Home » All about modern dentistry » Pain relief in dentistry » Pain relief on the lower jaw Dental manipulations on the lower jaw are carried out using two types of anesthesia: infiltration and conduction.
Infiltration anesthesia in the lower jaw is used when premolars, incisors, and canines are removed. Conduction anesthesia is used for dental interventions near molars, and anesthesia of the inferior alveolar nerve is considered the most appropriate. In parallel, isolated blocking of the buccal and lingual nerves is used.
What is mandibular anesthesia
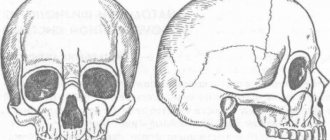
In pediatric dentistry, when treating primary teeth, they most often resort to mandibular anesthesia - anesthesia of the lower alveolar and lingual nerves. The inferior alveolar nerve arises from the mandibular nerve, passes through the mandibular foramen into the canal and branches to each tooth.
The action of the anesthetic solution is directed to the mandibular opening. Until the age of six, it is at the same level as the chewing surface of the primary molars, and then rises by 6 mm at the age of 9 and another 3 mm at the age of 12. Therefore, such exposure is not advisable until the age of six.
Since the inferior alveolar nerve is covered by a bony visor, it can only be reached in the groove of the mandibular nerve. The solution falls down under the influence of gravity. Before manipulation, it is recommended to palpate the edges of the mandibular ramus in order to determine the target point as accurately as possible. The needle is placed slightly above the mandibular foramen.
Material and methods
We examined 92 patients aged 21 to 50 years, without concomitant somatic diseases, who underwent surgical interventions on the lower jaw (removal of impacted and dystopic teeth, removal of teeth for chronic apical periodontitis, periodontal abscess).
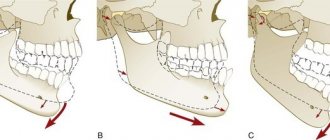
To determine the effectiveness of conduction methods of pain relief, we used a clinical assessment of the pain of interventions proposed at the Moscow State Medical and Dental University named after. A.I. Evdokimov. Heart rate, systolic and diastolic blood pressure were recorded. In all patients, we studied the dynamics of the amplitude of N2P2 oscillations - negative and positive waves, somatosensory evoked potentials: sensation threshold, pain threshold and pain tolerance level after blockade of the mandibular nerve as the most objective way to assess pain relief [11]. In 45 (48.9%) patients, conduction anesthesia was used on the lower jaw according to P.M. Egorov, in 47 (51.1%) - according to J. Gou-Gates modified by S.A. Rabinovich, O.N. Moskovets. In 26% of cases, anesthesia was performed in the presence of inflammation. The effectiveness of anesthesia was assessed by analyzing the zones of anesthesia, the time of onset of anesthesia (latent period) and its duration. An anesthetic based on articaine was used with a concentration of adrenaline: 1:100,000 and 1:200,000. Complications were recorded: the presence of hematomas, positive aspiration tests, post-injection pain, muscle trismus. With the method according to P.M. Egorov's solution fills the pterygomaxillary space, diffusing from the lower pole to the upper, and with the method according to J. Gow-Gates - from the upper pole to the lower [9]. Complex landmarks that require advanced skills in anesthesia according to J. Gow-Gates served as the basis for its improvement. Modified by S.A. Rabinovich and O.N. Moskovets, the direction of the needle is set by the position of the finger of the left hand in the projection of the neck of the condylar process, the lateral edge of which is the target point, which is achieved due to a certain position of the lower jaw during the injection. The results obtained were statistically processed using standard Microsoft Office 2000 programs on a personal computer.
Technique of mandibular anesthesia
In pediatric dentistry, this type of anesthesia is performed intraorally. There are various methods, but this one has proven to be the best.
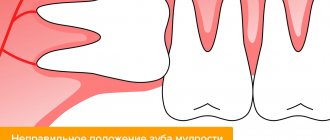
- The dentist determines the point at the intersection of the two lines. The horizontal line is a line running along the chewing surface of the lower molars or 3-5 mm above. The vertical line follows the direction of the pterygomaxillary fold.
