiplied by 100. The PFRI results are expressed as a percentage.
Ratings:
- From 0 to 10% – very low;
- From 10% to 20% – low;
- From 21% to 30% – average;
- From 31% to 40% – high;
- Over 40% is very high.
Php Index
Scientists Podszadlej and Haley developed an oral hygiene performance index. First, a dye solution is applied to the teeth, then the patient rinses his mouth with water, and 6 teeth are examined. In this case, their surface is divided into 5 sections: medial, distal, mid-occlusal, central, mid-cervical. The absence of staining is determined by zero, and the presence - by one.
When calculating, use the formula: IG = ZN/n, where ZN is the sum of codes for all teeth; n – number of teeth examined. With a value of 0, the condition of the oral cavity is considered excellent, and with a value of 1.7 or more, it is considered unsatisfactory.
Green-Vermillion index
The use of coloring agents is not required. The surfaces of teeth 16, 26, 11, 31, 36 and 46 are analyzed.
When there is no dental plaque, you can give zero points, if a third of the tooth surface is affected - one, up to two thirds - two, the rest - three points. Stone deposits are assessed similarly.
Green-Vermillion index
CPITN (periodontal disease treatment need index)
This method covers 10 teeth, allowing the dentist to see the condition of the gums of the upper and lower jaws. Grades are given as follows:
- 0 – no disease symptoms;
- 1 – gums are bleeding;
- 2 – tartar was found above and below the gum;
- 3 – gum pocket 4-5 mm deep;
- 4 – gum pocket more than 6 mm.
It may come as a surprise to many that the condition of teeth can be determined using a formula, but this is the truth. Therefore, do not neglect maintaining oral hygiene, so as not to be a poor student in this calculation.
The iOrtho clinic network provides high-quality services for correcting malocclusion with Invisalign aligners, sign up for a consultation now!
Index of need for periodontal disease treatment - CPITN
To assess the prevalence and intensity of periodontal diseases, almost all countries use the index of need for the treatment of periodontal diseases - CPITN . This index was proposed by specialists of the WHO working group to assess the condition of periodontal tissues during epidemiological surveys of the population.
Currently, the scope of the index has expanded, and it is used to plan and evaluate the effectiveness of prevention programs, as well as calculate the required number of dental personnel. In addition, the CPITN index is currently used in clinical practice to examine and monitor the periodontal condition of individual patients.
In this regard, the CPITN index can be considered a screening test at both the population and individual levels.
This index registers only those clinical signs that may undergo reverse development: inflammatory changes in the gums, which are judged by bleeding, tartar. The index does not record irreversible changes (gingival recession, tooth mobility, loss of epithelial attachment), does not indicate the activity of the process and cannot be used to plan specific clinical treatment in patients with developed periodontitis.
The main advantages of the CPITN index are the simplicity and speed of its determination, information content and the ability to compare results.
To determine the CPITN index, the dentition is conventionally divided into 6 parts (sextants), including the following teeth: 17/16, 11, 26/27, 36/37, 31, 46/47.
The periodontium is examined in each sextant, and for epidemiological purposes only in the area of the so-called “index” teeth. When using the index for clinical practice, the periodontium is examined in the area of all teeth and the most severe lesion is identified.
It should be remembered that a sextant is examined if it contains two or more teeth that cannot be removed. If only one tooth remains in the sextant, it is included in the adjacent sextant, and this sextant is excluded from the examination.
In the adult population, starting from 20 years of age and older, 10 index teeth are examined, which are identified as the most informative:
When examining each pair of molars, only one code characterizing the worst condition is taken into account and recorded.
For persons under 20 years of age, 6 index teeth are examined during the epidemiological survey: 16, 11, 26, 36, 31, 46.
CODE 1: bleeding observed during or after probing.
Note: bleeding may appear immediately or after 10-30 seconds. after probing.
CODE 2: tartar or other plaque-retaining factors (overhanging edges of fillings, etc.) are visible or felt during probing.
CODE 3: pathological pocket 4 or 5 mm (the edge of the gum is in the black area of the probe or the 3.5 mm mark is hidden).
CODE 4: pathological pocket 6 mm deep or more (with the 5.5 mm mark or black area of the probe hidden in the pocket).
CODE X: When only one or no teeth are present in the sextant (third molars are excluded unless they are in place of second molars).
