General information
As such, the medical term “pimple on the tongue” does not exist.
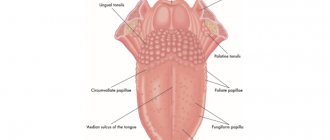
Rather, it is a collective term in everyday spoken language, reflecting the appearance on the tongue of adults and children of formations (swellings, tubercles, nodules, vesicles) of various origins. Depending on the reason for their appearance, they can be of different colors (red, white, yellow, pink). Often, such pimples appear in other parts of the oral cavity: on the palate, on the mucous membrane of the mouth, on the lip, and often there is a pimple on the gum above the tooth. Less common is a blister filled with pus on the gum (purulent pimple on the gum). In a healthy person, the mucous membrane of the tongue is normally pale pink in color, and the papillae are slightly pronounced. The bulk of the tongue is made up of muscular striated tissue, intertwined in three perpendicular directions, between which there is connective tissue in which blood vessels and nerve fibers pass.
It should be noted that changes in the oral mucosa and the immediate condition of the papillae of the tongue (size, plaque on it, color) are often a kind of indicator of impaired functioning of the body, and most often the presence of pimples on the tongue is one of the signals of the appearance of certain problems (mainly from the gastrointestinal tract), vitamin deficiency . Such phenomena may also indicate the appearance of diseases such as glossitis , stomatitis , an allergic reaction , vitamin deficiency , infectious diseases, for example, with scarlet fever , when the tongue becomes crimson in color and the papillae on the tongue increase sharply.
However, the appearance of pimples on the tongue is not always caused by a disease. They are often the result of mechanical trauma from eating solid foods (crackers, chips, seeds) or the manifestation of a local allergic reaction to any foods or medications/oral care products. Pimples in the mouth in adults often cause discomfort to the patient, can be painful, and interfere with eating and talking. Let us consider below why they appear, what they are like and what to do when they appear.
Preventive measures
It is easier to prevent a disease than to eliminate it over a long period of time. In this regard, it is necessary to adhere to the following medical instructions for the prevention of rashes on the surface of the tongue :
- following oral hygiene rules (high-quality toothpaste, toothbrush);
- refusal of salty, spicy, hot, solid foods;
- use of vitamins;
- cessation of smoking and alcoholic beverages;
- constant physical activity;
- timely visit to the dentist.
By following these recommendations, you can prevent the onset of the disease and other adverse consequences.
A rash on the surface of the tongue that does not disappear on its own after several days must be cured. Initially, you need to find out the recommendations of a specialist. He conducts an examination, appropriate examination and prescribes medications. An advanced inflammatory process in the oral cavity is fraught with complications.
What diseases will the condition of the surface of the tongue tell about:
Pathogenesis
The pathogenetic mechanisms of the development of various types of formations on the tongue are based on different processes - proliferative inflammation, dystrophies, tumor processes, sensitization of the body (specific/nonspecific) and allergic manifestations, injuries to the mucous membrane of the tongue, causing morphological, biochemical and functional disorders in the tissues of the tongue. Accordingly, the basis of morphological changes/reactions of tongue tissues is the reproduction/transformation of cellular structures, promoting the formation and proliferation of granulation tissue structures, atypical hyperplasia of the epithelial mucosa, which is manifested by the formation of granulomas , tubercles , nodules , vesicles and their necrotic changes of varying severity, characteristic of those or other diseases of the body and oral cavity, in particular.
How to avoid what is predicted in omens
A pimple on the tongue, even regardless of superstitions, is an unpleasant thing, and taking into account popular beliefs, the mood deteriorates even more. To prevent a sign from coming true, it is usually enough:
- after paying attention to the pimple, really talk less about personal topics, watch your tone;
- if the pimple hurts a lot, in addition to the usual measures to eliminate unpleasant sensations, it is useful to ask for forgiveness from those who were allegedly recently offended;
- It is enough for non-superstitious people to leave the pimple unattended.
An alternative method, universal for all bad omens: as soon as an undesirable sign is noticed, you must say “mind me” and, if desired, spit over your left shoulder.
Important! If the pimple hurts for a long time, the redness spreads, it is better to consult a doctor. Inflammations should be treated before they spread.
