Indications for the use of antibiotics in dentistry
The need for treatment with antibiotics depends on the nature of the infection and the body's ability to withstand the course. The main reasons for prescribing antibiotics include:
- When advanced caries threatens pulpitis, the dentist may prescribe antibiotics to limit the spread of the pathological process. The patient is prescribed antihistamines to complement the effectiveness of antibiotics.
- With the development of an inflammatory process of periodontal tissue (periodontitis), antibiotic therapy allows the destruction of protozoa, gram-negative anaerobes in the oral cavity. Various dosage forms of drugs are used for treatment: gels, ointments, intramuscular and intravenous injections, tablets.
- The proliferation of pathogens, poor immunity, caries and dense plaque can lead to the development of gingivitis. After laboratory detection of the sensitivity of microbes to the antibiotic, a course of treatment is prescribed. Antibiotic drugs are mainly used for catarrhal gingivitis.
- The appearance of purulent accumulations inside the oral mucosa provokes the appearance of a fistula. The process occurs due to the proliferation of anaerobic gram-negative bacteria, streptococci, staphylococci, Pseudomonas aeruginosa or Escherichia coli. A doctor-prescribed course of antibiotics, which are also used for dental implantation, will help cope with the infection.
- Inflammation of the connective tissue around the root of the tooth is called periodontitis. The occurrence of the disease is a consequence of dental trauma, a complication of pulpitis, caries, or an error in dental treatment. If the process is not stopped, pus may appear. The effectiveness of antibiotics for periodontal disease is felt after preliminary cleaning of the periodontal tissue.
- The result of inflammation of various origins can be a granuloma - a cavity of granulation tissue filled with fluid. Location: on the gum near the root of the tooth. It is important to start treating granuloma in the early stages. The use of antibiotics facilitates the opening of the granulosa vesicle and suppresses the infection accumulated in it, and serves to prevent infection. Self-medication with antibacterial drugs is unacceptable.
Symptoms
The danger of a dental cyst lies in the fact that signs of pathology appear only when the neoplasm reaches a relatively large size. In the early stages, small cysts do not manifest themselves in any way, meanwhile the infectious process covers an increasingly larger area of healthy tissue. In the initial development of pathology, cysts are discovered by chance during routine examinations or treatment of other diseases.
The duration of the formation of a dental cyst takes only 1-2 days; as it develops, the following symptoms may occur:
- unpleasant and even painful sensations in the tooth, which intensify when chewing solid food;
- protrusion of the gum of a tooth, in the area of the root of which a cyst forms, the growth of the gum becomes larger over time, redness is observed;
- the formation of a fistula in the area above the root of the tooth, the release of serous or purulent accumulations from it;
- general weakness and malaise;
- increase in body temperature.
Note! When a dental cyst occurs, the symptoms are not immediately visible; they appear in the later stages of development. The pain when a tumor appears is aching in nature, but it is less pronounced than the pain caused by caries and pulpitis.
If a clinical picture occurs and you suspect a pathological process, be sure to consult a doctor. Under no circumstances should you resort to self-treatment - the dental cyst must be removed. In addition, taking the wrong medications can worsen the patient’s overall well-being.
Sometimes there is no pain in the oral cavity; instead, the basis of the clinical picture is intense headaches. The cause of this phenomenon may be a cystic formation in the maxillary sinus.
Types of antibiotics for toothache
Doctors use antibiotics in dentistry, which have a wide range of applications, to stop the growth and reproduction of mixed bacterial infections in the oral cavity. Drugs are divided into the following types:
Should I take an antibiotic for dental inflammation?
What to do if the gums become inflamed after the removal of a wisdom tooth, due to trauma, or with advanced caries? How to treat a complicated form of periostitis and periodontitis? The effectiveness of therapy largely depends on the selection of the optimal type of antibacterial drug to suppress the pathological process. It is useful to know when an antibiotic is prescribed for dental inflammation, which groups of drugs are most often used in dental practice.
Types of dental cysts
Tooth cysts have different classifications, each of which is formed according to certain characteristic parameters of the pathology.
According to the nature of the disease, they are distinguished:
- residual cysts – occur after tooth resection (removal) surgery; this is the most common type of cyst;
- retromolar – formed during severe eruption of wisdom teeth;
- radicular - cysts are located on or near the tooth root;
- follicular – at the heart of such cysts is the germ of a permanent tooth; follicular neoplasms arise as a result of poor quality care of baby teeth.
