The tongue is often injured. Sometimes these damages are so insignificant that we do not notice them, but these mucosal defects are the entry point for infection. Glossitis is an inflammation of the tongue that is caused by various bacteria and viruses. The disease causes a number of unpleasant symptoms that interfere with normal eating, and sometimes even interfere with talking. Glossitis is dangerous due to its complications. If measures are not taken in time, diffuse purulent inflammation may occur, spreading far beyond the oral cavity.
The disease is very common. Most often occurs in people with reduced immunity, smokers, and patients who do not pay due attention to oral hygiene.
Forms
Types of glossitis:
- deep;
- desquamative;
- diamond-shaped;
- villous;
- folded;
- Gunter's;
- syphilitic or interstitial.
The most dangerous is deep glossitis. The pathological process begins on the lower part of the tongue, and if left untreated, spreads to the floor of the oral cavity. In the case of abscess formation, the purulent process can spread to the neck, which is a life-threatening condition.
Desquamative glossitis is better known as “geographic tongue.” Irregularly shaped areas of peeling alternate with normal ones, so the tongue looks like a geographical map. This type of disease is typical for patients with chronic lesions of the digestive system, allergies, helminthic infestations, and can also occur during pregnancy.
Diamond-shaped lesions are typical for patients with chronic gastropathology. The disease is recurrent.
Villous glossitis occurs due to hypertrophy of the papillae of the tongue. This disease is one of the manifestations of a fungal infection - candidiasis, and can also occur in smokers.
The disease may be congenital. Such anomalies include a folded shape. This glossitis does not cause unpleasant symptoms and does not require special treatment.
Gunter's tongue is not an independent pathology, but one of the manifestations caused by anemia resulting from a lack of vitamin B 12 and folic acid in the body. The disease develops gradually. The mucous membrane of the tongue becomes smooth, the papillae decrease in size, and the tongue acquires a crimson hue.
Interstitial glossitis is also a secondary manifestation and is characteristic of patients with syphilis. The pathological process proceeds deeply, affecting muscle tissue. If left untreated, the muscles are replaced by connective tissue, which is an irreversible process. This form can transform into a malignant tumor.
Having seen photos of glossitis of different etiologies, you can be convinced that the clinical symptoms of this disease are varied, so only a specialist can make a differential diagnosis.
Glossitis of the tongue can be either an independent disease or one of the clinical symptoms of another pathology. For proper treatment, it is necessary to find out whether the disease is a primary inflammatory process, or arose as a result of changes in other organs and systems.
Epidemiology
The only source of infection is a person infected with this virus. The most dangerous are those who do not have any clinical manifestations: virus carriers are the main source of the spread of HIV infection among the population.
During a dental appointment, infection can occur in the following cases:
- when using medical instruments contaminated with blood or other biological fluid that have not been disinfected (various devices, discs, burs, probes, needles, syringes, cutting and piercing instruments, etc.);
- in the presence of wound surfaces and ulcerations in the oral cavity;
- in case of extensive contamination of the skin of healthcare workers with blood, blood getting into the eyes;
There are known examples of infection during acupuncture treatment.
(There is no airborne transmission of infection.)
The immunodeficiency virus is found in the highest concentration in the blood. Next in descending gradation are sperm, vaginal and cervical secretions of the glands, breast milk, and saliva. Blood and other specified biological fluids are factors in the transmission of HIV from an infected person to other persons.
The virus is moderately resistant outside the human body. In the external environment (biosubstrates), its infectious effect lasts up to 2 weeks, in a dried state (discharge on linen, objects, etc.) - up to 1 week. Radiation exposure and ultraviolet rays do not affect it. When boiled, the virus dies within 5 minutes; when heated to 56°C, inactivation occurs after 30 minutes. Disinfectants used in the practice of medical institutions (chloramine, calcium hypochloride, hydrogen peroxide, alcohol, etc.) in concentrations provided for the disinfection of hepatitis viruses are guaranteed to destroy HIV upon direct contact of the disinfectant with contaminated blood or other human biological fluid on the surface of an object, including a hollow one ( internal surfaces of the syringe, needles, capillaries, probes, etc.).