An incident occasionally signals the need to pay attention to the atmosphere in the family; perhaps decisive measures should be taken to mitigate “small” conflicts and contradictions
Classification
As such, there is no classification of formations in the tongue, since their appearance is influenced by numerous exogenous/endogenous influence factors. Some authors classify these phenomena from an etiological point of view, and therefore distinguish several groups:
- Formations in the tongue of traumatic origin - acute and chronic mechanical trauma of the tongue, chemical trauma, physical factors (high/low temperatures).
- Formations on the tongue caused by local/general infection. Infectious agents in the oral cavity are often various strains of viruses ( adenovirus , retrovirus , herpes simplex virus , measles virus , HIV ), staphylococcus , streptococcus , fungi , fusospirillum .
- Formations in the tongue associated with sensitization of the body/disorders of immune processes. Such formations are based on the presence of reactive zones on the oral mucosa that react in a certain way upon contact with allergens of various origins (toxins, foods, drugs, etc.), contributing to the development of autoimmune reactions.
What to do
The human oral cavity is home to many bacteria, both beneficial and pathogenic. They have both negative and positive effects on the human body. Pathogenic bacteria cause inflammatory processes, including glossitis, or inflammation of the tongue. Often patients notice a white pimple that reacts with pain to every touch. In fact, this is not a pimple, but an inflamed nodule. In medicine, such inflamed nodules are called glossitis.
A transparent pimple under the tongue can occur as a result of mechanical damage or as an allergic reaction to chemical and food irritants.
You can get rid of glossitis only through comprehensive measures. The first step is to consult a doctor to determine the true cause of its occurrence. The oral cavity should be kept clean, preferably rinsed with a soda solution or a decoction of St. John's wort. It is also necessary to strengthen the immune system and limit the consumption of spicy and too hot foods so as not to irritate the inflamed nodule.
Causes
The causes of pimples on the tongue are quite diverse and can be both local and general. The main reasons include:
- Mechanical/chemical damage of various origins (shards of fillings, sharp edges of teeth, low-quality metal crowns, hot/cold food, dentures). These are predominantly formations on the tip of the tongue or on the side.
- Insufficient/improper oral hygiene care.
- Exposure to infectious agents (bacteria, viruses and fungi), which can, under some conditions, cause inflammation and red pimples on the tongue closer to the throat.
- Uncontrolled long-term use of antibacterial drugs.
- Bad habits: smoking and abuse of alcohol-containing drinks, which irritate the oral mucosa.
- Hypo / vitaminosis (lack of vitamins (B6, PP, B12, A, E) and iron, accompanied by an increase in the papillae of the tongue (red papillae over the entire surface of the tongue).
- Diseases of the gastrointestinal tract ( gastritis , gastric ulcer , hepatitis , cholecystitis , chronic colitis . Formations are located at the root of the tongue, that is, closer to the throat.
- Endocrine disorders: hypothyroidism , diabetes , menopause .
- Candidal single lesion of the oral mucosa (white pimple on the side of the tongue).
- Allergy to prosthetic material (usually acrylic structures containing methacrylic acid ester).
Location: at the tip
A white pimple on the tip of the tongue can appear at the site of a microtrauma as a result of an infection entering the wound. Fans of chips, seeds, pistachios and other nuts are especially susceptible to developing pimples on the tip of the tongue. Solid foods scratch the delicate tip of the tongue, causing pathogenic bacteria to enter the wound, causing it to become inflamed and painful.
Often a pimple occurs due to an exacerbation of the herpes simplex virus against the background of decreased immunity. In this case, strengthen your immune system and take vitamin complexes. But in any case, consult a doctor and get tested to make an accurate diagnosis.
Also, a pimple can pop out due to chronic stomatitis. If the patient has a weakened immune system and has carious teeth, persistent infection in the oral cavity sooner or later leads to stomatitis. Without timely treatment, it can become chronic, periodically exacerbating.
Symptoms
They manifest themselves by the appearance on the tongue, and often on the oral mucosa, of formations of various colors, shapes and sizes, resembling pimples in appearance (photo below).
They can be either painless or accompanied by pain, especially when swallowing and talking. Less common are redness of the tongue, burning, swelling, increased salivation, and impaired motor function of the tongue/speech. However, in any case, their appearance causes discomfort.
Pimples appeared on the tongue: treatment at home
Having determined the nature of the rash, the doctor can prescribe a comprehensive treatment of the disease (drug and herbal treatment) or non-drug treatment at home. Pimples on the root, tip, and near the frenulum of the tongue can be removed using folk remedies.