Classification of neoplasms according to their origin:
- odontogenic – arise as a result of the transition of the inflammatory process from other dental diseases;
- non-odontogenic - the causes of the development of such cysts include problems not related to the teeth and oral cavity.
Locations of cystic formation:
- anterior teeth;
- teeth that are adjacent to the nasal sinuses with their roots;
- wisdom teeth.
How to use an antibiotic for tooth inflammation with pus
At the first stage, while the pathological process is less active, rinses with an antibacterial effect are carried out as prescribed by the dentist.
Local medications act directly on the affected area and are less absorbed into the systemic circulation, which reduces the risk of side effects.
You need to crush the tablets of Lincomycin, Azithromycin or Tetracycline, combine them with lukewarm (not hot) boiled water, and rinse your mouth with the solution. The proportions of the components are selected by the dentist.
Active inflammatory process in the periosteum and gums after removal of the problem unit, with infection from the outside or hematogenously, flux is an indication for the prescription of antimicrobial compounds. It is important to prevent complications that develop when purulent masses accumulate or exudate exits into the oral cavity through the fistula. With the flow of blood and lymph, infectious agents penetrate into other parts of the body.
Periodontitis and periostitis in acute or chronic form are dangerous diseases. To heal the wound, the dental surgeon first cleans the affected area, removes a thick mass containing pathogens, particles of blood and mucus. The second stage is the prescription of antibacterial drugs. For purulent inflammation, penicillins show high effectiveness: Amoxicillin, Amoxiclav. Depending on the severity of the pathological process, antibiotics are taken orally or given injections.
If an odontogenic infection is detected, against which the gums fester, the use of the drugs Gentamicin, Grammidin C, Ciprofloxacin, Cifran is indicated.
Causes
Treatment of the disease primarily depends on the causes of its occurrence. Factors that often lead to inflammation:
- Untreated caries in a timely manner. In a mild form, the disease does not affect the pulp in any way, since the carious lesion extends only to the superficial tissues. As the crown is destroyed, caries affects all cellular structures and reaches the roots.
- Chronic periodontitis (except for mild forms). Deep periodontal pockets that form with this pathology reach the root plexuses. Pathogenic microorganisms that multiply in these cavities spread throughout the tooth and reach the pulp.
- Injury. Impact, bruise and other external influences contribute to the disruption of the established blood supply process and lead to a pathological process.
- Poor quality dental treatment. If the dentist did not clean the tooth cavity well before placing the filling, leaving carious particles, they will spread into deeper layers and reach the neurovascular bundle. Also, due to the fault of the doctor, the patient may receive a thermal burn of the pulp if the specialist neglected the rules while drilling the crown and did not cool it enough with water. The disease is also provoked by overdrying of the dentinal tubules by air flow.
- Exposure to acids, alkalis, medications, toxic filling compounds and other chemicals.
- Blood infection. Infection can penetrate into the pulp not only through carious holes, but also during sepsis.
- The patient's individual predisposition to tooth wear and the formation of mineral deposits in the pulp chamber.
Types of pathology
There are 2 main forms of the disease: acute and chronic. In the first case, a person suddenly experiences a sharp, paroxysmal pain (most often at night), which does not depend on external factors and does not go away when the irritants are eliminated. At first, a dark hole appears on the enamel, which grows over time and affects deep tissues, including reaching the canals.
If the inflammation does not go away after 3 weeks, the disease becomes chronic. Dull aching pains appear with a certain frequency and are disturbing not only at night.
Types of acute pulpitis:
- Focal. It is observed only for a few days. The pain lasts up to 20 minutes, with the intervals between attacks being about 2-3 hours. There is swelling of the gums.
- Diffuse. It extends to the coronal part, nerve endings and root. There is a disruption in the blood supply to tissues. The pain becomes throbbing and lasts much longer than with the focal form.
- Purulent. The cavity of the affected unit fills with pus. A painful pulsation is felt. The patient's condition is constantly deteriorating.
- Serous. Most often, this type is observed in children (pulpitis of temporary teeth). This is a pathology of infectious etiology, which is accompanied by short attacks of pain.
Classification of chronic dental pulpitis:
- Fibrous. Is a consequence of acute. It can proceed latently for several months with periodic periods of exacerbation. The gums are not swollen, the pain is aching and occurs infrequently.
