Gum cancer is included in the group of malignant neoplasms of the oral cavity along with carcinomas of the tongue, floor, cheeks and palate. Malignant processes in different anatomical structures of the oral cavity proceed differently, the reasons for their development and treatment methods are similar.
- Causes of gum cancer
- Stages
- Symptoms of gum cancer
- Risk group
- Diagnosis of gum cancer
- Treatment for gum cancer
- Prevention
- Forecast
- Possible complications of gum cancer
Causes of gum cancer
Statistics know the annual incidence of oral cancer - almost 9,300 Russians, but the number of patients with gum or tongue cancer is unknown. Processes that are close in localization are not similar in prognosis, for example, in terms of aggressiveness, “two big differences”: gum tumor behind the wisdom tooth and under the rest of the dentition, the common thing is the causes leading to malignant transformation.
Until the 2000s, tumors of the oral cavity were considered to be the property of alcoholics and heavy smokers, and cancer processes in this area were called “marginal.” Alcohol and tobacco abuse of all types - smoking or chewing - are still top of the list of risk factors today.
In the 2000s, the population of young and never-smoking intelligent patients leading a sober and healthy lifestyle increased sharply. It was clear that this cohort did not have a generally accepted root cause of cancer, and it was found - infection with human papillomavirus type 16. Unlike cervical cancer, which is also associated with HPV infection, oral carcinomas are not considered markers of promiscuity; a single encounter with HPV-16 is sufficient to initiate the disease.
Modern risk factors also include background processes in the mucous membrane - leukoplakia and erythroplakia, which are initially benign, but with a great potential for proliferation, which can lead to carcinoma in the distant future.
The third cause of gum cancer is chronic trauma to the mucous membrane from dentures, as well as a sluggish inflammatory process maintained by damaged parts of the tooth that are not removed in a timely manner.
Failure to comply with oral hygiene is also included in the causal list, although modern foreign scientists are skeptical about this factor, suggesting that all people brush their teeth twice a day. As targeted surveys and examinations of dentists show, in our country not all social groups have the same level of hygiene, and for Russians this reason is still relevant.
Unlike tumors of all other areas of the oral cavity, which men suffer from several times more often, gum cancer is not gender specific - both sexes are affected equally. The increase in incidence begins after 40 years of life, with each subsequent decade of life marked by a doubling of the number of cases.
Stages
In most cases, gum cancer is not detected at an early stage, which is typical for all oral tumors. People are not used to looking into their own mouth until there is a good reason for this - pain that occurs when the periosteum is involved in the process.
The height of the gum of an adult is small, however, when staging cancer, the tumor is graded in “steps” of 2 centimeters: less than 2 cm, from 2 cm to 4 cm, and more than 4 cm, because malignant processes of the oral cavity are often non-nodular. , and flat infiltrates and ulcers.
The stages of gum cancer are distributed as follows:
- stage 0 or carcinoma in situ - cancer cells have not penetrated into the deep layers of the mucous membrane, as a rule, the disease is visually manifested by leukoplakia, an oncological diagnosis is established only by microscopy;
- Stage 1 - carcinoma is less than 2 cm and there are no signs of damage anywhere else;
- Stage 2 - the primary lesion is more than 2 cm, but less than 4 cm, grows no more than a centimeter deep, there are no metastases in the lymph nodes;
- Stage 3 involves variability in the size of the primary gum lesion, including more than 4 cm, without metastases or with cancer cells in one lymph node no more than 3 cm in diameter;
- Stage 4 is divided into subgroups:
- 4A - extensive tumor without involvement of lymph nodes, or smaller in size with a large lymph node, but not more than 6 cm;
- 4C - the local condition is not important because there are distant metastases.
4B - cancer growing into the jaw and surrounding tissues without metastases, or a smaller lesion with large or multiple tumor lymph nodes on either side of the neck;
Symptoms
It should be noted that early diagnosis of the disease affects a favorable treatment outcome.
Important first symptoms of gum cancer are bleeding gums and pain.
Then a dense infiltrate forms on the gum or bleeding granulations from the periodontal pocket.
These are signs of the initial stage of the disease.
Subsequently, ulceration of the formations occurs and an ulcer appears on the gum.
As a rule, it is painless, crater-shaped with a dense base, surrounded by a red mucous membrane.