Herbal medicine
Herbal decoctions and infusions effectively remove pimples both on the tip and at the base of the tongue. The most effective rinses are chamomile, St. John's wort, and calendula. Herbal decoctions are especially effective when the rashes are inflamed.
Method for preparing the decoction: pour a teaspoon of herbs into a glass of boiling water, leave for about 15 minutes, and cool. You need to rinse your mouth 2-4 times a day.
Infusions and decoctions can be taken orally, this will help alleviate the symptoms of the disease, relieve inflammation, and help stabilize metabolic processes.
Compresses and lotions
If the formations are inflamed, pain and inflammation can be relieved by applying a cotton swab moistened with a herbal decoction of chamomile and calendula to the affected surface.
You can numb the surface of the tongue using therapeutic and prophylactic toothpaste, which is applied for 2 minutes. The paste relieves pain, has a calming, anti-edematous and anti-inflammatory effect.
Rinsing with antiseptic solutions
They help treat inflammation of the mucous membrane, eliminate tubercles on the tongue both at the very beginning and closer to the throat. In the fight against the disease, the use of Chlorophyllipt and Chlorhexidine is common. The preparations can be used as rinses and are effective for irrigating the oral cavity. Procedures are carried out several times a day.
Tests and diagnostics
The diagnosis is made based on examination of the oral cavity and patient complaints. If necessary, laboratory and instrumental examinations are carried out:
- Bacterioscopic examination - scraping from the mucous membrane of the tongue and microscopy of Gram-stained smears.
- Bacteriological examination (culture of material from the oral cavity on nutrient media).
- Analysis of saliva for the presence of an infectious agent.
- Blood sugar test.
- Clinical/biochemical blood test
- If necessary, gastroscopy, ultrasound of the abdominal organs to identify gastrointestinal diseases.
In children
Dental diseases in a child are determined not only by the presence of pain in the mouth, but also by the appearance of painless rashes on the mucous membrane, which parents call “pimples.” Pimples in a child's mouth are actually inflammatory swellings, bumps, watery blisters or nodules that are not pimples. The oral mucosa is very sensitive to various influences, so even a slight provocation causes inflammation. It could be:
- unbalanced diet;
- weakening of protection after illness;
- changes in intestinal microflora;
- activation of opportunistic oral flora.
Any changes in the oral cavity are a signal from the body that you need to pay attention to. On the one hand, the appearance of rashes may indicate pathology of internal organs or dental diseases. On the other hand, a favorable environment for the proliferation of microorganisms in the mouth can lead to the fact that a minor crack, in the absence of treatment and hygiene, quickly becomes inflamed and suppurates. With the participation of various microorganisms in the mouth, various dental diseases develop in children - most often they are caused by streptococci, fungi, and staphylococci. Also, do not forget about changes in the oral mucosa during infectious diseases ( influenza , measles , scarlet fever , chicken pox , infectious mononucleosis , fungal infection).
It makes sense to consider a common disease in children, which is accompanied by the appearance of various elements on the oral mucosa. Stomatitis is the most common cause of the appearance of elements on the tongue and gums that look like pink or red pimples. The main cause of this disease is the introduction of bacteria to the mucous membrane with dirty hands and toys, unwashed fruits and berries. Small, painful pink or red formations appear on the surface of the tongue. The pain intensifies when eating, talking and swallowing saliva. If the process is not eliminated at this stage, a superficial defect of the mucous membrane of a round or oval shape develops - aphtha ( aphthous stomatitis ). It is covered with a coating of fibrin, which gives it a white or yellowish tint. The edge of the aphtha is surrounded by a red rim.
Red formations on the tongue are a sign of inflammation of the tongue ( glossitis ). Outwardly, they can be mistaken for inflamed pimples. As a result of a burn from hot tea or food, the papillae of the tongue become enlarged and painful, so they can be mistaken for pimples.
In chickenpox, this element is a vial of liquid. The accumulated fluid raises the stratum corneum. The blisters in the mouth quickly burst and small round grayish erosions are formed, which externally resemble aphthae covered with crusts. Chickenpox rashes appear with a difference of 1-2 days, so the elements will be at different stages: papules, vesicles, and then crusts. Also, blisters form with herpetic lesions of the mucous membrane, enterovirus infection and Dühring's dermatitis herpetiformis.
