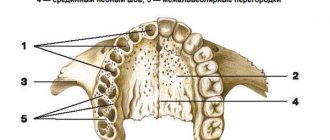
Residual defects of the hard palate after palate surgery are variously shaped openings through which the oral cavity communicates with the nasal cavity after the primary operation to eliminate a congenital cleft palate.
The main signs of residual palate defects:
- reflux of liquid and food from the oral cavity into the nasal cavity during food intake,
- the presence of a hole in the hard palate (round, slit-like, extensive),
- speech impairment and malocclusion.
Introduction
Defects of the palate and oronasal anastomosis are an urgent and pressing problem in reconstructive surgery.
Through defects and anastomosis can be a primary problem, as in the case of congenital clefts, and can also be a consequence of flap necrosis or infectious complications after primary or repeated uranoplasty, as well as resections for benign neoplasms, necrosis and sequestrectomy, post-traumatic injuries of the upper jaw. One way or another, this is a serious functional illness that has physiological, social consequences and can significantly damage the development of a child or young person if observed at a young age.
The variety of surgical techniques used is based on the variability of the shape, size of the defect, the condition of the surrounding tissues and the general somatic condition of the patients. For small defects and intact adjacent tissues, local plastic techniques are often used. But the problem is that with this option of closing the defect, the risk of relapse is quite high. These are complex defects for the surgeon, despite their small size, and are associated with communication between the oral and nasal cavities and/or the maxillary sinus (the presence of a fistula). The aggressive environment of the nasal cavity provokes constantly persistent inflammation and prevents adequate wound healing. Therefore, the choice of surgical tactics should be in favor of well-supplied axial flaps.
FAMM (facial artery musculomucosal) flap - a flap with an axial type of blood supply - was described for the first time. J. Pribaz et al. in 1991, today it is one of the most commonly used flaps for the reconstruction of intraoral defects [1–4].
The FAMM flap is supplied by the facial artery. The facial artery, with an average diameter of 1.5-2 mm, with a blood flow speed of 20-30 mm/s, is a reliable source of blood supply to the flap [5].
The flap includes the buccal mucosa, submucosa, part of the buccal muscle, as well as a rich perforating blood flow from the facial artery, which allows you to cut out a flap in the cheek area up to 8-9 cm long, up to 2.0 cm wide, up to 0.5 cm thick - depending on the size of the defect in the floor of the mouth.
A well-supplied portion of the buccal muscle included in the flap allows for reliable tamponing of the oronasal and/or oroantral anastomosis, which is a good prevention of the development of infectious complications and, as a consequence, necrosis of the flap.
Various modifications of the FAMM flap are described in detail in the literature. To cover defects of the anterior palate, a FAMM flap is used on the superior basis on the proximal part of the facial artery with reverse blood flow. To close defects predominantly in the posterior part of the hard palate, a flap is used on the lower pedicle, the distal fragment of the facial artery with direct blood flow [6].
To eliminate defects of the tongue and floor of the mouth, a modification is used - a transverse FAMM flap [7].
The cheek is an adjacent anatomical site to the palate, and variations in flap design (superior and inferior bases) allow for convenient rotation of the flap into the defect area.
To date, there is no “gold standard” of operations for re-closing palate defects with relapse of oronasal anastomosis. This problem is relevant and requires the development of new algorithms in the selection of donor material and its use in eliminating various defects of the palate.
The purpose of the study is to develop an algorithm for eliminating defects of the palate and alveolar process of the upper jaw using various modifications of the FAMM flap depending on the location and size of the defect.
Possible complications during treatment
Possible complications:
1. The danger of thrombosis is greatest within 20 minutes after restoration of blood flow through the anastomosed vessels. This time should be waited out, observing the pulsation of the stitched arteries.
2. A slow capillary reaction of the tissues of the transplanted flap indicates inadequate blood flow; its cyanosis indicates difficulty in venous outflow.
3. If the anastomosis is performed incorrectly, microvascular thrombosis cannot be prevented in any way, including the use of medications.
4. Vascular sutures, especially on vessels less than 5 mm in diameter, should not be attempted by a surgeon who has not been trained in microsurgery.
Material and methods
In the period from 2016 to 2022, 18 patients aged from 6 to 60 years with a current diagnosis of a defect of the hard palate and/or alveolar process and oronasal anastomosis were operated on in the Department of Reconstructive, Plastic Maxillofacial Surgery of the Federal State Budgetary Institution "Central Research Institute of IIS and Maxillofacial Surgery", Surgical treatment was performed to cover the defect and oronasal anastomosis with a FAMM flap.