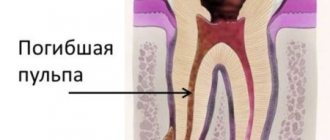
- Gangrenous. This is a complication of acute fibrotic disease, in which the death of pulp tissue and destruction of the coronal part occurs.
- Hypertrophic. In the carious cavity, tissues of a bright red hue are clearly visible, which constantly bleed, especially when pressed.
Symptoms
Despite the fact that each type of disease has its own distinctive features, there is a list of symptoms characteristic of all forms of pathology. At the initial stage of the disease, the tooth begins to react painfully to cold and hot, as well as to other irritants. Then a sharp throbbing pain appears, which intensifies at night and when lying down. Soreness occurs spontaneously or under the influence of irritating factors.
External manifestations of the disease, regardless of its type:
- darkening of the enamel;
- tooth mobility;
- bleeding;
- redness of the gums;
- swelling of the tissues around the diseased tooth;
The chronic form of pulpitis can be asymptomatic. It is characterized by a putrid odor from the mouth and aching pain.
Important! Very often the patient cannot understand which tooth hurts. The pain may radiate to the neck or ears. To determine the location of inflammation, a doctor’s examination and additional diagnostic tests are necessary.
Diagnostic methods
To make an accurate diagnosis, the dentist conducts and prescribes the following studies:
- inspection of the damaged cavity using a mirror and probe;
- checking the tooth’s reaction to temperature fluctuations (thermometry);
- exposure of the crown to a weak electric current (electroodontodiagnosis), with the help of which one can distinguish the disease from deep caries and determine in what form it occurs;
- X-ray.
Features of treatment
The therapeutic regimen directly depends on the stage of the disease and the location of inflammation. Treatment methods for pulpitis used in dentistry:
- Biological. Only the source of infection is eliminated, the progression of the disease is stopped, and the inflammation gradually goes away. Medicines are introduced into the cavity, which stop the growth and reproduction of pathogenic microflora and help eliminate inflammation.
- Conservative (vitalization). The doctor preserves the living pulp, but removes its coronal part. The tooth is completely preserved, while its functioning is restored.
- Devitalization. A special paste is placed into the drilled hole, which promotes the complete death of the pulp. The neurovascular bundle is removed, then the specialist places a temporary filling. When tissue inflammation completely disappears, the filling material is replaced with a permanent one. Devitalizing paste is used by pediatric dentists for tooth pulpitis in a child.
- Surgical. Surgical removal is divided into amputation (partial removal of pulp tissue) and extirpation (the pulp is completely removed).
Attention! The sooner the patient contacts the dentist, the higher the likelihood that the tooth can be saved. A qualified doctor will be able not only to cope with swelling and inflammation, but also to restore the integrity of the crown and restore the lost whiteness of the enamel.
Is it possible to cure a disease with folk remedies?
Pulpitis requires qualified medical care and cannot be treated on its own. Home methods for relieving pain and reducing inflammation can only temporarily alleviate the patient’s condition. Without timely conservative or surgical treatment, severe complications are possible.
Possible complications
If you do not receive treatment on time or do it incorrectly, the risk of complications increases, such as:
- periodontitis (damage to hard tissues around the tooth root with pulpitis);
- periostitis (inflammation of the periosteum, or flux);
- abscess (purulent inflammation accompanied by intoxication of the body);
- sepsis (blood poisoning);
- chronic pathologies of internal organs and systems.
Preventive measures
In order to avoid long-term treatment and surgical intervention, you need to take care of the prevention of pulpitis by adhering to the following rules:
- brush your teeth 2 times a day, rinse your mouth after eating, remove plaque and tartar in a timely manner;
- visit the dentist for preventive examinations at least once every six months;
- do not use toothpicks or other traumatic devices;
- eat a balanced diet, ensure that the body receives a sufficient amount of vitamins and minerals;
- give up bad habits (smoking, drinking alcohol), large amounts of sugar and junk food;
- treat caries and other dental pathologies in a timely manner, without bringing them to severe stages.
Sharp pain radiating to the neck, temples or ears is a reason to urgently visit a dental clinic. If treatment is not started in time, serious complications are possible, including complete tooth loss and a septic process.
By following preventive measures, you can protect yourself from the occurrence of pulpitis and other oral diseases.
Names of antibiotics used for inflammation of the dental nerve and root
The dentist prescribes medications to suppress infection based on the results of an examination of the problem area. When the nerve is inflamed, it is difficult to eat and drink; throbbing or aching pain accompanies a person throughout the day and intensifies at night.
