In what cases may the bone fail to take root?
The bone may not take root in cases where it becomes infected, including when the patient violated the schedule for taking antibiotics or did not follow the doctor’s orders.
Much attention is paid to food intake: the patient can simply, out of forgetfulness, bite into something hard, and his stitches will come apart, and the material and bone graft will become infected through the open wound.
The above accounts for 90 percent of cases
when the bone may not take root.
Are there any contraindications to bone grafting?
Of course, there are contraindications to bone grafting. These include
:
- various chronic diseases, incl. diabetes mellitus with high sugar levels,
- the period when the patient takes a number of drugs, including chemotherapy,
- in the period after chemotherapy, when the bone cannot be “touched” at all.
Features of hygiene after bone grafting
After bone grafting it is recommended
:
- use of special surgical toothbrushes,
- the use of toothpaste should be limited, and even better, use special toothpastes for post-surgical interventions,
The main thing when carrying out hygiene is NOT TO INJURY
area of bone grafting! You should try to eliminate contact with this area or reduce it to a minimum.
Webinars on using EthOss from world clinicians
REGISTRATION CERTIFICATE
Bone grafting is one of the most popular operations in maxillofacial surgery and dentistry. It is needed to prepare the patient for the installation of a dental implant. Due to various dental pathologies or prolonged absence of teeth, bones undergo atrophic processes and become thin. Since the bone must be sufficiently dense for the implant to be installed and survive well, bone grafting will help correct the bone deficiency.
Biological bone materials are usually created in two ways - either from the bone tissue of cattle, or from cadaveric biomaterials, that is, from the bones of deceased people. Yes, this is allowed in most countries, but you must admit that in the 21st century, using such a technique no longer seems like a completely modern way to restore a smile, and besides, there is a high risk of getting an allergic reaction, or the patient’s personal intolerance to these materials, as well as cross-infection of the bone.
Therefore, technology has not stood still for a long time, and British clinicians have found a way out of this situation and created a completely safe synthetic bone material that causes natural regeneration of human bones, consisting of calcium beta-triphosphate and calcium sulfate. This development is called - bone material EthOss (Ethos)
EthOss is a bone material developed by implantologists for implantologists. It consists of absolutely biocompatible materials that stimulate bone regeneration processes. Contains no animal or human ingredients.
The use of this material has achieved clinical success among a huge number of specialists, since EthOss eliminates the need for donor grafts and artificial scaffolds. The built-in barrier eliminates the need for additional membranes and speeds up the surgical process. This results in a faster operation with a minimally low pain threshold for the patient.
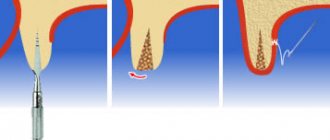
How is implantation performed during bone grafting?
Implantation during bone grafting can be carried out either simultaneously with bone grafting, or delayed - when the implants are installed in the new “grown” bone.
As an experienced implant surgeon, in my practice, in 80-90 percent of cases I perform bone grafting at the same time
with implantation.
I will explain why I perform plastic surgery with implantation at the same time, and what is the advantage of this approach. Bone grafting itself requires a long healing period, from 4 to 9 months. And if we maintain this period and then do implantation, then we have to wait another 4 months. That is, the time frame in this case increases significantly.
And if I do implantation along with bone grafting, then the implant takes root along with the bone. A good implant has an excellent osteogenerating surface, and when fused, an excellent result
.
This reduces the patient’s rehabilitation time. And most importantly, the patient DOES NOT NEED
second surgery. We understand that a large number of surgical interventions do not improve trophism, mucous membranes, or bone tissue.
Everything we do at the German Implant Center, from tooth extraction to implantation, is carried out as atraumatically as possible for the patient.
How many implants are placed during a total restoration?
We specialize very broadly in total implant rehabilitation. In the upper jaw, 6-8 implants are recommended according to our protocol; in the lower jaw, 6 implants are sufficient for total rehabilitation.