- The injection is made at the intersection of these lines.
- After the injection, the needle is gradually advanced, releasing the solution, along the bone by 1.1-1.2 cm. During this period, up to 1 ml of medication must be injected.
- The correct position is this: the bevel of the needle is directed towards the bone, the syringe is deflected in the opposite direction.
- After the injection, the soft tissue in the injection area is pressed against the bone for 1-2 minutes.
Advantages and disadvantages
The main advantage of the technique is maintaining clarity of consciousness and the absence of pain.
In dental practice, several methods are used to assess the location of the needle and nerve endings:
- Ultrasound. Using special ultrasound equipment, you can see the exact location of the needle inside the maxillary bone. Thanks to visualization, the insertion process is significantly simplified, and also ensures precise localization of the alveolar process. Due to this, trauma is minimized.
- Neurostimulator. Allows you to determine the location of the nerve by assessing the distance of the needle from the required nerve endings. As for use in tuberal anesthesia, it is considered a method for the safe location of nerve processes.
Disadvantages include:
- high risk of damage to nerve endings and blood vessels;
- the likelihood of the drug entering the circulatory system;
- restrictions on the use of ultrasound and neurostimulators;
- lack of precise determination of the localization of nerves;
- greater likelihood of complications compared to other anesthesia techniques;
- increased morbidity.
Instruments and preparations
To implement the procedure, a dental spatula with a syringe is required. Anesthetics for local anesthesia are used for injection:
- Lidocaine. An inexpensive drug, produced in the form of a 1-2% solution. Contraindicated in patients with liver disease.
- Trimekain. It has higher efficiency and longer lasting effect compared to the previous one. However, there is a risk of developing side symptoms: nausea, loss of energy, dizziness.
- Ultracaine. A foreign drug that demonstrates high efficiency. It has a long-lasting effect and has impressive analgesic properties.
Extraoral route of administration
The patient turns his head to the side. The area where the drug will be administered is disinfected with alcohol. Next, the surface of the crest of the zygomatic-alveolar zone is palpated. The area where the medication is administered is stretched.
This method involves directly inserting a needle under the left cheekbone to a depth of 2 to 2.5 cm. The syringe is then pulled out to check if there is blood in it. If it is not there, then the painkiller is administered slowly.
The drug begins to act in 5-10 minutes. In this case, the patient may feel discomfort in the form of tingling and numbness.
Possible complications
- If you hit a large blood vessel, a hematoma can form.
- If the needle is not inserted deep enough, the anesthetic will not work because it will dissolve in the fatty tissue.
Intraoral route of administration
The patient relaxes his jaw and opens it halfway. The cheek is moved to the side using a dental spatula. The injection is placed under the junction of the buccal mucosa and the membrane of the alveolar ending.
The needle is located above the second molar, pressed into the hard tissue, then raised towards the upper jaw. The injection depth is 2-2.5 cm. The procedure is then carried out in exactly the same way as with the extraoral method.
Reference! Both methods involve injecting an anesthetic into the sinus between the fatty tissue and the optic nerve.
What happens after the introduction of conduction anesthesia?
2-3 minutes after the administration of the anesthetic, the patient may feel numbness, tingling and other unpleasant sensations in the lower lip and tongue. The closer the solution was injected to the inferior alveolar nerve, the faster the reaction will occur.
First, pain relief is noticeable at the end of the tongue, then spreads to the lower lip and the corner of the mouth. As soon as the patient’s entire tongue and lower lip are completely numb, this indicates that the anesthesia has taken effect and therapeutic manipulations can begin.
Results and discussion
The results of the first clinical signs of pain relief in the form of paresthesia in the area of the anterior third of the tongue and the corresponding half of the lower lip are presented in the table.