Most patients have a history of multiple operations for the underlying disease in the scope of primary uranoplasty, reuranoplasty, the number of previously undergone surgical interventions on the palate in this group of patients ranges from 1 to 8-10, and yet in all cases there was a recurrent residual defect coupled with cicatricial -changed surrounding tissues due to repeated surgical interventions, inflammatory and necrotic processes. The size of the defect from 3 to 40 mm, the need to separate two anatomical zones - the oral and nasal cavity / maxillary sinus, as well as the presence of a persistent inflammatory process in the nasal cavity / maxillary sinus dictated the need to bring in a sufficient amount of well-supplied tissue from another anatomical area.
The psychological and emotional state of these patients makes it a priority to choose a traumatic surgical intervention, without serious donor damage, an optimal surgical intervention in terms of time, with a minimization of the rehabilitation period associated with lower risks in case of failure.
At the first stage of treatment of such patients, the primary task is the reliable and effective elimination of the oronasal anastomosis with a soft tissue flap; in the future, patients are planned to undergo bone reconstruction followed by dentofacial rehabilitation.
In all 18 cases, to plan a flap in the projection of the facial artery, as an instrumental method of research, patients underwent duplex ultrasound scanning of facial vessels with determination of qualitative and quantitative characteristics of the facial arteries, which in 100% of cases helped to determine the localization of the facial artery in a typical place, as well as to register a satisfactory blood flow speed and vessel diameter.
In cases of extensive bilateral defects, CT angiography of the vessels of the face and neck was performed to visualize the bone edges and determine the true size of the defect, which is the most reliable method of preoperative diagnosis and precision flap planning.
Results and discussion
Considering that this method was used in patients with the most complex forms of the disease, requiring the creation of a large wound defect, we did not have the opportunity to form a control group with conventional wound suturing, which would have been technically impossible. The average duration of surgical intervention was 47.6±9.3 minutes. An uncomplicated course of the early postoperative period with wound healing by primary intention was achieved in 38 (92.7%) patients. In 2 patients, limited suppuration of the wound occurred, which required partial spreading of its edges. Another patient had marginal necrosis of one of the “tops” of the diamond-shaped flap, and therefore the wound healed partially by secondary intention. Long-term results were monitored from 15 to 40 months after surgery. Recurrence of the coccygeal tract occurred in 1 (2.4%) patient and was limited (fistulous tract in one of the edges of the wound). The probable cause of relapse was incomplete radical excision of pathologically altered tissue. Repeated surgery in this patient consisted of excision of the recurrent fistula and suturing of the wound; there was no need for plastic surgery. In all other patients, a strong elastic scar was formed at the lowest “critical point” of the postoperative scar.
After complete wound healing, all patients noted a significant improvement in quality of life. The relocated flap created a load-resistant, full-fledged skin-fat layer that did not cause any inconvenience. Thanks to this type of plastic surgery, an increase in the angle of the intergluteal fold was achieved with a decrease in its depth, although the contour of the fold was always preserved and was not deformed.
The negative side of this method of plastic surgery was the long-term hypoesthesia of the transferred flap, which was observed in 11 (26.3%) patients. Despite the presence of scars extending beyond the sacrococcygeal region, all patients were satisfied with the cosmetic effect of the operation. The likely reason for satisfaction could be the significant predominance of men and the long existence of the disease, and the formation of scars was assessed as an inevitable price to pay for getting rid of a chronic purulent process.
In surgical treatment of the epithelial coccygeal tract, an important requirement is the radical excision of pathologically altered tissues, which are one of the causes of relapse of the disease. Treatment methods with primary restoration of the integrity of the skin have undoubted advantages [6, 9]. This ensures an early return of patients to their usual activities. Conventional wound suturing can be effective in excision of a simple fistula tract. However, with the complex location of the fistula tracts, their branching, the presence of cicatricial and inflammatory-infiltrative changes in the surrounding tissues, especially after previous attempts at surgical treatment, with radical excision quite large wound defects are formed, which cannot be closed by simply bringing the edges of the wounds together. In such situations, wounds can be left completely or partially open with prolonged healing by secondary intention, or closed using plastic movement of the skin, which, in our opinion, is preferable.