Often, implantation occurs simultaneously with the installation of temporary teeth, that is, the patient leaves the clinic “with teeth”, and not on the second or third day, but on the same day when implantation is done:
Preliminary implantation planning is carried out using CBCT, the implants are placed in the required positions.
After this, a surgical template is made, according to which the implants are installed. And based on the same computed tomography (CBCT) and images, a temporary structure is made that will be attached to the implants installed for the patient.
And it turns out the so-called “full case” is when the patient comes, if necessary, if circumstances require it, teeth are removed (or they have already been removed/lost earlier), implants are placed on the patient and an orthopedic structure is fixed - his new teeth.
Who invented the bone material EthOss?
This composition of bone material was invented by two clinicians - Dr. Peter Fairbairn and Dr. Paul Harrison.
Dr. Peter Fairbairn, Professor at the University of Detroit School of Dentistry (Michigan, USA), Director of Education of the Association of Dental Implantology (UK), one of the Presidents of the London Dental Association, and Dr. Paul Harrison (member of PHD, MBA, BSC). He is also a global expert in dental product design.
Following an academic career at the University of Leeds, Dr Paul Harrison founded an independent advanced materials invention consultancy. One successful project involved the development of a bone stretching technique using external fixators to strengthen the union after a fracture. Thanks to this, Paul became interested in the subject of bone regeneration.
From the very beginning, EthOss was designed with dentists in mind. True bone regeneration is more than using bone materials to create volume and an artificial frame. The use of EthOss has been proven to promote faster growth of native bone with little pain. Since 2015, its popularity among dentists and patients has been growing very quickly, which was also facilitated by the British Online Academy. EthOss was conceived and developed by clinicians in the UK and is available worldwide.
On which jaw does tooth bone resorption occur faster?
How quickly does a deficiency of bone and bone tissue occur in the absence of a tooth?
In fact, tooth bone tissue decreases faster in the upper jaw, since the upper jaw is softer and more porous. In the lower jaw, the bone also disappears quite quickly, since the vestibular plate near the teeth is quite thin. Six months after tooth loss, quite severe atrophy of bone tissue occurs, and the atrophy progresses. And therefore, in order to avoid atrophy, it is advisable to do implantation simultaneously immediately after tooth extraction.
This format is the regular, daily work of the specialists of the German Implantology Center. For example, a patient comes with a crack in the root of a tooth - the tooth must be removed. We can go with two options:
Option 1.
We can remove the tooth and 3 months later implant the tooth into the patient.
But during these three months, shrinkage of the bone tissue still occurs, since - I said earlier - the vestibular bone plate is very thin. And in this case, the patient undergoes 2 surgical interventions
: the first is tooth extraction, the second surgical intervention is the installation of a dental implant.
Option 2.
In our practice, we recommend and practice the second option. This is a one-step implantation, when the patient has a tooth removed, an implant is installed, and in order to avoid collapse of the bone tissue in the places where the roots of the tooth used to be, these places are filled with a bone graft. Due to graft filling, we do not have tissue “collapse”; the contour of both the gums and the jaw bone tissue is preserved. Which, in turn, is very difficult to achieve with delayed, delayed implantation.
Who can undergo bone grafting?
Who are potential patients for bone grafting, and what are the age restrictions for it?
This is a bit of a tricky question :). The oldest patient I have performed bone grafting on is a 75-year-old patient, a wonderful, purposeful woman. She had bilateral terminal defects on her lower jaw. She really wanted implantation and refused a removable structure.
I performed bone grafting on this woman at the same time as implantation. And literally 6 months later she was fitted with prosthetics. And everything went great.
In the case of the patient’s age, the main thing is that he has no contraindications. Perhaps there are age restrictions, but they are not so pronounced, because, although trophism deteriorates with age, regenerative abilities decrease, but the main thing is the presence of contraindications. You need to look at the tests, and if the patient is healthy at 75 years old, then why not?
Materials for alloimplantation
Today, there are a sufficient number of different types of materials that have proven themselves in orthopedic and implant dentistry. Below is a small list of products for alloimplantation:
- The product of the American company AlloSource, called ADLB, is demineralized lyophilized cortical allobone and has an osteoinductive effect. The time to fill the bone defect is 6-12 months.