Growing deep into the gums, the ulcer affects the bone tissue. Cancer cells multiply rapidly due to the intensity of metabolic processes in the gums.
There are a number of other symptoms of the disease, including:
- Sudden weight loss;
- Loss of appetite;
- Nausea and vomiting;
- Excessive salivation;
- Hair loss;
- Increased body temperature.
Symptoms of gum cancer
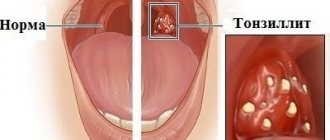
Gum tumors are divided into:
- exophytic - growing outward and forming a node;
- endophytic - spreading deep into the gums, in the form of a flat infiltrate or ulcer;
- mixed - a combination of two growth options; as a rule, this is a far advanced or recurrent process.
I detect a knot on the surface of the gum at an early stage, because it gets in the way, the tongue “feels” for it, and it gets injured when brushing your teeth or while eating. Infiltrates grow faster and are found later, when complaints of pain or bleeding appear.
Cancer in the initial stage does not hurt, especially since the oral mucosa is accustomed to irritating, spicy foods and hot foods. Temporary discomfort while eating does not cause everyone anxiety with a desire to see what is happening there. Gum cancer can masquerade as toothache, forcing you to see a dentist. Most often, it is the dentist who discovers the malignant process.
In stages 3-4, when cancer grows into the jaw, destroying the bone, the pain becomes constant, sharply intensifying while eating, and due to basic malnutrition leading to significant loss of body weight.
A large cancerous ulcer is accompanied by inflammation of the surrounding tissues and decay, causing intense pain radiating to the ear and temple. Secondary infection of the cancerous infiltrate is inevitable; it is manifested by a “heavy” putrid odor. The patient cannot open his mouth due to a painful spasm of the masticatory muscles - trismus. The general condition worsens, the temperature rises, and weakness increases.
Citizens who abuse alcohol drown out the pain by increasing the dose of alcohol, and complain of the appearance of a painful and often inflamed metastatic lymph node under the jaw or on the neck. The presence of various microflora in the mouth complicates metastatic conglomerates in the lymph nodes with secondary infection; when the size is more than 3-4 cm, a zone of decay is formed in the center of the lymph node, often with the formation of a fistula. During this period, symptoms of intoxication with high fever appear.
A reflex increase in salivation with impaired swallowing is characteristic. Salivation is very profuse, so it is possible that saliva may be thrown into the respiratory tract at night with the development of aspiration pneumonia. All malignant tumors lead to increased thrombosis and ease of development of bacterial infection in a weakened body. An additional negative factor is malnutrition up to complete starvation with exhaustion and the development of the fatal anorexia-cachexia syndrome.
Distant metastases are not typical for gingival carcinoma, but recurrences are common after treatment. Cancerous destruction of oral tissues with frequent bleeding from vessels destroyed by the tumor against the background of chronic inflammation in metastatic lymph nodes leads to a serious condition and death.
Symptoms of advanced oral cancer
You may have any of the following symptoms:
- persistent pain in the lips, mouth, or both;
- a lump on the lips, neck, or mouth that does not go away;
- white or red spots on the gums, tongue, or cheeks;
- persistent bleeding, pain, or numbness in the mouth;
- persistent sore throat;
- feeling as if something is stuck in the throat;
- problems chewing or swallowing;
- pain while chewing food or swallowing;
- swelling, which causes dentures to fit poorly or cause discomfort;
- voice change;
- ear pain;
- inability to open mouth.
to come back to the beginning
Risk group
Knowledge of risk factors allows you to calculate a likely “candidate” for the development of oral cancer and timely modify behavior towards a healthy lifestyle, eliminating actions that are hazardous to health.
High-risk group for malignant processes in the gum area:
- People who smoke have celebrated their fortieth birthday, because the frequency of neoplasms increases with age and the “control point”, after which the incidence doubles with each decade of subsequent life, is precisely 40 years.
- Young people with a full range of risk factors. Before the age of 40, carcinomas of this localization are rare, but early introduction to tobacco simultaneously with chewing betel or nas, with persistence in the mucosal cells of the human papillomavirus type 16, significantly increases the chances of cancer.