To determine the need for periodontal disease treatment, population groups or individual patients can be categorized based on the following criteria.
0: CODE 0 (healthy) or X (excluded) for all 6 sextants means that there is no need for treatment for this patient.
1: A CODE of 1 or higher indicates that this patient needs to improve his oral hygiene status.
2: a) CODE 2 or higher indicates the need for professional hygiene and the elimination of factors that contribute to plaque retention. In addition, the patient needs training in oral hygiene.
b) CODE 3 indicates the need for oral hygiene and curettage, which usually reduces inflammation and reduces pocket depth to values equal to or less than 3 mm.
3: Sextant with CODE 4 can sometimes be successfully treated with deep curettage and adequate oral hygiene. In other cases, this treatment does not help, and then complex treatment is required, which includes deep curettage.
The prevalence and intensity of periodontal disease in the population is assessed based on the results of a survey of 15-year-old adolescents.
Prevalence of signs of periodontal damage (adolescents 15 years old)
Prevalence Bleeding gums Tartar
low 0 – 50% 0 – 20%
average 51 – 80% 21 – 50%
high 81 – 100% 51 – 100%
Level of intensity of signs of periodontal damage (adolescents 15 years old)
INTENSITY LEVEL BLEEDING GUMS CALCULUS
LOW 0.0 - 0.5 sextants 0.0 - 1.5 sextants
AVERAGE 0.6 - 1.5 sextants 1.6 - 2.5 sextants
HIGH < 1.6 sextants < 2.6 sextants
Arnim index
Allows you to evaluate the effectiveness of hygienic procedures carried out in the oral cavity, to identify plaque lesions on the surfaces of the incisors from the lips. They are dyed with erythrosine. The specified area is captured in a photograph and then developed at four times magnification. Dental contours and identified pathological formations are applied on paper and planimers are used.
Arnim index
Navi Index
The surface of the teeth is assessed from the side of the teeth. Before assessment, you need to rinse your mouth with 0.75% fuchsin.
Magenta
They think like this:
- 0 is set if there are no pathological deposits;
- 1 is placed when plaque deposits are painted only at the gum border;
- 2 is given if the plaque is noticeable at the gum line;
- 3 is set when a third of the tooth is occupied by deposits;
- 4 is given if two-thirds of the tooth is affected;
- 5 is given when more than two-thirds are affected.
Navi Index
Important! The resulting numerical value should be considered a conversion to the average number of one tooth of a particular person.
Ramfjord index
The Ramfjord index is part of the periodontal index. It is designed to detect plaque on the vestibular, lingual and palatal surfaces, proximal surfaces of 11, 14, 26, 31, 34, 46 teeth. The enamel is painted with Bismarck brown solution and points are given.
Ramfjord index
The required number is obtained by dividing all points by how many teeth were examined.
Advantages and disadvantages
An important component of implantation at all stages is an accurate index assessment of the condition of peri-implant tissues, implants and supported prostheses. The Schiller-Pisarev test is quite effective and allows you to diagnose a wide range of conditions - gum inflammation, periodontal destruction, the amount of tartar, plaque, the need for certain therapeutic measures and their volume.
The relationship between the elements of the implant and adjacent tissues and its difference from a natural tooth may make complex periodontal studies impossible.
The Schiller-Pisarev test is quite accurate and objective and has two interpretation options. The first is visual, based on the nature of the gum staining, the second is numerical, that is, index. The main problem of the technique is that dental indices from 30-50 years ago do not meet the current needs of modern implantology.
That is, they can be used, but when interpreting the results, it will be necessary to take into account the full list of current changes and improvements in the field of prosthetics. At the same time, it is the Schiller-Pisarev test that is considered the most informative of all similar diagnostic methods and allows the results to be most successfully adapted to the conditions of endosseous implantation. However, the convention of numerical values still does not disappear anywhere, since diagnostics are carried out using markers, and not high-precision digital equipment. Modern researchers say that the Schiller-Miller test is still relevant, but should be used with certain modifications and clarifications.
conclusions
The listed periodontal indices contain information about the hygienic situation in the oral cavity, the intensity of the spread of inflammation and the destructive process in the periodontium.
The examinations are simple to perform, do not cause pain to the person, and do not require the doctor to undergo special training.