- The product of the American company CeraMed, called Allograft, represents demineralized allograft in the form of small particles and has an osteoinductive effect. The time to fill the bone defect is 6-12 months.
- The product of the American company AlloSource, called AlloGro, represents demineralized allobone in the form of bone chips with proven osteoinductivity. Used to fill bone defects, bone callus forms 10-14 days from the moment of implantation.
- The product of the American company Synthes, called DBX, is a demineralized bone matrix that has an osteoinductive and osteoconductive effect for 6 months.
- The product of the American company GenSci Regeneration Sciences, called DynaGraft, is a demineralized bone matrix with the possibility of an osteoinductive effect. Used to fill bone defects with achieving the desired effect within 6-12 months.
- The product of the American company Osteotech, called Grafton DMB, is a demineralized bone matrix with an osteoinductive effect and achieving the desired effect within six months.
- The product of the American company Pacific Coast Tissue Bank, called Lambon, is a demineralized lyophilized allogeneic implant manufactured in the form of a plate. It has an osteoinductive effect, the delimiting function lasts for 4-5 months, and the full implantation effect is achieved after 6-8 months.
- Product of the Russian company Kostny Bank CITO im. Priorov called Perfrost. It is a demineralized lyophilized cortical allobone and has an osteoinductive effect. The time for filling bone defects ranges from 15 to 90 days.
Bone augmentation of the lower jaw
The operation also has its own specifics, since in this projection there is a large accumulation of nerves, the mandibular canal, the temporomandibular joint, etc. It is important to place the bone carefully, without touching or crushing the nerve endings.
The lower jaw is characterized by the transplantation of a donor composition, which is taken from the area of the wisdom teeth or the chin. The donor block is fixed with metal screws, and the gaps are filled with bone chips. After a few months, once the block has taken root, the screws are removed and you can proceed to the implantation procedure.
The most common question is: is it possible to do without replenishing bone volume? Yes, in some cases it is possible. For example, with express implantation, when a root-shaped implant is implanted immediately after the extraction of its tooth. In almost all other cases, even if a month has passed since the tooth was removed, it is impossible to do without bone tissue augmentation. But this operation guarantees a stable position of the implant - reliability, durability and an ideal result of implantation and prosthetics.
Types, sources of origin and composition
In general terms, all existing barrier membranes can be divided into two groups: resorbable and non-resorbable. There are also membranes with a very long period of resorption and, it seems, they are trying to separate them into a separate class, but in my opinion, they should be classified as resorbable, because in the end they still dissolve and disappear. Non-resorbable membranes are made from various bioinert materials (Teflon, PTFE, titanium alloys, etc.), they are used much less frequently, we will talk about them when we consider osteoplasty using the NCR method.
Here and further, we will talk about the most common resorbable barrier membranes in surgical practice.
The main component of barrier membranes existing on the market is collagen, an organic substance of protein nature, the main structural element of connective tissue. The source of collagen for barrier membranes is 98% best friends and, at the same time, human food - pigs. Occasionally, allocollagen (of human origin) or something else (biopolymers, polysaccharide derivatives, etc.) is used.
The main reason for using collagen to produce barrier membranes is its predictable breakdown naturally by collagenase enzymes and the formation of amino acids common to the body. Without unnecessary breakdown products and other LSD.
Anyway. We, the end consumers of barrier membranes, are concerned not so much with production secrets, but with a number of criteria that are important for practice. They are generally similar to what we expect from osteografts and biomaterials in general, and include:
Form factor.
sizes, packaging, etc. The same barrier membrane can be of different sizes. Thus, the Geistlich Bio-Gide we use is available in sizes 16x22, 25x25 and 30x40 mm
And we choose the right size, depending on the scale of the surgical intervention.
Physical and biological properties.
