A deep bite is a developmental anomaly of the oral cavity in which the upper incisors almost completely overlap the lower ones. It not only distorts the proportions of the face, but can also cause speech disorders, increased tooth wear and trauma to soft tissues. Pathology can be detected both in early childhood and in adulthood. Treatment depends on the severity, but most often involves braces, plates, or orthodontic surgery.
Signs of a deep bite
Signs depend on the severity of the abnormality.
Mild degree
Often the patient does not notice the external manifestations of the pathology, because with a mild degree, the abnormal bite may not even distort facial features and speech. The main signs are small chips and microcracks of the upper front teeth.
Average degree
In addition to small cracks and chips, the following violations appear:
- increased abrasion of the enamel of the upper teeth on the inside;
- difficulties in pronouncing the sound “s”;
- the lower third of the face visually moves away, its height decreases;
- the act of biting is distorted, which leads to disruption of the entire chewing process;
- problems in the functioning of the temporomandibular joint (clicking, crunching and sometimes pain; it is difficult for the patient to open his mouth wide);
- the lips close unaesthetically - the lower or upper lips come forward strongly.
Severe degree
The most severe consequences of improper jaw development manifest themselves, namely:
- Violations of facial proportions.
Often such distortions are called a “bird” face, when the chin goes back strongly and the upper lip hangs excessively over the lower lip. The lower third of the face is also reduced.
- Trauma to the palate.
Due to the distal bite, the lower incisors reach the upper palate. Soft tissues are subject to mechanical friction not only during eating, but also at rest.
- Deformation of the upper jaw.
The upper teeth protrude forward, and the distribution of the load during chewing becomes completely uneven.
Fix a gummy smile
If your gummy smile is caused by a short upper lip or overactive muscles. There are several relatively simple medical and aesthetic solutions to improve the appearance of your gums when you smile. Without worrying about surgery. After all, your smile should light up the room, not make you feel self-conscious! Continue reading to learn more about how to correct a gummy smile and the available treatment options in cosmetic injections.
Fix a gummy smile
What is a gummy smile?
The technical term for a gummy smile is excessive display of gums. And it is determined when 2-4 mm of gums are visible when smiling. A smeared smile is the result of various factors, whether it be excessive expression of gum tissue. Which makes teeth appear shorter than they are, or a thin upper lip. Overactive muscles around the upper lip. Can cause more gum tissue to be visible when you smile. Or the way the upper jaw developed could also be a factor.
Lip fillers for a gummy smile
Lip fillers, also known as dermal fillers, are a quick way to reduce the amount of visible gum. Increasing the thickness of the lips and helping to balance the shape. Typically, filler is only injected into the upper lip, but this is a choice that can be made in consultation with your nurse or doctor.
Anti-wrinkle injections for a gummy smile
Anti-wrinkle injections help those whose gummy smile is the result of overactive muscles around the upper lip. By targeting overactive muscles or the muscles near the nose, anti-wrinkle injections relax said muscles and ultimately reduce the amount of gum showing when smiling because the newly relaxed muscles don't pull as much on the upper lip. Anti-wrinkle injections can last up to 12 months. They are non-invasive and only take about 30 minutes with no downtime required.
Fix a gummy smile
Fix a gummy smile
So what makes my smile gummy?
A NUMBER OF FACTORS CAN RESULT IN A GUMMY SMILE
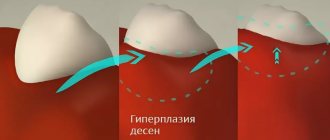
Too much gum tissue
Some of us simply have more gum tissue than others. In some cases, the teeth appear short. Because they have not completely erupted from the gums and are still partially covered by gum tissue. Gums can also grow over teeth due to a condition called gingival hypertrophy.
Worn or short teeth
Your teeth may appear small compared to your gums. If they are worn out or are naturally shorter than average.