They help to assess the general condition of periodontal tissues and formulate conclusions about the effectiveness of therapeutic and preventive measures.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags gums periodontal indices
Did you like the article? stay tuned
KPU index assessment
To determine the degree of infection, dentists use three basic indicators.
In the case of assessing the prevalence of caries, a percentage value is used. The calculation method involves dividing the number of patients in whom pathology was detected by the total number of those who underwent examination, after which the result is multiplied by one hundred. When comparing regional indicators, data obtained during examinations of adolescents aged twelve years are used - a value not exceeding 30% is considered low.
The intensity of infection is calculated based on the number of elements affected by caries, and provides for the presence of five degrees. In the case of younger patients, the coefficient varies from 1.1 to 6.5, while for adults the range of values is 1.5-16.3.
To assess growth, periodic surveys are prescribed, during which the difference between the current and previous indicators is determined. The diagnostic results not only reflect the level of oral health, but also allow you to create a treatment plan that takes into account the specifics of each patient’s body.
Characteristic disadvantages
Among the disadvantages characteristic of the method under consideration are:
- Inclusion of both cured and extracted elements in the indicators;
- The influence on the overall picture of previous dynamics, characterized by an increase in intensity as they grow older;
- Ignoring the early stages of development of carious diseases.
Such shortcomings, in fact, limit the possibility of forming a detailed picture characterizing the state of oral health. Over time, new areas of caries localization, deformation and loss of fillings, as well as other processes are observed in the dentition. The specified data is summed up again during the next inspection, which leads to a distortion of the final results and general statistics.
Papillary bleeding (PBI) according to Saxer and Miihiemann
The periodontal bpe index (PBI) is needed to determine the degree of gum inflammation. A probe is used to make a groove along the interdental papillae and observe for 30 seconds.
The severity of gingivitis is 4 points:
- 0 – no blood;
- 1 – appearance of only blood spots;
- 2 – pinpoint blood appearances along the line of the furrow;
- 3 – blood fills the triangle between the teeth.
- 4 – intense bleeding.
The study of the papillae - PapillaBleeding - is carried out in the following quadrants: the gums of the 1st and 3rd quadrants from the lingual surface and the 2nd and 4th quadrants - from the vestibular side (the vestibular side is the vertical wall of the tooth from the lips and cheeks). First, each quadrant is counted, then the arithmetic mean is derived.
How is the procedure performed?
The essence of the Schiller-Pisarev test is to lubricate the gums with a solution of iodine and potassium. As a result, areas with deep connective tissue lesions become stained - this is due to the accumulation of large volumes of glycogen in areas of inflammation. The tests are repeated from time to time - if the treatment is carried out correctly, the condition of the gums will improve, and the inflammation will subside or disappear altogether. That is, if the therapy is correct, then repeated tests should be weakly positive or negative.
Gum staining is due to the high amount of glycogen. When the inflammation passes, there is less glycogen, and the tissues cease to be intensely stained. In this way, the intensity and degree of development of the disease is determined.
Composition of the solution
To take Schiller-Pisarev samples, the composition of the solution is used in the following proportions:
- crystalline iodine – 1.0;
- potassium iodide – 2.0;
- distilled water – 40.0.
Before using therapeutic and prophylactic toothpaste (Parodontax, Parodontol paste), the gum mucosa is lubricated with a special solution, then the degree of staining is determined, and the data obtained is recorded in the disease history. Control – after 1, 2, 3, 6 and 12 months.
General overview
Periodontal indices are a quantitative (in percentage or coefficients) expression of pathological processes occurring in the periodontium.
In comparison with clinical diagnostic methods, the index assessment is relative and does not claim absolute accuracy.
However, it has a number of advantages that clinical diagnostics lack. With its help it is convenient:
- conduct epidemiological studies for any segment of the population;
- monitor the dynamics of pathological processes;
- compare the results of different studies;
- evaluate the effectiveness of treatment and prevention.
Hygiene efficiency index
The evaluation requires the use of dyes. Examine the surface from the cheeks 16 and 26, lips 11 and 31, tongue 36 and 46 teeth.
Hygiene efficiency index
Important! At zero, the composition does not paint the parts being examined. When unity, coloring of a different nature is noticeable.
PDI index
The PDI index characterizes the health of the gums and periodontium. The vestibular and oral surfaces of the 16th, 21st, 24th, 36th, 41st, and 44th teeth are analyzed.
- "Candide" solution for the oral cavity: instructions
PDI index