By analogy with osteografts, barrier membranes must have a number of physical and biological properties. Of course, information about the properties is important, first of all, for the doctor, and not for the patient. However, you, friends, also need an idea of the properties to understand how we, doctors, navigate when choosing a barrier membrane to solve a particular clinical problem.
hydrophilicity - well, this goes without saying, because liquid is the main transport medium of the body.
strength – the ability of a barrier membrane to maintain integrity under load and fixation. It should not turn into rags, if we decide to pin it or screw it in, the underlying graft should not erupt, and the stretched membrane should not creep.
elasticity - the barrier membrane must take the shape of the area to which we adapt it. Without unnecessary creases and filing.
adhesion – an ideal barrier membrane literally sticks to the underlying graft and, most often, does not require any special fixation.
We can talk about the properties of barrier membranes for a very long time. And we will do this one day, in an experiment called “M.P.” You, friends, need two things about properties:
– physical properties determine how the barrier membrane behaves during surgery. Does it make the doctor’s work easier and cheaper, or, conversely, complicates it and requires the use of something additional. Pins and screws, for example.
– biological properties determine what happens to the barrier membrane after surgery. They are difficult to measure and practically impossible to study objectively. Therefore, by appealing to biological properties, you can “sell” anything you want. That is why such criteria as “permeability” and “resorption time” are still the subject of fierce disputes, discussions, fights and other quarrels in the professional dental community. And that is why I urge you to believe them as little as possible.
And we just have to consider one more category of biomaterials:
Instead of a prologue. What are biomaterials?
From the point of view of the explanatory dictionary, biomaterials mean any foreign substances and objects introduced into the body and complemented by it structurally and/or functionally, and used for medical purposes . That is, biomaterials can be called artificial heart valves, endoprostheses, implants, including dental ones, metal structures used in osteosynthesis, hemostatic agents, dentures, crowns, inlays, fillings, etc. And vice versa, earrings for piercing, Tattoo inks and all sorts of scary things for body modding do not belong to biomaterials, in their correct understanding.
What we use for “bone tissue augmentation” would be more accurately called “biomaterials for regenerative surgery,” which specifies and explains their purpose. In general terms, the modern dental market offers us three categories of such materials - osteografts, barrier membranes and mucografts:
A little later, we will look at each of these categories in detail.
It is quite difficult to talk about indications and contraindications for the use of biomaterials from the patient’s point of view, so their use during certain osteoplastic operations is an issue that relates more to a specific technique than to the material itself. Therefore, we will consider it in articles devoted to certain osteoplasty techniques. That is, soon.
But, in general, dear friends, you need to know the following:
– the use of biomaterials is always a compromise, a necessary measure.
Yes, theoretically and practically, we could do without them. And there are many examples of this:
Let me clarify that the two right pictures show a temporary crown on an installed implant. Biomaterials for osteoplasty were not used in this clinical case.
But in such cases we are faced with a problem - if we need to compensate for the atrophic loss of bone or mucous membrane, then it must be taken somewhere. And often the process of obtaining an autograft (i.e., one’s own fragment of tissue for transplantation) increases the trauma, complexity and duration of surgical intervention. And sometimes it is even a separate surgical operation with all the consequences: the risks of complications increase and the safety of surgical treatment decreases. The desire to avoid all this by replacing the autograft with something “artificial” seems completely logical.
– none of the existing biomaterials improves the quality of regenerating tissues.
This is a microscopic photograph of what happens after osteoplasty using biomaterials.
If we are talking, for example, about “building up bone tissue,” then none of the osteografts used in modern surgical practice makes the bone stronger, stronger, more beautiful, etc. Moreover, what we get as a result of using “artificial bone substitutes” can hardly be called bone in the biological sense - rather, it is a bone callus with the inclusion of particles of biomaterial (as in the microscopic picture above), its properties and structure are very different from normal healthy bone tissue. If we're talking very seriously, the use of grafts “degrades” the quality of the tissue. But we are forced to make this compromise in order to fill their volume and, accordingly, create conditions for normal implantological rehabilitation.
– there are no biomaterials that accelerate tissue regeneration.