An extremely high-risk group when the prospect of becoming a cancer patient over time is very high:
- Suffering from precancerous processes - leukoplakia and erythroplakia;
- Older people who smoke, use dentures, and the older they are, the more likely malignant transformation is;
- Adults with a hereditary predisposition, which is identified by the presence in the family of patients with oral carcinomas.
All patients at risk should visit the dentist at least twice a year and undergo treatment for precancerous processes.
What is oral cancer
Regular examination by a doctor - prevention
Oncological diseases of the oral cavity are caused by malignant cell growth in various tissues of this anatomical region. Since almost the entire oral cavity is lined with epithelial tissue, the likelihood of developing cancer is quite high.
This does not mean that anyone is susceptible to this disease. For tumor growth to occur, the influence of negative factors is necessary.
Malignant growth can affect the following parts of the oral cavity:
- Lips.
- Gums.
- Language.
- Buccal mucosa.
- Sky.
- Floor of the mouth.
The most common tumors are the tongue, the inner lining of the cheeks and the floor of the mouth. The clinical picture and the rate of spread of tumor cells depend on the location of the disease. When a tumor grows in the buccal area, the salivary glands may be affected.
Diagnosis of gum cancer
Oncopathology of the oral cavity is visual, that is, diagnosed during a routine examination without the use of any equipment.
During the initial examination, cells are scraped from the wound for cytological analysis, or, in the absence of an ulcer, the tumor is punctured with a thin needle. If possible, a part of the tumor is “bitten off” with a special instrument - this is a biopsy for histological analysis. The diagnosis of cancer is established solely by the result of a biopsy; cytology allows only to suspect the disease.
After morphological confirmation, an ultrasound of the oral cavity is performed, which explains the relationship of the neoplasm with the surrounding tissues, primarily with the bone and blood vessels, and the CT scan clarifies the condition of the entire anatomical region.
Next is the search for metastases: ultrasound of the neck, CT scan of the lungs or MRI.
Anatomical structure
The oral cavity is the initial section of the digestive tract, in which food is chewed and saliva is produced to digest food. It is involved in the process of breathing, swallowing, articulation and speech.
The composition of the oral cavity includes:
- vestibule (lips, front side of teeth, inner surface of cheeks);
- gums;
- the bottom on which the tongue lies;
- two thirds of the tongue;
- teeth;
- retromolar triangle - the space on the lower jaw behind the third molar;
- hard and soft palate.
Treatment for gum cancer
It is optimal to perform the operation at the first stage, if technically possible. The radicality of the surgical intervention ensures a distance of at least 2 centimeters from the tumor border; it is clear that this is possible with a small stage 1 lesion.
At stages 2-3, the possibility of surgery is limited by the depth of penetration of cancer cells deep into the tissues of the jaw; with a large depth of infiltration, the process is considered questionably operable, but a lot is determined by the experience and talent of the oncologist surgeon. Techniques have been developed that make it possible to replace large surgical defects of the jaw with skin flaps, ribs, metal structures or artificial tissues. Plastic surgery may be postponed until antitumor treatment is completed.
If the tumor thickness is more than 4 millimeters, the surgical plan includes removal of the lymph nodes of the neck; if the cancer infiltration is localized in the middle of the oral cavity, the nodes are removed from both sides. Lymphadenectomy has a positive effect on life expectancy, but reduces its quality. It is possible to refuse lymphadenectomy if there are no metastases, which is proven or rejected by a morphological study of a biopsy obtained from a “sentinel” lymph node.
Surgery for cancer above stage 1 is complemented by prophylactic radiation, which should begin one and a half months after surgery.
Initially inoperable stage 3 tumor conglomerates are tried to be reduced by radiation in combination with chemotherapy with platinum derivatives, postponing surgery to the second stage.
Contraindications for surgery: stage 4, proliferation of metastases from the lymph node into the skin or tissue of the neck, severe diseases in the decompensation stage.
If surgery is not possible, 7 weeks of radiation therapy is performed on the primary lesion and lymph nodes of the neck, with the introduction of platinum chemotherapy every 3 weeks. If radiation is contraindicated, chemotherapy is used; this is also done in case of relapse after chemoradiotherapy.