Before starting therapy, the doctor conducts an allergy test and interviews the patient to identify contraindications.
Antibiotics help eliminate inflammation of the root and dental nerve:
- Ciprofloxacin.
- Azithromycin.
- Amoxiclav.
- Azithromycin.
- Ampiox.
- Doxycycline.
- Digital
Pulpitis of the tooth and its treatment
A characteristic sign of this pathology is inflammation in the pulp, which is located inside the tooth cavity, where blood vessels and nerves are concentrated. The cause of inflammation is the penetration of harmful bacteria into the cavity due to damage to the external dental tissues (enamel and dentin). This is the destruction that we most often owe to untimely treatment of deep dental caries: pulpitis becomes a consequence of the carious process. Much less often, it appears due to mechanical damage to the pulp, poor preparation of the tooth for filling, and unprofessional installation of orthopedic structures.
Treatment methods for pulpitis
In dentistry, two main methods are used to treat dental pulpitis in adults and children:
- biological - drug treatment of pulpitis with antibiotics and medications;
- surgical - treatment of pulpitis by amputation (partial removal of the pulp) or extirpation (in which the nerve of the tooth is completely removed).
The choice of technique remains with the dentist. The doctor studies X-ray diagnostic data, interviews and examines the patient. Based on these data, he selects the most rational method of treating pulpitis for a particular case.
List of effective antibacterial agents for dental infections under the crown
After endoprosthetics and implant installation, some patients complain of discomfort. Pain and inflammation are a consequence of a violation of the technology for fixing artificial teeth and crowns: the dentist did not completely fill the cavity inside the problem unit or mechanical damage to the canal walls occurred. If the implantologist is poorly qualified, the pin may be installed incorrectly. Perhaps the smallest parts from dental instruments remain inside the canal.
There are several causes of the pathological process and pain syndrome:
- swollen gums or gumboil (acute inflammation);
- cyst - a cavity with fluid near the root of a problematic unit of the dentition;
- inflammation of the submandibular salivary glands;
- dental granuloma;
- a fistula on the gum is a hole through which purulent masses are released.
With the development of inflammation in periodontal tissues, an abscess forms at the root apex. Painful sensations are a consequence of the active accumulation of exudate and pressure on neighboring areas.
The main condition for eliminating discomfort is a timely visit to the dentist to remove the crown, clean the root canals, and eliminate the cause of the inflammatory process. Uncontrolled use of antibiotics can harm the body.
Before treating the canals, the doctor makes an injection into the gum, removes the prosthesis, and examines the affected area.
Effective antibiotics are prescribed to suppress the infection:
After the removal of a wisdom tooth, there is an increased risk of not only inflammation, but also bleeding from the socket.
If the patient takes the drug Warfarin to prevent thrombosis, then you need to warn the dentist: the doctor temporarily stops taking the medication for several days before and after the extraction of the “eight”, be sure to coordinate this action with the cardiologist.
It is important to know how to combine an antithrombotic agent with antimicrobial compounds.
What is a dental cyst?
Tooth cyst - what is it? An odontogenic cyst is a pathological neoplasm that occurs in the upper part of the tooth root. The internal cavity of the cyst is filled with liquid or mushy purulent contents; it is enveloped by a dense layer of epithelium.
The size of the cyst starts from a few millimeters, with rapid development reaching several centimeters in circumference. Most often, the pathological process affects the upper jaw, since the roots of its teeth have a more porous structure.
In order to understand what a dental cyst is and how to treat it, you need to know why such a phenomenon occurs. The formation of cysts occurs as a result of inflammation, thus the body restricts healthy tissue from the affected areas, clogging them along with bacteria into bubbles.
The use of antibiotic therapy during pregnancy and lactation
Most antimicrobial agents are prohibited for use by expectant mothers and during breastfeeding. When prescribing antibiotics to suppress the purulent-inflammatory process in the gums and periosteum, the doctor takes into account the benefits for the woman and the possible risk for the developing fetus.
With the active spread of infection, suppuration, development of sepsis, severe complications against the background of the pathological process, it is possible to take certain groups of antibacterial agents. The new generation of antibiotics is less toxic to the fetus.
Under strict medical supervision, in the minimum effective dose, the following is prescribed:
- Ornidazole;
- Metronidazole;
- Josamycin;
- Azithromycin;
- Clarithromycin;
- Clindamycin;
- Cefepime;
- Ceftaroline.