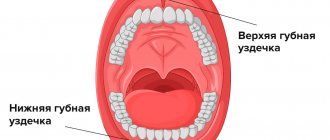
Short or overactive upper lip
If your upper lip is too short when you smile, it may expose more gums. In other cases, the upper lip is of normal length, but rises too high when smiling .
Jaw problems
Excessive growth of the upper jaw, known as vertical maxillary excess. May cause gums to swell and disrupt the proportions of your smile .
Fix a gummy smile
What should I do if I think my smile is gummy?
Your doctor can evaluate your smile
If you are concerned about how much gum tissue is visible when you smile, your dentist can perform an examination and explain treatment options. During your visit, your doctor will examine your teeth, gums, and jaw to determine the cause. Impressions and x-rays may also be needed.
Can I stop my smile from looking gummy?
Most Causes of a Gummy Smile are HEREDITARY
Unfortunately, when a gummy smile is caused by genetics, there are no reliable methods of prevention. However, by visiting your dentist regularly, you can resolve teeth grinding and other problems. Which can ultimately lead to a gummy smile.
What is considered a “gummy smile”?
Dentists Say SHOWING THREE MILLIMETERS OF GUM TISSUE OR LESS IS NORMAL
“Anything that shows a smile larger than three to four millimeters begins to look gummy.”
The best treatment option for you DEPENDS ON THE CAUSE OF YOUR GOOMY SMILE
One of the most common treatment methods is medical-aesthetic solutions. For patients with a slightly gummy smile, laser gum contouring is an option. Your doctor may use a soft tissue laser to remove gum tissue. By improving the proportions between teeth and gums, a short upper lip will make you feel self-conscious.
Embrace your smile
You're not alone - some of the most recognizable smiles in the world. Including Nicole Kidman, Jennifer Garner and Gwen Stefani, have a gummy smile! Every person's smile is unique and deserves to be celebrated!
If a gummy smile leaves you or someone you like less laughing at you. The Cosmetology Clinic offers free consultations with our certified cosmetologists.
Fix a gummy smile
Causes of deep bite
Heredity
One of the child’s parents may have a pathology of distal occlusion or other problems that affect its development in the offspring.
For example, there are such variants of the abnormal structure of the parent’s face, which can lead to a deep bite in the child:
- Macrogeny.
The upper jaw is significantly enlarged, and the lower jaw is developed normally. A large upper jaw is a dominant trait that is transmitted genetically.
- Microgenia.
The lower jaw is underdeveloped, while the upper jaw is developed normally. This situation indicates chromosomal disorders, for example, Patau syndrome or Edwards syndrome.
Pathologies of intrauterine development and the postpartum period
The formation of the jaw system occurs approximately in the 5th week of pregnancy. If a woman is diagnosed with an intrauterine infection, fetal hypoxia, a delay in its development and other similar pathologies, this may subsequently cause a distal bite.
Jaw growth, taking into account genetically determined data, begins after birth, during breastfeeding. Its absence or incorrectly similar nipples (the holes of which are too large, as a result of which the child does not make sucking efforts) can also affect the condition of the teeth, as well as the following problems:
- hypotrophy,
that is, the baby’s lack of weight in relation to his height.
- Rickets.
This disease is associated with disorders of bone formation (bones do not develop quickly enough). It most often occurs in infants and young children.
- Defects of the musculoskeletal system.
For example, muscular torticollis, postural disorders, as well as other pathologies of bone tissue.
Important!
A deep bite can appear due to the child’s bad habits - frequent and excessive sucking of a pacifier and/or finger, biting the lip.
Disturbances in dental development
The following dental pathologies can provoke distal bite:
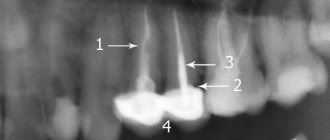
- Super eruption or extrusion
(“rabbit” teeth, that is, excessively elongated front incisors of the upper jaw).