With infectious mononucleosis, enlarged mushroom-shaped papillae appear on the tongue, which are mistaken for pimples. With influenza, catarrhal stomatitis , which involves the soft palate, arches, uvula, cheeks and tongue. Against the background of catarrhal changes, rashes appear like red millet grains. The white dots in the baby are associated with the glandular nodules of Bon - these are the rudiments of the salivary glands located on the soft palate. They usually resolve on their own. White pimples appear with candidiasis - outwardly they look like cheesy layers on the tip of the tongue and under the tongue.
Treatment of pathological formations on the oral mucosa in a child
- An important condition for treatment is the elimination of irritating factors. The child should not be given salty and sour foods, juices, and rough food is not allowed. During illness, food should be pureed (porridge, mashed potatoes, mashed soup, soufflé, pureed cottage cheese), liquid (milk, cream, sweet tea, cocoa).
- Local treatment includes oral care - rinsing with herbal decoctions and antiseptics after each meal and at night. You can use a decoction of sage, chamomile, and calendula. Calendula tincture, 1 teaspoon per glass of water, can be used, which has an antimicrobial and anti-inflammatory effect. For rinsing in children, you can use a solution of Miramistin , Chlorhexidine , an alcohol solution of Citral (25 drops per 0.5 glass of water), a solution of furatsilin , Hydrogen Peroxide (2 tbsp. L per 0.5 glass of water), Stomatofit Fresh , an alcohol solution of Chlorophyllipt ( 1 tsp per 0.5 cup of water), Hexoral , Rotokan , Angiosept . These procedures prevent secondary infections and more serious complications.
- Most diseases of the mucous membrane are of inflammatory origin, therefore, locally, in addition to rinsing, irrigation with antiseptics in the form of a spray is prescribed ( Stopangin , Kollustan , Ectericide with chlorophyllipt , Rotocan-Vialine ). Older children can dissolve tablets or pastes ( Strepsils , Ingalipt Vialine Ingaliptum Ultravirk paste , Faringosept , Gramicidin , Neo-Angin ).
- For severe pain, local anesthetics are used. An alcohol solution of propolis (4-20%) in addition to having an antimicrobial effect, also has an analgesic effect. For topical anesthesia, propolis tincture is used with oils (peach, sea buckthorn, rosehip) or glycerin: take 4 drops of tincture and 10 drops of oil. A decoction of mint leaves as a gargle can also be used as a pain reliever. For pain, enveloping decoctions of flax seed and marshmallow root are used.
Treatment of pimples on the tongue
Carrying out an examination of the mucous membrane of the tip, side, and root of the tongue, the doctor examines the red pimples and growths. Based on laboratory tests, examination and medical history, the specialist makes a diagnosis, finds out why the disease appeared, and determines the therapeutic direction. The classic method of treatment is medication:
- Antibiotics are used to destroy bacteriological pathogens
. Effective drugs for local action: Bioparox, Fuzafyungin. As well as medications for systemic treatment: Amoxicillin, Cefadroxil. - To prevent the rashes from becoming inflamed, anti-inflammatory drugs are prescribed: Stomatidin, Ingalipt, Lugol.
- Antiseptic agents accelerate wound healing: Chlorhexidine (it is necessary to apply lotions and rinses).
- Dysbacteriosis, which can cause rashes on the mucous membranes, is treated with probiotics: Bifidumbacterin, Acipol, Linex, Bifiform.
- If pimples appear on a baby's tongue, they are often caused by fungal infections; thrush is treated with antifungal drugs
. It is worth doing daily rubbing of the tongue, cheeks and lips with a broad-spectrum solution of Candide. After just 1–2 days, less plaque forms, and after a week, the signs of the disease completely disappear. - Allergic reactions are eliminated with the help of antihistamines: Fenistil, Cetrin, Erius.
Diet
Diet Table No. 1b
- Efficacy: therapeutic effect after a week
- Terms: 10-30 days
- Cost of products: 1100-1200 rubles per week
Diet Table No. 1
- Efficacy: therapeutic effect after 3 weeks
- Terms: 2 months or more
- Cost of products: 1500 - 1600 rubles. in Week
Until complete recovery, you need to avoid hot, spicy and sour foods and drinks. Avoid rough foods that injure the mucous membranes of the tongue, gums and cheeks (chips, crackers, nuts, overcooked potatoes, meat and fish). The quality of the diet can remain the same, but all dishes should be pureed or soft to reduce trauma to the mucous membrane. In nutrition, you can focus on Table No. 1b and Table No. 1 , followed by a transition to normal nutrition.