The list of approved drugs is indicated by the dentist. The best option is to additionally consult with a gynecologist managing the pregnancy.
Anti-tuberculosis antibiotics are allowed to be used by pregnant women in combination with other drugs according to a specific regimen for a long period.
Biological method of treating pulpitis
If the disease has become chronic, a biological method or conservative treatment of pulpitis with calcium is used. The process involves applying therapeutic pads containing calcium preparations. The technique is also used in the following cases:
- if the pulp was accidentally exposed during the caries treatment procedure;
- when you need to strengthen the bone partition between tooth enamel and pulp.
The specialist applies a drug for the treatment of pulpitis to the site of thinning bone tissue and thereby strengthens it. Next, the tooth is filled and monitored over time, conducting X-ray examinations at certain time intervals. The method is suitable:
- children with baby teeth;
- patients under 30 years of age during the treatment of reversible pulpitis;
- everyone who takes special care of their oral cavity.
If, after treatment of pulpitis, the tooth aches, hurts when pressed or bitten, and the pain remains for a long time, intensifies at night, and becomes long-lasting, you must return to the clinic. Aching pain during the treatment of pulpitis indicates that more radical, that is, surgical, methods are needed.
Contraindications to treatment with antibacterial drugs
Compositions for suppressing the inflammatory process in gingival and bone tissue during toothache are not suitable for all patients. Restrictions for use are related to age, body reactions, and special conditions. Most antibacterial drugs should not be used by nursing mothers or pregnant women.
Main contraindications for antibiotic therapy:
- allergic reactions;
- liver and kidney failure;
- intolerance to the active substance: you need to choose a substitute with another active ingredient;
- myasthenia gravis;
- damage to the optic nerve;
- severe diseases of the gastrointestinal tract;
- the patient is taking medications that are incompatible with a certain group of antibiotics;
- tendinitis;
- epilepsy;
- children's age (restrictions are indicated in the instructions for the drug).
A limited range of antibacterial compounds are used in pediatric practice.
It is important to clarify in the instructions the age of the child for safe antibiotic therapy for acute inflammation of tissues in the oral cavity.
In case of purulent inflammation, the development of periostitis and periodontitis, when the gums are swollen, the dentist selects effective antibacterial compounds. Many inexpensive antibiotics work well for dental inflammation and quickly suppress the pathological process. New generation drugs with a minimal list of contraindications and side effects are safer.
Antibiotics for toothache.
Many people consider antibiotics a panacea for all ills and, at the first problem with their teeth, begin to take them intensively. However, such self-medication can cause irreparable harm to other organs and systems of the body, without improving the condition of the teeth. Prescribing antibiotics is the exclusive prerogative of the doctor. In what cases are these medications prescribed?
Treatment of hyperplastic (hypretrophic) gingivitis
At the first stage, the same set of measures is provided as for catarrhal gingivitis.
If the treatment is ineffective, sclerotherapy is indicated: injections into the gingival papillae of sterile hypertonic solutions (10% calcium chloride or gluconate solution, 40% glucose solution, 90% ethyl alcohol). The administration of 0.1-0.3 ml of such solutions is carried out under local anesthesia. The injection is carried out with a thin needle from the top of the papilla to its base simultaneously in 3-4 papillae. The interval between injections is 1-2 days, the course is 4-8 injections. Pregnant women with this form of gingivitis do not undergo sclerotherapy.
Treatment of ulcerative-necrotizing gingivitis
Includes:
- relief of acute gum inflammation;
- reducing intoxication of the body, increasing the resistance of the body and periodontal tissues;
- elimination of local unfavorable factors that may contribute to the progression of the inflammatory-destructive process.
The treatment plan repeats the sequence of medical actions for other inflammatory periodontal diseases, but there are some features [10, 19, 20]:
- professional hygiene is carried out in stages under local anesthesia (applications, oral baths with lidocaine solution; if necessary, infiltration or conduction anesthesia);
- at the first visit, only supragingival dental deposits are removed;
- other local measures are carried out as the inflammatory process subsides.
It is important that both the doctor when seeing a patient and the patient at home use antiseptics that release atomic oxygen and chlorine-containing solutions, which have an adverse effect on the anaerobic microflora. Acceleration and facilitation of the removal of necrotic tissue from the surface of the gum lesion is ensured with the help of proteolytic enzymes. To optimize the epithelization of tissues (after cleansing them from a film of necrotic tissue), keratoplasty preparations are used.