Forecast
An individual prognosis for the course of the disease is based on the size of the neoplasm and the depth of its penetration deep into the jaw, involvement of vessels and nerves in the conglomerate.
The degree of damage to the lymph nodes affects life expectancy; metastases almost halve the likelihood of cure. Much determines the aggressiveness of cancer cells; low differentiation is not in favor of the patient.
Specific percentages by years of survival are unknown because the incidence is low and statistically gum cancer is not distinguished from the group of oral carcinomas.
Briefly about the disease
Oncological tumors of the oral cavity are not rare, and gum cancer is diagnosed in 9% of cases of such diseases.
The disease itself is a malignant tumor of the soft tissues of the jaws.
A malignant process on the gum is dangerous because there are many lymph nodes and capillaries nearby. It is into the lymph nodes that metastases mainly penetrate, in approximately 70% of cases. Their penetration into the brain and other vital organs is insignificant.
Gum cancer most affects men aged 55+. This may be explained by the fact that women seek medical help more often than men. And, besides, men have more bad habits than the fair sex.
Possible complications of gum cancer
First of all, patients are concerned about the cosmetic consequences of treatment; in this regard, chemoradiation treatment is preferable, but is fraught with a higher frequency of relapses and is inferior to surgery in terms of survival.
The list of dangerous complications of carcinoma includes deterioration in nutrition with exhaustion and the development of fatal anorexia-cachexia syndrome. Long-term cancer-preventive therapy worsens nutritional status and worsens underweight. From the first days of treatment, the patient necessarily needs nutritional correction and nutritional support with special protein mixtures. In some periods, the patient may require tube and parenteral nutrition, since swallowing is seriously impaired and spasm of the facial muscles develops, up to the inability to open the mouth due to trismus.
Malnutrition and tooth loss after irradiation worsen the course of concomitant diseases and contribute to the development of infections against the background of a natural decrease in immunity. A change in the swallowing reflex due to too intense production of saliva, literally flowing in a stream, leads to the night-time reflux of saliva with food debris and bacterial flora into the respiratory tract and the occurrence of severe aspiration pneumonia.
Blockage of lymph outflow and proliferation of neck vessels by metastatic lymph nodes is complicated by constant headaches and loss of consciousness.
The disintegration of a cancerous ulcer is fraught with bleeding, which can only be stopped by ligation of the artery. Tumor masses growing into the bones cause intense pain, aggravated by secondary infection. The most severe suffering for the patient's family is caused by the disintegration of a cancerous ulcer with the addition of a secondary infection and a foul odor. It is absolutely impossible to clear a progressive tumor of necrosis on your own; this is a very difficult task even for specialists.
Treatment of such patients is a great oncological art, which is available to the specialists of our clinic. We are ready to help any patient, with or without complications, who has been treated for a long time and is just beginning to fight for life.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Alieva S.B., Alymov Yu.V., Kropotov M.A. etc. /Cancer of the oral mucosa. Oncology. Clinical recommendations // Ed. Davydova M.I.; M.: Publishing group RONC, 2015.
- Gelfand I.M., Romanov I.S., Udintsov D.B. /Tactics for the treatment of localized forms of cancer of the oral mucosa// Tumors of the head and neck; 2016; 6.
- Romanov I.S., Yakovleva L.P. /Issues of treatment of oral cancer// Farmateka; 2013; 8.
- Kurokawa H., Yamashita Y., Takeda S. et al. /Risk factors for late cervical lymph node metastases in patients with stage I or II carcinoma of the tongue// Head Neck; 2002; 24.
- Little M., Schipper M., Feng FY et al. /Reducing xerostomia after chemo-IMRT for head-and-neck cancer: beyond sparing the parotid glands// Int J Radiat Oncol Biol Phys; 2012; 83.
- Midgley AW, Lowe D, Levy AR et al. /Exercise program design considerations for head and neck cancer survivors// Eur Arch Otorhinolaryngol; 2018; 275(1).
Recovery
Throat cancer
During the recovery period, vitamin complexes with microelements are actively used. Vitamins A, B, C and D play an important role in the restoration of damaged tissues.
Physiotherapeutic procedures are used during the period of rehabilitation and regeneration and may include laser therapy, electrical myostimulation, inhalation and electrophoresis of medicinal substances, magnetic therapy, exercise therapy, and ultrasound therapy.