Causes of glossitis
Glossitis occurs under the influence of provoking factors. The most common of these is damage to the mucosa. Damage can occur due to the consumption of hard, spicy, hot foods. Often the tongue is injured by crowns, tooth fragments, braces or improperly made removable dentures. For infection to penetrate, a microscopic defect is sufficient, which does not cause discomfort and is visually invisible.
The source of infection in the oral cavity increases the likelihood of inflammation during injury. These include carious teeth, gum inflammation, stomatitis, and chronic tonsillitis. Failure to comply with hygiene rules, using someone else's utensils, toothbrushes, and dirty hands while eating increase the risk of infection entering the oral cavity. Children who can put dirty hands and foreign objects into their mouths are at particular risk.
Smoking and alcohol reduce local immunity and make the mucous membrane more vulnerable. In this group of patients, glossitis occurs more often than in other people.
Constant exposure to chemicals that destroy the mucous membrane eventually leads to chronic inflammation. Glossitis can even be caused by poor-quality toothpaste or mouthwash.
Dysbacteriosis, carriage of the herpes virus, reduced immunity are predisposing factors in the occurrence of glossitis.
Bacterial infections
Ulcerative-necrotizing gingivitis develops in HIV-infected individuals both during various periods of clinical manifestations of AIDS, and without them in the presence of antibodies against the virus. Patients complain of pain and bleeding gums while brushing their teeth and eating; bad breath. Upon examination, a gray-yellow plaque (necrotic film) is found covering the gingival margin and interdental papillae. The mucous membrane in the gum area is hyperemic, swollen, and tense.
After treatment, the symptoms disappear, but there is a tendency to relapse. A prolonged course can lead to deep ulcers with damage to bone structures and necrotization of the interdental septum (Fig. 4).
Rice. 4. Herpes simplex on the lip.
The consequence of gingivitis is periodontitis (periodontitis) with irregular generalized destruction of bone tissue and the supporting-retaining apparatus of the tooth. Treatment of patients does not provide lasting results.
Clinical manifestations
The first thing those suffering from glossitis encounter is pain, burning, and severe discomfort in the oral cavity. Over time, the intensity of these manifestations increases, making it difficult to eat food. Taste sensations are dulled and may be completely absent. Some patients have a phenomenon called perverted taste.
The tongue swells, which causes severe discomfort. The patient's speech is impaired, any movements of the tongue bring pain. Hyperthermia and deterioration in general health are possible.
Upon examination, you can reveal an enlargement of the tongue, a change in its color to a brighter one, up to crimson. Ulcers, blisters, spots, erosions, plaque, and lesions with altered epithelial structure may appear on the mucous membrane.
The most dangerous complication of glossitis is phlegmon. A focus of purulent inflammation is formed, which rapidly spreads to the chin and neck. Soft tissues are destroyed. Such patients require emergency medical care.
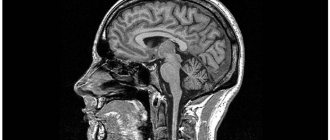
Anatomy of the tongue
The tongue is divided into: body, apex and root. The tongue consists of muscles and is covered with epithelium. Also on the back of the tongue there are many special papillae with which we feel taste. The largest grooved papillae are located closer to the root of the tongue. In the center of the tongue there are filiform papillae, on the sides there are leaf-shaped papillae. And in front of the tongue there are mushroom-shaped papillae.
Diagnosis and treatment methods for glossitis
In most cases, the basis for diagnosis is the patient’s complaints and visual examination of the oral cavity.
When visiting a doctor, be sure to indicate when the pathological manifestations appeared and what they are associated with. If any dental treatment was performed, be sure to mention it. It is better to seek medical help at the first signs of illness. Avoid taking any medications, especially antibiotics. This may make diagnosis difficult and reduce the effectiveness of subsequent therapy.
To determine the cause of glossitis, additional diagnostic methods are used: examination of scrapings from the mucous membrane under a microscope, ELISA, PCR. These methods make it possible to determine what pathogen caused the disease, as well as to confirm or exclude syphilitic glossitis.