In addition, the choice of surgical method is influenced by unfavorable anatomical features such as high buttocks and a narrow deep intergluteal fold, which not only significantly worsen the quality of wound healing, but also lead to an increase in the number of relapses of the disease. Despite the controversial etiology of the epithelial coccygeal tract, almost all coloproctologists note that the most frequent occurrence of relapse of the disease is at the bottom of the intergluteal fold, which requires surgical treatment to make certain adjustments to the spatial structure of the sacrococcygeal region [3, 8].
Plastic surgery according to A.A. Limberg is attracted by the possibility of radical excision of pathologically altered tissues, preliminary planning of the size of the tissue to be moved, and a relatively simple technique. The presence of a wide, well-vascularized pedicle while preserving the subcutaneous tissue, and therefore the superficial and deep cutaneous vascular network, leads to the fact that disruption of the blood supply to the transferred flaps is quite rare [4, 5].
However, the classical implementation of this method leads to the location of the lowest point of the wound at the bottom of the intergluteal fold along the midline. A deep intergluteal fold (especially when the buttocks are closed to each other) creates conditions for the accumulation of skin secretions, skin maceration, and constant bacterial contamination due to poor aeration in this area. These factors have an adverse effect on the nature of healing of wounds located at the bottom of the fold, and also contribute to the penetration of hair into a poorly formed scar and, as a consequence, the occurrence of relapse of the disease [9, 10].
Considering the vulnerability of the symmetrical location of the rhomboid defect, we shifted the position of the “critical point” laterally, moving it from the depths of the intergluteal fold, which eliminates the impact of adverse factors on wound healing. A simple but important detail is the additional fixation of the flap to the bottom of the intergluteal recess, which helps maintain its contour and at the same time corrects the intergluteal angle, and also improves the healing of the flap.
Thus, the use of modified rhomboid plastic surgery according to Limberg in the surgical treatment of common forms of the epithelial coccygeal tract allows for radical excision of pathologically altered tissues with relatively simple skin-plastic closure of the wound defect with good early and long-term results.
conclusions
The optimal way to reconstruct small and medium-sized through defects of the palate and alveolar process is the reconstruction method with a FAMM flap; depending on the location and size of the defect, various flap configurations can be used with convenient positioning of the pedicle in the free interdental space near the defect. If one of the linear dimensions of the flap exceeds 35 mm, it is worth considering the possibility of using two FAMM flaps to close the defect and the possibility of recruiting the mucous membrane of the soft palate adjacent to the defect to freely align the edges of the flap with the edges of the defect. An obligatory component of the flap is an axial vessel (facial artery, a component of the FAMM flap), supplying blood to the recruited area of the buccal muscle (anterior or posterior, respectively), otherwise the flap will no longer be axial/perforating and there will be a risk of flap necrosis and defect recurrence. The choice of the donor site of the cheek is determined by the presence of interdental space, which makes it possible to conveniently insert the stem without resorting to tooth extraction, which avoids unwanted cosmetic defects in the dentition. In case of defects of the anterior and middle parts of the hard palate, we recommend using the FAMM flap configuration on the upper base, and depending on the size of the defect (if one of the linear dimensions exceeds 35 mm), consider the possibility of plastic surgery with two FAMM flaps with possible recruitment of the adjacent mucous membrane of the hard palate palate for free comparison of the edges of the flap with the edges of the defect.
Small isolated defects located strictly within zone II3a are well suited for reconstruction with a buccal mucomuscular flap on an inferior basis with a stem inserted in the retromolar region.
We do not recommend eliminating defects of the soft palate with a buccal mucomuscular flap due to the fact that this will not restore the phonation and swallowing functions of the soft palate, and we suggest looking for other alternative techniques.
Postoperative complications were presented in the form of ischemia of the end fragment of the flap (in 2 cases), which did not affect the successful outcome of the operation. In 2 cases, a hematoma was observed in the donor area, which did not require additional intervention. No cicatricial contracture or impaired mouth opening was observed.
As a result, 5-7 days after the operation, the patients returned to their normal rhythm of life and diet; no problems with breathing, speech, or taking liquid or solid food were found.