Systemic (general) therapy for patients with necrotizing ulcerative gingivitis includes (Table No. 1):
- antibacterial drugs (beta-lactam antibiotics - penicillins and cephalosporins), tetracycline antibiotics, macrolides, antiprotozoal drugs (metronidazole);
- anti-inflammatory drugs;
- vitamins, adaptogens;
- hyposensitizing agents.
Criteria for assessing the effectiveness of complex treatment of inflammatory periodontal diseases can be:
- improvement of the patient’s general condition;
- relief of inflammation - in acute gingivitis;
- stabilization of periodontal status - with periodontitis;
- improvement of parameters assessed by additional research methods.
We are far from thinking that we were able to take into account and present all aspects of complex therapy, and especially drug therapy, for inflammatory periodontal diseases, and we admit that some of the materials were not included in this publication. Therefore, all constructive comments from readers will be received with gratitude.
For readers interested in this issue, we provide a list of recommended literature.
LITERATURE
- Abaev Z. M., Domashev D. I., Antidze M. K. et al. Modern methods of treatment and prevention of periodontal diseases // Dentistry. - 2012, No. 4. - P. 72-74.
- Wolf G.F., Rateitzhak E.M., Rateitzhak K. Periodontology; lane with German; edited by G. M. Barera. - M.: MEDpress-inform, 2008. - 548 p.
- Goncharova E.I. Herbal remedies in the prevention and treatment of periodontal diseases // Ros. stoma magazine. - 2012, No. 3. - P. 48-52.
- Grudyanov A.I. Periodontal diseases. — M.: Publishing house “Med. information agency", 2009. - 336 p.
- Grudyanov A.I., Aleksandrovskaya I.Yu. Planning of therapeutic measures for periodontal diseases. — M.: LLC “Med. information agency", 2010. - 56 p.
- Grudyanov A.I., Ovchinnikova V.V., Dmitrieva N.A. Antimicrobial and anti-inflammatory therapy in periodontology. — M.: LLC “Med. information agency", 2004. - 80 p.
- Periodontal diseases. Modern view on clinical, diagnostic and therapeutic aspects: study. village, recom. UMO MH&SR and Ministry of Education. RF / Yanushevich O. O., Grinin V. M., Pochtarenko V. A., Runova G. S. et al.; edited by O. O. Yanushevich. - M.: GEOTAR-Media, 2010. - 160 p.
- Krazhan D.S., Garazha N.N., Orlov M.N., Morgoeva Z.Z. Potentiated effect of antiseptics and sorbents on the microflora of periodontal pockets // Med. Bulletin of the North Caucasus. - 2012, No. 2. - P. 40-42.
- Lobko S. S., Khomenko A. I., Shadurskaya S. K., Petruk A. A. Therapeutic dentistry: Etiotropic therapy of marginal periodontal diseases: Textbook. allowance. - Mn.: BSMU, 2001. - 70 p.
- Makeeva I.M., Kudryavtseva T.V., Erokhin A.I., Akulovich A.V. Periodontal diseases: a guide. to practice therapist classes. dentistry for students IV and V courses of stoma. faculties. - MEDpress-inform, 2009. - 96 p.
- Makeeva I.M., Smirnova T.N., Chernousov A.D. et al. The use of lactoferrin in the complex treatment of dental diseases (literature review) // Dentistry. - 2012, No. 4. - P. 66-71.
- Müller H.-P. Periodontology; lane with him. - Lvov: GalDent, 2004. - 256 p.
- Patient management plans. Dentistry / ed. O. Yu. Atkova, V. M. Kamenskikh, V. R. Bosyakova. - M.: GEOTAR-Media, 2010. - 240 p.
- Platonov I. A., Andreeva T. A. Workshop and methodological guidelines on pharmacology. Part 2. Ed. prof. I. A. Platonova. - Smolensk, 2009. - 106 p.
- Modern aspects of clinical periodontology / Ed. L. A. Dmitrieva. - M.: MEDpress, 2001. - 128 p.
- Therapeutic dentistry: national. manual / ed. L. A. Dmitrieva, Yu. M. Maksimovsky. - M.: GEOTAR-Media, 2009. - 912 p.