Determining the causative agent of the disease is the basis for successful treatment. The emphasis is on etiotropic therapy, that is, eliminating the cause of the disease. If glossitis is bacterial in nature, properly selected antibiotics will give an excellent result, but these drugs are completely useless for viral or candidal glossitis. For fungal infections, antimycotic drugs are prescribed; for viral infections, antiviral and immunomodulators are prescribed. If the cause of glossitis is anemia, treatment of the underlying disease is necessary. Special tactics are necessary for the pathological process caused by Treponema pallidum. A dermatovenerologist must be involved in the treatment of syphilitic glossitis.
An integral part of glossitis treatment is diet. In the acute period, eating food causes serious difficulties for patients, so porridges, purees, and pureed soups are recommended. Food should not be cold or hot. Solid foods, spicy, salty, sour are excluded. This avoids irritation of the mucous membrane, which minimizes discomfort and speeds up the healing process.
In some patients, the pain syndrome is significant. In such a situation, unpleasant sensations can be relieved with the help of applications with anesthetics. To moisturize excessively dry mucous membranes, products containing glycerin are used.
Local therapy includes removing plaque from the tongue and treating with antiseptic solutions. Substances such as chlorhexidine, furacilin, and potassium permanganate are widely used. To speed up the recovery of the mucous membrane, vitamin A is used topically.
Systemic antibiotics and antiviral drugs are prescribed according to indications. This tactic is used in severe cases. With a mild clinical course of glossitis, a positive result can be achieved with local treatment.
In severe cases, swelling of the tongue can be significant and make breathing difficult. In such situations, it is necessary to take glucocorticosteroids. More often they are used in the form of ointments.
During treatment you need to give up smoking and alcohol. These substances irritate the mucous membrane and prevent its regeneration.
Some patients with glossitis have keratinized areas on the tongue. Such changes cannot be treated conservatively and can only be removed surgically.
If you consult a dentist in a timely manner and follow all his recommendations, the outcome of the disease will be favorable. Glossitis responds well to treatment if its cause is determined and targeted. If the disease is not treated, it can be complicated by an abscess or phlegmon. These conditions require surgical treatment and long-term antibiotic therapy, so it is better to start treatment at the initial stage.
Viral infections
In HIV-infected people, the most common manifestations of stomatitis are caused by the herpes simplex virus. Primary infection with the herpes virus occurs in children, adolescents, and, less commonly, young adults. Since the infection is latent, there is a tendency to recur, and manifestations can be both general (fever, pain when swallowing, swollen lymph nodes) and local. Acute herpetic rashes can be localized in any part of the maxillofacial area. Favorite places are lips, gums, hard palate. The initially small bubbles that form then merge into larger ones. After the destruction of the tire, the underlying tissues tend to ulcerate. In the oral cavity, the bubbles burst very quickly, and usually erosion is immediately detected. On the red border of the lips, the vesicles of the blisters shrink, forming dry or weeping crusts.
The herpes virus can cause generalized lesions up to and including herpes encephalitis.
Recurrent herpetic stomatitis is most often localized on the red border of the lips with the involvement of surrounding areas of the skin. The blisters quickly enlarge, merge, and a secondary infection develops. The contents of the blisters suppurate, resulting in the formation of crusts of a dirty yellow color; after their separation, an eroded or ulcerated surface is exposed (Fig. 5).
Rice. 5. Viral wart.
The lesions on the hard palate and gums are represented by small bubbles that quickly burst, leading to ulcerative lesions of the mucous membrane. Clinical manifestations can be triggered by a cold, stress, or respiratory infection (Fig. 6).
Rice. 6. Hairy leukoplakia on the lateral surface of the tongue.
Shingles (herpes zoster) in the oral cavity and on the face is characterized by asymmetry of the lesion according to the area of innervation of one of the branches of the trigeminal nerve. It is also possible that two or three branches of trigeminus are involved, when elements appear on the mucous membrane in the form of small blisters and then an ulcerated surface. The rash is preceded by burning pain, simulating pulpitis of intact teeth, radiating along the maxillary or mandibular branch of the fifth pair of nerves. These pains may persist even after involution of the lesions (up to 1–2 months).