Signs about acne on other parts of the face
Besides the tongue, a pimple can be located anywhere. Each location has its own interpretation.
Pimples on the chin usually have a positive interpretation. So, if a pimple appears in this place on a lonely girl, then soon fate will give her a meeting with an important person who may later become a spouse. A pimple on the chin is generally associated with love relationships, so if the rash is frequent, this indicates a stormy personal life and impending passionate romances. If suddenly a pimple on your chin begins to hurt and itch, then it is better not to quarrel with your significant other in the near future in order to avoid a break in the relationship.
Since ancient times, acne on the forehead has been given serious importance. They were considered a symbol of recovery. If you are overcome by an illness, then a pimple that pops up on your forehead indicates that the disease will soon recede. But if you are healthy, then you should be wary and more attentive to your health. Often we wait for a sign from fate in favor of making a decision. It is believed that a pimple on the forehead is such a sign. Cast aside doubts and step boldly towards change.
Kisses with a loved one are foreshadowed by a pimple on the lower lip. If it jumps up on the upper lip, then a long-awaited meeting with a friend or relative will soon take place. If a pimple pops up in the corner of your lip, then be prepared for temporary difficulties in family relationships. Learn to compromise.
Pimples on the nose were jokingly called a sign of excessive curiosity. In fact, if a pimple appears on the tip of your nose, then stop interfering in someone else’s life, do not give advice unless you have been asked to do so.
Acne on the right cheek promises a change in financial condition, usually for the better, but you need to try for this. Maybe you should take a risk and take on a new project or improve your grades in order to receive a scholarship. Pimples on the left cheek indicate that you will be able to restore long-lost connections with someone close to you.
If the rashes are located closer to the bridge of the nose or in the eyebrow area, then this is a good sign. It portends leisure time in a friendly atmosphere.
Prevention
Simple tips can help reduce the risk of inflammatory diseases of the oral cavity.
- Complete nutrition.
- Elimination of allergens from the diet.
- Avoiding irritating and hard foods that injure the mucous membrane.
- Careful oral hygiene (brushing teeth, using rinses and dental floss).
- Using a toothbrush with soft bristles, which also prevents injury to the mucous membrane.
- The use of pastes with antibacterial action.
- If inflammatory elements appear in the mouth, consult a dentist.
Signs: biting your tongue while eating
Often, eating is marred by biting the tongue; few people think that this happens for a reason. A tongue bitten while eating advises you to immediately shut up. Most likely, you have started a fascinating story about someone else’s life and are about to tell your interlocutor someone else’s secret. You risk being left with a painful sensation in your mouth, as well as without the trust of a friend.
Another belief says that if you eat alone and your tongue is bitten, it means that you are being discussed at the moment. At the same time, you are not viewed in the best way; think about who you might have “annoyed” over the past time.
A different situation arises if it is not you who bites your tongue, but your interlocutor. Listen and think carefully about his speech, is there so much truth in it? Perhaps they are lying to you. Do not fall for lies, do not go into discussion with a person about a specific person. There are often cases when your expressed opinion will play an evil trick on you.
List of sources
- Karakov K.G., Vlasova T.N., Lavrinenko V.I. Independent and symptomatic glossitis in the clinic of therapeutic dentistry // Textbook. Stavropol, Publishing and Information, 2012. – 102 p.
- Borovsky E.V., Mashkilleyson A.L. Diseases of the mucous membrane of the oral cavity and lips. // M., 2001, 73-90.
- Danilevsky N.F., Leontiev V.K., Nesin A.F., Rakhni Zh.I. DISEASES OF THE ORAL MUCOSA // Textbook. Moscow, 2001.- 268 p.
- Borovsky E.V., Danilevsky N.F. Atlas of diseases of the oral mucosa. - M.: Medicine, 1991.
- Beloklitskaya G.F. The use of chlorhexidine-containing drugs in dentistry (literature review) / G.F. Beloklitskaya // Modern dentistry. - 2001. - No. 1. — P.15-18.