- Insufficient eruption of lateral teeth
due to early loss of lateral primary teeth (which ideally fall out around 9–12 years of age).
- Loss of molars at an early age.
Permanent back teeth usually appear before the age of 13.
- Increased abrasion.
We are talking about the side teeth, which wear out much faster than normal. Most often this is associated with bruxism - active grinding, for example, while eating or sleeping.
Lip contouring and teeth whitening
When to perform lip contouring: before or after whitening
Expert opinion
: Svetlana Serova, hygienist at the German Implantology Center
In my opinion, teeth whitening is worth thinking about before lip contouring
, I'll explain why.
Before teeth whitening, therapeutic procedures are mandatory, all caries, all gum inflammation, if any, are treated.
and also professional teeth cleaning is carried out - plaque and tartar
:
All this is necessary so that the whitening composition does not cause pain when applied, and after the procedure we get the result we need:
A situation may arise that there will be carious lesions on several teeth; accordingly, the entire treatment process may take some time, and if lip contouring is done earlier, then there is a high probability that you will have to go without snow-white teeth for some time.
I want to say that lip plastic surgery, no matter what material it was used for, is still an intervention, albeit a small one, and time must pass before the slight swelling subsides and everything “lives up” - so to speak. Therefore, you will also have to wait a bit with Air Flow, since getting the composition on your lips can cause discomfort and additional irritation.
Types, types and forms of deep bite
The type of bite is determined by the level of overlap of the lower teeth:
- Mild degree.
The lower teeth are half visible.
- Average.
The lower teeth are 50–100% invisible.
- Severe degree.
The upper incisors cut into the soft tissue of the lower jaw, completely covering the lower teeth.
There are two types of deep bite:
- Distal.
This is the most common type of deep bite. With it, the lower jaw is slightly shifted back, and the lower teeth are not visible by approximately 1/3. The relationship of the distant teeth is disturbed. The patient has difficulty biting, chewing, nasal breathing, and sometimes experiences pain in the temporomandibular joint.
- Neutral.
With such a bite, the upper incisors also overlap the lower ones by 1/3, but the lateral teeth remain in place and their relationship does not suffer.
There are such forms of deep bite:
- Roof-shaped.
The upper front teeth protrude strongly forward, overlapping the lower ones.
- Blocking.
The upper incisors overlap the lower ones and are inclined backwards.
Lip level repositioning in the treatment of gummy smiles: a new approach
An attractive smile depends on the correct proportion and arrangement of three components: teeth, gums and lips. The upper lip should symmetrically show no more than 3 mm of gum, and the gum line in turn should run parallel to the contour of the lip. Excessive exposure of the gingival profile, usually called a gummy smile, provokes the visualization of excessive volume of soft tissues of the upper jaw located in the frontal area. The prevalence of this type of smile profile is used when excessive appearance of the maxillary gum occurs while smiling.
This article presents a clinical case of treatment of a gummy type of smile through lip reposition and traction of sutures placed on the levator labii muscles. A similar approach can be implemented by removing a strip of mucosa from the vestibule area of the oral cavity, thus minimizing the risk of relapse. Thanks to the combination of two surgical procedures at once, it is possible to achieve controlled traction of the levator labii muscles, thereby ensuring the achievement of a stable and aesthetically acceptable result.
Clinical case
A 25-year-old female patient was referred to the Department of Implantology at the Federal University of Santa Catarina, Brazil, with the chief complaint of excessive gingival volume exposure when smiling. The patient's general somatic history was not burdened, and there were no contraindications to the operation. Analysis of the facial profile confirmed the symmetry of all components, and the normal length of the upper lip is 20 mm. When smiling, the patient's teeth were visualized from the right first molar to the left, exposing the gum profile by 4-5 mm. Intraoral examination revealed healthy periodontal tissues with sufficient width of attached gums, as well as acceptable dimensional proportions of the teeth (Figure 1).
Photo 1. View before treatment: 4-5 mm of gingival profile exposed.