I would even say more - little depends on the brand, manufacturer or country of origin of the biomaterial. All grafts and barrier membranes existing in the world work the same way, according to the same biological laws. It is absolutely wrong to say that “this material works better than this one” or “this one is good, but this one is complete crap!” Of course, biomaterials differ from each other in a number of properties, and today we will definitely talk about these properties.
– each category of biomaterials has its own purpose and clearly defined function.
Just like in this picture:
To use biomaterials for other purposes is, at a minimum, to seriously risk the result. For example, we may try using a hemostatic sponge to fill the subantral space during a sinus lift. And perhaps we will even get a good result. But the word “possible” really confuses me personally. In surgery, the use of this word should be kept to a minimum.
– the use of biomaterials must be justified and understandable, first of all, to you.
“We’ll stick it here, we’ll pin it here”... in other words, the use of grafts and barrier membranes is always a great way to inflate the cost of treatment or artificially complicate the upcoming operation. Indeed, installed implants can be counted, their brand and model can be easily determined from control images, but determining the volume of graft de facto used during sinus lifting or the size of the installed barrier membrane (and, in general, the presence of this very membrane) is not so simple. If for some reason you do not understand why the use of biomaterials is necessary in your clinical case, then they are not needed. We will talk about their use in various clinical situations in subsequent articles, when we study each of the existing methods of osteoplasty. Well, after the operation, it makes sense to “check” with the actual consumption of biomaterials - all grafts and barrier membranes used in modern surgery have special stickers indicating their parameters and serial numbers - one sticker remains in the medical record, the second is pasted into the contract, on a control image or a special form that is given to the patient.
Finally, last but not least:
All existing biomaterials are disposable. One package is intended for ONLY one operation:
This, in fact, means that, firstly, unused remnants of biomaterials cannot be re-sterilized and used, and secondly, that the absence of the above sticker indicates that in your treatment, the “left” material or residues of some kind may have been used. - some other operation. I categorically do not recommend saving on this, because it is impossible to properly sterilize already opened material in a regular dental clinic without losing its properties.
In principle, dear friends, knowledge of the above is quite enough to understand whether expensive, generally speaking, biomaterials are needed for bone tissue augmentation specifically in your clinical case. Just in case, I remind you that
if you don’t understand something, then you don’t need it.
Just remember this article >>.
As part of the RegenerationDay by Geistlich seminars, I manage not only to increase my sense of self-importance, but also to talk with doctors from various clinics, cities and regions of our country. And I can’t help but notice a harmful trend - the excessive abuse of biomaterials, the stupid desire to push them where, in principle, they are not needed. Many see them as some kind of panacea, some kind of “magic pill” that can, if not guarantee, then improve the result of any osteoplastic surgery. Alas, this is not true.
A lot of osteoplastic operations are performed in our dental center - more than two hundred since the beginning of the year. At the same time, the consumption of biomaterials is relatively small - they are used in less than half of the cases. Why? To answer this question, you need to at least read this >> or just stop by our clinic for a consultation.))
Expert opinion
Igor Yurievich Malinovsky
Maxillofacial surgeon, implantologist
Experience: more than 11 years
Osteoplastic surgery often precedes dental implantation. Especially in cases where the tooth was removed more than a year ago. Without load, the bone sags, atrophies, and its volume becomes insufficient to install an implant. This is why it is so important to restore teeth immediately after their removal. If there are a large number of missing teeth, the only way to do without osteoplasty may be basal implantation with deeper installation of implants into hard layers of bone tissue.
How to do without bone grafting
Is it possible to do without bone grafting and sinus lift?
Yes, in some cases you can do without bone grafting. But you need to understand that if the patient does not have bone tissue, and we install an implant, the crown will hang over the gum, and something from food will constantly get clogged there. That is, it is aesthetically unsightly, and all the food will be stuffed there, the patient will always have a “pocket of food supplies” from yesterday and the day before yesterday.
Option with a smaller diameter implant
You can place an implant of a smaller diameter, and at the same time we can carry out soft tissue regeneration - replant the mucous membrane (this can be connective tissue from the palate, from the tubercle of the upper jaw). And thus we achieve replenishment of the volume of soft tissues. Due to this, aesthetics are visually improved and hygiene problems are eliminated.