- Filatova N.A., Elizova L.A., Chekhova N.O., Kostryukov D.A. Possibilities of achieving stabilization of the inflammatory process in periodontitis // Int. scientific-practical conf. "Achievements and prospects in dentistry." - 1999. - T. 1. - P. 257-260.
- Tsarev V.N., Ushakov R.V. Antimicrobial therapy in dentistry: Guide. — M.: Med. information agency, 2004. - 144 p.
- Tsepov L. M. Periodontal diseases: a look at the problem. - MEDpress-inform, 2006. - 192 p.
- Tsepov L. M., Nikolaev A. I., Mikheeva E. A. Diagnosis, treatment and prevention of periodontal diseases. — 3rd ed., rev. and additional - MEDpress-inform, 2008. - 272 p.
- Tsepov L. M., Nikolaev A. I., Nesterova M. M. et al. System doctor - patient - periodontal pathology: reasons for suboptimal interaction that reduces the quality of dental care // Dental South. - 2012, No. 8. - P. 28-29.
- Yudina N. A., Lyugovskaya A. V., Kurochkina A. Yu. Antimicrobial therapy in the treatment of periodontal diseases: educational method. allowance. - Minsk: BelMAPO, 2008. - 42 p.
Are antibiotics effective?
Before starting a course of antibiotics, you should determine the cause of your toothache. There are two main factors that provoke it:
- Caries that has developed to pulpitis. When the carious process affects the nerve, the tooth begins to react to various irritants: sour, sweet, cold, hot. Since in this case the pain is provoked by an intradental inflammatory process, antibiotics will be completely useless. For such pain, anti-inflammatory drugs, for example, Ibuprofen, are relevant. In addition to drug treatment, it is also planned to remove the affected tissue and fill the dental canals.
- An infection localized in a “dead” tooth. In such a situation, after removal of the nerve, the tooth does not react to sour, sweet and other irritants, but at the same time it hurts - and more and more every day. It's all about microbes that multiply either in an unfilled canal or in some tiny crack in the root. As a result, a purulent abscess or gumboil develops near the root of the tooth. The latter, by the way, is deadly. If such inflammation of the tooth root occurs, antibiotics are prescribed, but before taking them the patient will have to undergo the procedure of opening the abscess.
Before pinning any hopes on antibiotics, you should understand a few facts about this group of drugs:
- antibiotics help in treating the disease that provokes toothache, and do not relieve the pain itself (there are analgesics for this purpose);
- different antibiotics have different effects on pathogens, so it is almost impossible to successfully select such a medicine on your own;
- the effectiveness of taking antibiotics without concomitant dental treatment tends to zero.
The course of antibiotic treatment should not be interrupted prematurely: incomplete therapy will not lead to the desired result.
Treatment at the dentist
The doctor begins treatment by washing the socket and treating it with antiseptic solutions, and then cleans the socket from the remains of the blood clot using a surgical curette. Then the wound is dried with a gauze swab and treated with an anesthetic and antibacterial agents. The wound is covered with a bandage, which is designed to protect the open surface of the wound from possible biological, chemical or mechanical irritants. To check the possibility of detecting pieces of the extracted tooth in the socket, an x-ray can first be taken.
The procedure for cleaning the hole as a whole is carried out according to the following scheme:
- Local anesthesia is performed;
- The well is washed with an antiseptic solution (hydrogen peroxide solution 3%, chlorhexidine 0.05% or furatsilin 0.02%), and food debris and necrotic masses are removed;
- If there are foreign bodies in the hole (root fragments, cysts and granulomas), they are removed using special instruments;
- After cleaning the hole, it is treated with antiseptic solutions, dried with a sterile gauze swab, and turunda with an antiseptic and an anesthetic is injected into it. With a mild degree of inflammation, a turunda may not be necessary; thorough cleansing of the hole and subsequent care for it is sufficient;
- In case of a pronounced necrotic process in the hole, rinsing and application with trypsin is carried out - this is an enzyme preparation that accelerates the breakdown of dead tissue. Trypsin has anti-inflammatory and anti-edematous effects, helps clean the socket from necrotic masses and pus;
- After completing all the manipulations, the patient goes home, the doctor appoints appointment days when he needs to come for antiseptic treatment of the hole and change the turunda, if one has been installed. If necessary, a course of antibiotics is prescribed.
For alveolitis, antiseptic baths (not rinsing) with solutions of chlorhexidine 0.05% or miramistin 0.01%, which can be purchased ready-made at the pharmacy, are effective. When performing baths, the solution is taken into the mouth and held for several minutes, then carefully spat out. To relieve pain and reduce the degree of inflammation, nimesulide or ibuprofen are prescribed.