The etiology of a gummy smile is apparently related to an overactive upper lip. After discussing possible treatment approaches, the patient's consent was obtained for the lip repositioning procedure. Intervention planning began by marking future incision lines with methylene blue approximately in the middle of the visualized gingival profile (Figure 2). After anesthesia (2% lidocaine with 1:100,000 adrenaline) in the area of the vestibular mucosa from molar to molar, a “v”-shaped incision was formed not to the full depth of the tissue, 1 mm above the mucogingival junction. A second similar incision was made parallel to the first, 8-10 mm below the mucogingival junction. After connecting the two incisions, it was possible to remove a strip of mucosa, exposing the underlying connective tissue (photo 3). If minor salivary glands were present, they were also removed.
Photo 2. Planning the incision 8-10 mm apical to the mucogingival junction.
Photo 3. Connective tissue exposed.
Once the muscle fibers attached to the lip structure on both sides were identified, they were sutured, including the orbicularis oris (OO), levator labii superioris (LLS), levator labii superioris and alae nasalis (LLSAN), and zygomatic muscle (Zm), resorbable thread (VICRYL 4.0, Ethicon). The suture was started by tucking the OO muscle fibers on either side of the midline (Figure 4). Then, at the height of the lateral incisors and canines, the needle was followed from the distal to the mesial direction on both sides, thus piercing the LLS and LLSAN muscle fibers and ensuring their downward traction (Figure 5).
Photo 4. Sewing muscle fibers.
Photo 5. Sewing the muscle fibers in the area of the lateral incisors and canines.
Then, at the height of the corner of the mouth, a similar procedure was carried out with the Zm muscle fibers on the left and right sides, ensuring the same level of tension (photo 6). Therefore, after capturing the LLS, LLSAN and Zm fibers, the suture was returned to its original position by re-engaging the OO fiber region. After this, a surgical knot was formed. This approach helps maintain the lip in a more coronal position and avoid dislocation, ensuring complete immobilization (Figure 7). The second suture is provided along the trajectory already described above, including the levator labii muscles, with the formation of moderate tension (photo 8).
Photo 6. Sewing muscle fibers in the canine area.
Photo 7. At the end of the manipulation, the suture should re-pass through the central area.
Photo 8. View after suturing.
The tissue approximation in the middle part of the surgical area was carried out by suturing VICRYL 5.0 (Ethicon) using a single suture technique (photo 9). The remaining wound borders were closed with interrupted sutures (Figure 10).
Photo 9. Bringing tissues closer together to ensure symmetry.
Photo 10. Intermittent stitch for tissue stabilization.
After surgery, the patient was prescribed amoxicillin 500 mg, 3 times a day for 5 days; meloxicam 15 mg, 2 times a day for 3 days; paracetamol 500 mg, 4 times a day for 3 days; and rinse the mouth with a 0.12% solution of chlorhexidine gluconate 2 times a day for 2 weeks. The patient was also advised to apply an ice pack to her lip immediately after surgery to reduce swelling, and to avoid any mechanical impact on the upper lip area. It was also recommended to minimize lip movement whenever possible for 2 weeks. The sutures were removed 2 weeks after surgery. The patient reported mild pain and tension when smiling and speaking during the first week. A small scar was formed in the suturing area, but it was not visible when smiling (photo 11). Follow-up examination of the patient after 12 months confirmed a decrease in the visualization of the gingival profile when smiling (Figure 12).
Photo 11. View after 3 months.
Photo 12. View of a smile after a year.