How the treatment method works
When planning local plastic surgery, it is necessary to determine the functional significance of the area of the defect to be closed, its size and relief, as well as the condition and reserves of adjacent tissues. When using methods of local plastic surgery, it is necessary to follow the general rules for this type of plastic surgery:
1) the skin and subcutaneous fatty tissue should be dissected at the same level, within healthy tissues, 3-5 mm away from the edge of the defect;
2) when mobilizing the edges of a wound or a displaced flap, subcutaneous fatty tissue must be completely included in the thickness of the mobilized tissue, separating it directly from the fascia;
3) sutures on the edges of the wound must be applied without tension, which can be judged by the color of the skin after applying the sutures. In order to ease the tension of the skin, it is permissible to tighten the tissue by placing sutures on the subcutaneous fatty tissue, and also to apply incisions to the entire thickness of the skin without damaging the underlying tissue;
4) if there is significant tension on the edges of the wound, causing concern for the outcome of the operation, another type of plastic surgery should be used. Simple approximation of the edges of the wound is applicable when closing a defect if the tissue around it is displaced. Good mobility of the skin is observed with prolonged use of prostheses. In this case, the delimited defects of the stump close freely, without tension on the edges of the wound. Approaching the edges of the wound after their mobilization with possible additional incisions is carried out with limited displacement of the skin of the stump surrounding the defect. To mobilize the edges of the wound, the skin with subcutaneous fatty tissue is separated from the fascia itself for a distance of 4-6 cm. Blood circulation and innervation are usually not disturbed. If there is a lack of plastic material, extended, parallel or unloading incisions are additionally made, which allow a more rational distribution of the mobilized tissues or an increase in their area. The shape of the cut depends on the specific conditions. Applying unnecessary incisions or a large number of unloading notches leads to the formation of unwanted additional scars on the skin of the stump.
Observation program after treatment method
Rehabilitation after plastic surgery usually includes a set of measures aimed at reducing swelling, eliminating hemorrhages, increasing muscle tone, and improving the quality of the skin. Rehabilitation programs should be aimed at improving the health of the body as a whole - its detoxification, improving microcirculation, increasing the intensity of metabolic processes, moisturizing and lifting the skin. On the other hand, they should be aimed at restoring the skin in the surgical area. When drawing up a rehabilitation plan, many factors are taken into account, including the patient’s health and age, the presence of chronic diseases, bad habits and other individual characteristics.
Prognosis after treatment method
Postoperative monitoring should be as close as operative monitoring. It is necessary to maintain body temperature and fluid balance. Pain relief is extremely important. The patient should not experience anxiety or malaise. A high level of observation and care for the patient is required, which is best achieved in the intensive care unit, where the patient should remain for the first 24-48 hours. In addition to monitoring the patient, it is necessary to carefully monitor the condition of the autograft. The surgeon or nurse on duty must constantly monitor the presence of a capillary reaction. In specialized microsurgery departments, monitoring of the patient and the condition of the autograft is carried out by a team on duty. If thrombosis is suspected, an urgent operation is required - thrombectomy. Complications that arise must be corrected as soon as possible, while the viability of the flap is still preserved. If everything goes smoothly during the flap transplant operation after removing the vascular clamps, the likelihood of complications is low. It increases in cases where there were difficulties in applying vascular anastomoses during surgery. A decrease in flap temperature compared to the patient's body temperature indicates arterial or venous insufficiency, or both complications. Blueness of the skin of the flap and accelerated capillary reaction indicate inadequacy of venous outflow, and vice versa: pallor, slower capillary reaction indicate arterial insufficiency. It is incorrect to assume that the success of a flap transplant depends only on the personal skill of the surgeon and on how skillfully he performed the anastomoses. Success, like failure, depends on the choice of the patient, the skill of the surgeons, anesthesiologist, and the staff of the operating room and recovery rooms.
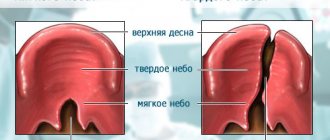
SYMPTOMS OF CLEFT PALATE
Symptoms of cleft palate are noticeable immediately upon birth. Breathing in such newborns is difficult, the air does not have time to warm up, so there is a predisposition to respiratory tract diseases. Due to the inability to suck, the baby has to be fed using additional devices. Pathological changes in the maxillofacial apparatus do not allow speech development. As a result of fluid accumulation, otitis media occurs, which can lead to hearing loss. With the appearance of teeth, their curvature, malocclusion, and extra teeth overlapping each other are noted. There is no physical or mental retardation in development, but children experience psychological discomfort and withdraw into themselves.
We know how to cure Cleft Palate
In the near future, a medical coordinator will contact you and advise you on the conditions and cost of treatment, select a doctor and make an appointment for you.
| Make an appointment | Or call us +375 29 699-03-03 +375 33 319-03-03 |