To prevent the turunda from falling out of the socket, during treatment you need to eat soft, pureed food and do not chew on the sore side. If the turunda does fall out, you need to rinse your mouth with chlorhexidine solution and immediately consult a doctor.
If this is not possible, you should rinse the hole yourself from food debris: to do this, bite off the sharp tip of the needle from a 5 ml syringe, bend it a little, and disinfect it with pure alcohol. A chlorhexidine solution is drawn into the syringe, the needle is inserted into the hole (not too deep) and the piston is pressed intensely to create a liquid pressure that can remove food debris.
All cases of alveolitis treatment are individual, so it may be necessary to visit the dentist up to several times.
With a favorable course of the healing process, the pain goes away, and the inflammatory process gradually subsides and disappears after a few days.
If the process, despite the procedures performed, progresses, then after antiseptics, gauze tampons soaked in propolis tincture or camvorophenol solution (10%) are inserted into the hole. A tetracycline-prednisolone cone inserted into the well has a good antibacterial effect.
How much does tooth treatment for pulpitis cost?
The final cost of pulpitis treatment is influenced by many factors: the degree of destruction of hard tissue, the number of canals in the tooth, the presence of complications, concomitant diseases, and the chosen treatment method. If the tooth is permanent and has one canal, then the procedure in Moscow clinics will cost from 5,000 rubles. This amount includes a full range of services: x-ray diagnostics, application of anesthetic, installation of a rubber dam, treatment of caries, treatment of dental canals with cleaning, installation of a filling. Price may change if multiple sessions are required.
Is it painful to treat pulpitis?
Many patients believe that treatment for pulpitis is painful. In fact, pain accompanies the disease itself, and not the procedure for its treatment. The pulp tissue and nerves become inflamed, which causes unbearable painful sensations comparable to an electric shock. Pulp removal is absolutely comfortable, because high-quality anesthetics completely relieve the patient of pain while the doctor prepares the canals. During treatment or after treatment of pulpitis, the tooth hurts when the internal tissues are severely inflamed. Then safe painkillers are prescribed while healing occurs (1 - 3 days).
Possible complications
If you delay visiting the dentist, inflammation can spread to the bone tissue of the tooth - periodontium. This is how one of the most common and dangerous complications of this disease begins - periodontitis, which can lead to tooth extraction. Periodontitis also occurs due to an unskilled approach to cleaning root canals.
If you are concerned about an elevated temperature after treatment for pulpitis, urgently contact a more reputable dentist, as the inflammation is progressing. Professional clinics use modern methods of canal treatment using microscopes, binoculars, visiographs, endomotors, and apex locators. These instruments prevent the risk of complications.
Unfortunately, pulpitis remains a common occurrence after caries treatment. The reason for its appearance is the same - the unprofessional actions of a doctor who violated medical protocols and made mistakes when filling. Perhaps he accidentally opened the pulp and gave bacteria access to it.
Stages and stages of tooth treatment for pulpitis using the devital method
- Stage I.
The tooth is anesthetized and the carious cavity is cleaned. The pulp cavity is opened. - Stage II.
A devitalizing paste is placed into the exposed pulp and the tooth is filled for 3 to 7 days. People still call the paste “arsenic,” although it has nothing to do with this substance. - Stage III.
During your next visit, your dentist will clean the root canals according to medical protocol. - Stage IV.
If there is a risk that the tooth will crack, it is covered with a crown. If the hard tissues are well preserved or only slightly damaged, they are restored. The tooth is strengthened with a fiberglass or metal anchor pin and securely filled with photopolymer material.
The treatment time for pulpitis depends on how damaged the tooth is, the age of the patient, whether there are complications, and how many root canals should be treated.
How is pulpitis treated surgically?
As we have already noted, there are two possible options for surgical intervention:
- treatment of pulpitis using the amputation method with partial preservation of the pulp;
- treatment with complete removal of soft tissues, blood vessels, and nerves.
If there is an objective possibility, the doctor will remove only the top of the pulp - from the crown, leaving the root part. The blood supply and sensitivity (innervation) of the tooth will be preserved. The technique is used in the treatment of children - for milk or permanent teeth that have not yet fully grown. This allows them to form normally in the future. Treatment for pulpitis can be carried out in one visit.