Discussion
The gummy type of smile is an aesthetic problem, which is observed in a significant part of the population. Understanding the etiology of this disorder is essential to developing an adequate treatment plan. The very first technique for correcting a gummy smile was developed in 1973 by Rubinstein and Kostianovsky. In 1978, Litton and Fournier demonstrated the effectiveness of a procedure to change the attachment of muscles at the attachment to bone structures when the upper lip is too low. A more aggressive approach was described by Miskinyar in 1983, which included myectomy and partial resection of the LLS. Ellenbogen and Swara proposed a method to limit the height of lip elevation during smiling by placing a silicone seal between the muscles and the anterior nasal spine. Ronsenblatt and Simon used an elliptical incision in the area of the mucogingival junction with further separation of a partial tissue flap and removal of a strip of mucosa. Humayun described the same surgical procedure, removing, however, an elliptical strip of epithelium followed by coronal displacement of the flap. Silva modified this approach by removing two strips of mucosa from both sides of the labial cord, thereby moving the new mucosal border more coronally. Storrer developed a new surgical technique with the formation of a new contour of the gums and suturing of the muscles of the levator labii and alae nasalis. Several authors have presented case reports of successful treatment of gummy smiles in patients using the lip repositioning technique, which reduced the range of soft tissue exposure by approximately 4 mm, and the consistency of the results was confirmed over a 6-month follow-up. In 2013, Silva et al reported a case of successful treatment of a gummy smile with stable results over 2.5 years. In 70% of cases, patients rated the level of gum exposure after treatment as optimal, and more than 90% of patients were willing to repeat the procedure again. However, the results of treatment for gummy smiles reported in the literature are short-term and require more detailed analysis.
Despite this, hypermobility of the upper lip can be stabilized by implementing a specific surgical approach. To verify such a condition of the lip, it is necessary to conduct a thorough analysis of the range of e translation from the position at rest to the position during a dynamic smile. In the case described above, the patient had a hyperactive lip with 4-5 mm of gingival profile exposed. The lip position was stabilized by traction of the muscles responsible for the formation of the smile profile (OO, LLS, LLSAN, Zm). This technique was first described by Saba-Chujfi, and allows achieving a stable treatment result without relapse of the lip position for at least 1 year. In addition, when using this technique, it is possible to avoid such surgical complications as the formation of a mucocele, the occurrence of paresthesia and transient muscle paralysis. To achieve the desired treatment results, it is necessary to carefully approach the diagnosis of aesthetic disorders, and the selection of appropriate clinical cases, according to the indications, suitable for a particular surgical approach.
A good understanding of the anatomy, topography and function of the levator labii superioris muscles is one of the success factors for such iatrogenic intervention. Contraindications for lip reduction surgery include inadequate width of attached gingiva, which makes it difficult to achieve proper flap separation and further stabilization after suturing; excessive height of exposure of the tissues of the upper jaw (> 8 mm) - in such cases, an interdisciplinary approach, including orthognathic, orthodontic and periodontal stages of treatment, is simply impossible.
As for the suturing technique, loop sutures allow stabilization of the muscle bundle on both sides of the surgical site. The direction of the sutures influences the degree of immobilization of the lip while maintaining symmetrical balance, limiting upward movement of the lip during smiling.
conclusions
This clinical case describes a procedure for predictive treatment of a gummy type smile. The combined technique of traction of the muscles of the levator labii superioris using loop sutures ensures the achievement of a good aesthetic result, the stability of which has been confirmed over 1 year. To further substantiate the effectiveness of this technique, it is necessary to conduct additional clinical studies on a larger sample of dental patients.
Authors: Gustavo Javier Salazar Littuma, DDS, MSc Humberto Cherem Mendez de Souza, DDS Gabriella Mercedes Peñarrieta, DDS, MSc Ricardo de Souza Magini, DDS, MSc, PhD Eduardo Saba-Chujfi, DDS, MSc, PhD
Correction of distal bite
Deep bites can be corrected surgically and non-surgically. The second option involves orthodontic and orthopedic treatment. First, the lateral teeth are pushed forward, then the inclination of the incisors is leveled. If desired, the patient can resort to orthopedic treatment - installation of veneers, onlays, crowns.