Viral growths come in the form of warts, papilloma, genital warts and frontal epithelial hyperplasia (papules or nodular lesions with filamentous growths).
Warty formations are localized in the corners of the mouth. They may have the appearance of a papilloma, ridge, or protrusions (Fig. 7).
Rice. 7. Hairy leukoplakia of the ventral and dorsal surface of the tongue.
Genital warts. Depending on the location, the lesion elements can have different appearances: multiple pointed protrusions or rounded, slightly raised areas with a flat surface. When localized on the gum or hard palate, the lesions appear as multiple pointed projections. When located on the cheeks and lips, the elements have a picture similar to focal epithelial hyperplasia: rounded, slightly raised areas with a diameter of about 5 mm with a flattened surface.
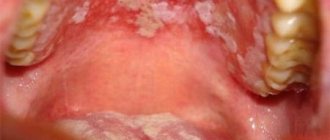
Hairy leukoplakia. The lesion is localized, as a rule, on the tongue, having different sizes and appearance. It is found in limited areas of the lateral, dorsal, ventral surface or covers the entire tongue. The mucous membrane takes on a whitish appearance, but hyperkeratosis does not develop. On palpation, the seals are not detected, which served as the basis for designating this form of lesion: soft leukoplakia (Fig. 8).
Rice. 8. Kaposi's sarcoma on the skin of the face.
On the lateral surface of the tongue, elements can be located bilaterally or unilaterally (Fig. 9). The mucous membrane, over a limited or widespread area, becomes irregular and rises in the form of folds (“corrugated”) or projections above the surrounding surface, which may resemble hair in appearance. Hence the name - hairy leukoplakia.
Rice. 9. Kaposi's sarcoma on the palate.
On the lower surface of the tongue, the focus of epithelial opacification may be smooth or slightly folded. Much less commonly, soft leukoplakia occurs on the cheeks, floor of the mouth, and palate.
There are no subjective sensations other than discomfort.
Hairy leukoplakia can be combined with candidal glossitis, confirmed by laboratory methods. However, treatment of candidiasis does not affect the appearance of the lesion.
Histological, virological, including serological, studies give reason to believe that the cause of soft hairy leukoplakia is the Epstein-Barr virus.
Soft leukoplakia must be differentiated from leukoplakia, lichen planus, chemical or electrical burn, and chronic hyperplastic candidiasis.
Prevention
Glossitis is easier to prevent than to treat. In order to avoid this unpleasant disease you need to follow simple rules.
The first is oral hygiene. This principle applies to both children and adults. If you wash your hands before eating, brush your teeth regularly, do not use someone else’s toothbrushes, and regularly sanitize your mouth, then the risk of developing tongue inflammation is minimal.
Try to avoid damaging the mucous membrane. Avoid eating hard foods that can damage your tongue, such as chips. Hot foods also cause epithelial defects. Spicy foods have an irritating effect. Abuse of them significantly worsens the condition of the tongue mucosa and increases the risk of infection.
Nicotine not only irritates the mucous membrane, but also impairs microcirculation, which reduces the resistance of the epithelium to the effects of infectious agents. Inflammatory diseases of the oral cavity are more common in smokers than in patients who are not adherents of this addiction. Strong alcoholic drinks also have a negative effect on the mucous membranes.
If you have symptoms of glossitis, do not self-medicate, contact a dental clinic. A competent specialist will determine the cause of the disease and prescribe treatment that will help quickly get rid of unpleasant symptoms. Remember, if glossitis is not treated, the disease can lead to serious complications and irreversible consequences.
As a sign of disease
The tongue is a kind of mirror of the work of the whole organism, therefore desquamative glossitis manifests itself as one of the symptoms of other diseases. These include:
- disruption of the gastrointestinal tract, liver, gall bladder;
- lack of B vitamins;
- unhealthy diet, dysbacteriosis;
- helminthiases;
- dermatoses;
- autoimmune diseases;
- acute infectious diseases such as typhoid or scarlet fever;
- some disorders of the hematopoietic system;
- abuse of drugs (and especially antibacterial) drugs.
In some cases, desquamative glossitis is hereditary.