Clinical manifestations of anesthesia with methods of blocking the mandibular nerve according to P.M. Egorov and J. Gow-Gates, modified by S.A. Rabinovich and O.N. Moskovets The effectiveness of conduction anesthesia in the lower jaw according to P.M. Egorov was 92%, according to the modified method of J. Gough-Gates - 98%. In conditions of tissue inflammation when performing anesthesia according to P.M. Egorov noted effective pain relief in 89% of cases. When performing anesthesia according to the J. Gow-Gates method as modified, effective anesthesia occurred in 96%. At the same time, the number of complications, hematomas, positive aspiration tests, and post-injection pain was 1.9%. Slightly more (2.2%) local complications were observed during anesthesia according to P.M. Egorov.
When using the modified method according to J. Gou-Gates, when removing impacted and dystopic teeth, additional anesthesia was performed 2.6 times less frequently than using the P.M. method. Egorova. In addition, during anesthesia according to P.M. Egorov, insufficient anesthesia of the mucous membrane on the lingual side was identified in 3 (3.2%) patients, and on the buccal side - in 14 (15.2%) patients. With mandibular anesthesia according to the modified J. Gow-Gates method, insufficient pain relief on the lingual side was noted in 2 (2.1%) patients, and in the area of innervation of the buccal nerve - in 11 (11.9%) patients. Our data confirm that buccal nerve blocking is achieved in significantly fewer cases. A combination of any method of mandibular anesthesia with buccal nerve block is necessary.
Dynamics of somatosensory evoked potentials: after anesthesia according to the method of P.M. Egorov observed a rapid decrease in the amplitude of fluctuations of somatosensory evoked potentials. The amplitude of the sensation threshold reached its minimum values already at the 5th minute. When blocking the mandibular nerve according to the modified J. Gow-Gates method, the greatest decrease in the amplitude of fluctuations of somatosensory evoked potentials at all sensitivity thresholds was noted at the 10th minute, when determining the pain threshold and level of endurance - at the 10-15th minute. The dynamics of the amplitude of N2P2 oscillations of somatosensory evoked potentials at the sensation threshold, pain threshold and pain tolerance level after blockade of the mandibular nerve are presented in the figure.
Dynamics of the amplitude of N2P2 fluctuations (negative and positive waves) of somatosensory evoked potentials at the sensation threshold (TS), pain threshold (PT) and pain endurance level (PAL) after blockade of the mandibular nerve according to P.M. Egorov and according to J. Gou-Gates (modified) using a 4% solution of articaine with adrenaline at a concentration of 1:100,000.
Thus, clinical and physiological studies have shown that the effectiveness of conduction anesthesia in the lower jaw depends on the method of injection anesthesia, the composition of the local anesthetic drug, the type of dental intervention and the presence or absence of an inflammatory process in the anesthetized tissues.
Recommendations after the event
Any type of anesthesia is stress for the body, which must be minimized. Immediately after applying anesthesia, you must rise from the dental chair carefully to avoid dizziness. After pain relief, you must avoid drinking hot and alcoholic drinks. Do not massage the injection area or eat hot food. It is necessary to rinse your mouth with soda-salt or any other solution as prescribed by your doctor several times a day. It is better to sleep on the side opposite to the injection.
Possible complications
Mandibular anesthesia in rare cases leads to the development of complications. One of them is numbness of the tissues of the pharynx with subsequent limitation of movements of the lower jaw. Physiotherapy, mechanical therapy and administration of medicinal solutions are prescribed as treatment. A hematoma can occur as a result of damage to a vessel. If it does not resolve on its own, a puncture may be required. When a nerve is damaged, neuritis sometimes develops, the treatment of which requires physiotherapeutic procedures using heating elements or electric current. A very rare complication is temporary muscle paralysis as a result of medical error. If the injection technique is violated, the needle rarely breaks off and gets stuck in soft or tendon tissue. In such cases, surgical removal is used after an X-ray examination. If the needle does not cause concern to the patient and has grown into the tissue, it does not need to be removed.
Scope of application in dentistry
Mandibular anesthesia is used before any manipulation that is accompanied by pain:
- elimination of carious cavities;
- root canal treatment;
- extraction of teeth, including impacted ones;
- opening of abscess foci to extract pus;
- removal of sequesters;
- excision of the mucosal hood during teething;
- removal of cystic formations and tumors in the mobile jaw area;
- splinting for jaw fractures.