Whenever it is possible to avoid various surgical procedures, but not at the expense of quality, then they should be avoided.
That is, surgery for the sake of surgery - it is not needed
.
Autogenous osteoplastic materials in dentistry
According to the literature, the autoplastic method most often used in dental surgery is the transplantation of bone obtained from another part of the patient’s body. The first autogenous transplant was tested by the surgeon Walter in 1820.
Over the next two centuries, patient-derived material was traditionally considered the " gold standard"
» osteoplasty. This was not least due to the imperfection of technologies for processing foreign osteoplastic materials and the low development of chemical production, limiting access to more advanced options.
Proponents of autogenous grafts point to high osteogenicity (due to the presence of cells), osteoconduction (due to the content of minerals and collagen) and osteoinductive properties (due to non-collagenous bone matrix proteins).
In terms of their structure, autografts can be cortical, spongy and spongy-cortical. It is generally accepted that when using cancellous bone materials, faster and more complete graft revascularization occurs.
This is possible due to the content of pluripotent cells
, which are able to differentiate and proliferate, participating in osteogenesis. In cortical grafts, these processes occur slowly.
A number of researchers believe that spongy-cortical fragments, due to their strong cortical part, have sufficient mechanical properties, and the spongy component helps to increase osteogenic potential.
Most often, the extraoral sites for collecting osteoplastic material are the lower jaw, less often the pelvic bone, the lateral edge of the scapula, or the rib. According to foreign experts, tissue from the pelvic bone and jaw has a high regenerative potential and is less susceptible to resorption.
In any case, additional intervention is necessary only to obtain autogenous osteoplastic material. This means the involvement of anesthesiologists and surgeons, additional risks and costs.
If an intraoral graft is required for osteoplasty, the optimal donor site is the body or ramus of the mandible, the retromolar region, the mental symphysis and the hump of the maxilla.
The biomaterial is collected under local anesthesia, which simplifies the entire treatment process, but additional trauma and risks remain.
It is worth mentioning that one of the main reasons for refusing this type of osteoplasty is patients’ fear of surgery and the natural desire to complete the treatment with minimal blood (literally).
Despite the obvious advantages of autografts (biocompatibility, infectious safety, regenerative potential), they have a significant drawback. The problem lies in graft resorption over time, mainly when using extraoral grafts
.
It is necessary to remember about age aspects and the tolerance of additional surgical intervention in certain categories of patients.
The method is used with caution in the elderly and children, including due to insufficient bone and the risk of damage to growth plates in children.
The need to harvest bone is always associated with an additional risk of infection of the donor site, blood loss, increased duration of the postoperative period, increased need for painkillers, increased medical costs, etc.
The need to overcome these disadvantages of autotransplantation has led to the rapid development of an alternative method, allotransplantation. For the first time in the world, an innovative method of replacing bone defects, in which another person acts as a donor, was used in 1880 under the leadership of William McEwan.
Benefits of demineralized lyophilized bone with proven osteoinductive activity
Among all the materials on the market, one can highlight a product called AlloGro from the largest tissue bank in the United States. This preparation is a demineralized lyophilized bone implant whose osteoinductive activity is determined by testing. The need for this test lies in the fact that the inductive properties of donor tissue are highly pronounced, and conducting a biotest eliminates about 10% of donors for the production of material for implantation. Today, in order to save money, to test for osteoinductive activity, laboratories use cell cultures of the SAOS-2 (osteogenic human sarcoma) type, into which thymidine and donor CMP are placed. As a result, the activity of cell division and the rate of thymidine excretion are determined. These data allow the osteoinductive efficiency to be calculated.
As a result of these clinical studies, the company was able to label the product as “Proven Osteogenic Activity.” One of the risks with allogeneic transplants is transmission of a viral infection such as hepatitis or AIDS. But to date, there have been no recorded cases of infection with any virus, even those infections whose development zone is the dura mater. Today, DLK is the most economical and effective osteogenic material.