With any type of treatment, a complete sanitation of the oral cavity is first carried out - all infectious processes are eliminated, caries is treated, tartar is removed, etc. If this is not done, the patient will face complications in the form of caries and periodontal disease. The dentist also explains in detail to the person the importance of home hygiene. If it is insufficient, these complications may also occur.
Treatment of deep bite in childhood
This correction can be carried out from the age of 7 years. At this age, the child develops a mixed bite, the bone tissue is still unstable, and the teeth are more susceptible to the effects of the braces system. Orthodontists also resort to installing removable plates.
It is also important to eliminate the cause of the pathology. For example, if a distal bite has formed due to the habit of thumb sucking, but it has not been eradicated, even after comprehensive treatment a relapse may occur. If the orthodontist discovers such a problem, then first of all he refers the child to a psychologist, since most often such habits are a consequence of stress.
Treatment of deep bite in adults
Mature people with this pathology have braces installed. At the same time, the position of the teeth is changed so that the chewing load is evenly distributed between them.
Reference!
With a distal bite, an overlap of the lower teeth by 1/3 would be considered a good result.
The next option is the installation of an orthopedic structure: veneers, onlays or crowns. The main disadvantage of this procedure is the likelihood of severe grinding of the teeth and injury to the pulp.
Another technique is a combination of the previous two methods. First, the teeth are orthodontically prepared, and then orthopedic restoration.
Orthognathic surgery
This treatment option is appropriate for severe cases of distal malocclusion. Surgery can reduce or increase the size of the jaw. It is also important to undergo treatment with an orthodontist before surgery. This period takes from one year to one and a half years.
The operation is performed under general anesthesia. The patient is observed in the hospital for several days, then walks with installed intermaxillary traction for another 6 weeks. After recovery, the second stage of orthodontic treatment follows, which, on average, lasts from a couple of months to six months.
Treatment of distal occlusion in temporomandibular joint dysfunction
First, the masticatory muscles are relaxed with muscle relaxants and a bite block. After this, the bone is fixed in a central position. Next, direct treatment is carried out. If the patient wishes, veneers or crowns can be installed.
How are lip contouring and teeth related?
Every year, a cosmetic procedure such as lip contouring is gaining more and more popularity. The procedure is now quite affordable and every girl or woman can afford to try it. With the help of lip surgery, you can correct their contour, increase their volume and change their shape.
The contouring procedure itself is safe; the main thing in this matter is to find a good cosmetologist who uses only certified and high-quality materials in his work.
Having decided to change the shape of their lips, most girls do not think about their teeth at that moment. But in vain!
After all, as soon as lip contouring is done, the gaze of strangers and especially close friends and family will be directed at the lips, which means that the teeth will automatically fall into the zone of attention. Therefore, before going to the cosmetologist, look in the mirror, study yourself and your teeth, imagine how your “new lips” will combine with your teeth, what your smile will look like, so that you don’t end up with plump lips, but cannot smile.
So, let's look at several possible options for what could happen to your teeth, and in what order to carry out procedures at a cosmetologist and dentist.
What happens if you don't correct a deep bite?
Complications of uncorrected deep bite:
- loosening of incisors,
- cracks and chips on the front teeth,
- abnormally rapid and uneven wear of enamel (especially lateral teeth),
- sensitivity of the anterior incisors to cold and food,
- gradual protrusion of the upper incisors,
- wedge-shaped defects.
Such defects appear due to the strong pressure of the lower front teeth on the upper palate.
There are also complications that do not directly affect the condition of the teeth:
- Trauma to the mucous membrane of the palate.
Constant friction of the lower incisors against the upper palate provokes persistent wounds. But the mucous membrane must constantly renew itself, which is why an excessive number of new cells appear. This, in turn, increases the risk of mutations and cancer.
- Disorders of the temporomandibular joint.
The patient can move the jaw limitedly, the muscles are stiff. People often experience pain in this area, hear crunching or clicking noises when chewing, and suffer from migraines. If this is not corrected, over time the patient will experience degenerative processes in the joint.