During the period of intrauterine development, the baby’s body completely depends on the lifestyle of the expectant mother. If a woman does not experience nervous overload, gets full rest, and eats right, then the child feels protected. Particularly conscious young ladies switch to a proper diet even when planning a pregnancy. However, in most cases, questions about nutrition during the perinatal period arise after an event has occurred. Advice from gynecologists, nutritionists, and pediatricians will help you develop a personal menu.
Nutrition during pregnancy raises many questions. Firstly, the older generation advises “eating for two”, and women are afraid of gaining extra pounds. Secondly, hormonal changes in the body dictate new gastronomic preferences. Fearing harm to the child, the expectant mother is lost between “would I like to” and “can I?” Thirdly, the pseudo-medical advice on nutrition that is poured in abundance on women from social networks is confusing. How to choose healthy foods, safe cooking methods, and create a diet during pregnancy? Read our article.
Nutrition during pregnancy
Organization of nutrition during the perinatal period is aimed at maintaining the health of the woman and ensuring the harmonious development of the baby. The main tool in achieving the goal is the responsible attitude of the expectant mother to her daily diet. Poor nutrition during pregnancy results in nutritional deficiency. This leads to the occurrence of intrauterine pathologies, complications of gestation, increases the chances of the child developing autoimmune reactions, and activation of unfavorable genetics (hereditary predisposition to diseases).
The causes of nutritional imbalance in the body of a pregnant woman are:
• Calorie deficit and surplus. The low energy value of the diet forces the baby’s body to turn on the mechanism of accelerated absorption of everything that the mother eats. Nutrigeneticists claim that the habit of eating everything continues after birth, threatening obesity. In the female body, a lack of calories is reflected in the weakness of the uterine muscles. There is a danger of miscarriage. Excess calories lead to excess weight gain, and this puts stress on joints, blood vessels, and the risk of developing gestational diabetes mellitus, hypertension, and varicose veins. • Lack of vitamins. Hypovitaminosis during pregnancy is a direct threat to the life and health of the child. Deficiency of vitamins A and E slows down fetal growth and provokes premature birth. Deficiency of B1, B9 causes defects in the development of the nervous system. Vitamin D deficiency is the cause of neonatal rickets and visual impairment. Hypovitaminosis B2 results in heart defects, cleft palate, and deformation of the arms and legs of a newborn. • Lack of minerals. Microelements participate in embryonic development no less than vitamins. Copper deficiency leads to a decrease in the immune status of mother and child, calcium, phosphorus - to demineralization of fetal bone tissue, iodine - to a delay in the neuropsychic development of the baby, iron - to iron deficiency anemia in a pregnant woman, the threat of miscarriage, magnesium - to premature birth, development arrhythmias in the mother, zinc - to slow growth of the embryo.
Eating right means ensuring your child’s stable growth and development, and protecting yourself from perinatal risks and complicated childbirth. A pregnant woman needs to eat not “for two,” but “for two.”
Approximate vitamin and mineral norm per day (in mg)
Minerals
- calcium - 1200
- phosphorus - 700
- magnesium – 360
- iodine - 200
- zinc - 15
- iron - 30
- copper - 2-3
Vitamins
- retinol (A) - 1.2
- thiamine (B1) - 1.8
- pyridoxine (B6) - 2.1
- folic acid (B9) - 400 mcg
- tocopherol (E) – 10
- ergocalciferol (D) – 500IU
- ascorbic acid (C) – 100
To prevent vitamin and mineral deficiency, it is recommended to supplement your diet with special vitamins for pregnant women.
Early signs of pregnancy
For women with a regular monthly menstrual cycle, the earliest and most reliable sign of pregnancy is a missed period. However, there are other early signs of pregnancy that you should also pay attention to.
During pregnancy, a distinction is made between obstetric and embryonic periods.
Gynecologists count the obstetric period from the first day of the last menstruation, due to a simpler calculation, since the exact date of ovulation and conception is difficult to determine.
How do the first symptoms of pregnancy appear:
Each woman is individual, which means the first signs of pregnancy are not always identical. In this connection, it is difficult to notice the first symptoms, which may occur even before the delay.
The complete absence of early symptoms of pregnancy in the first weeks is very rare, and this is due to the increased level of sensitivity of the woman’s body to hCG (a hormone produced by the embryo in the first 14 days of its development).
And since this condition is not observed often, in most cases, it is still not difficult to notice the period of the first symptoms of pregnancy.
Among which a woman has:
- Feeling sick or vomiting (usually called morning sickness, but can happen at any time of the day or night).
- Metallic taste in the mouth.
- Flatulence (bloating).
- Dizziness.
- Feeling tired (common during pregnancy).
- Increased emotionality, depressed mood.
- Chest pain (manifests in the early stages).
At the same time, you may notice other signs of pregnancy:
- Constipation;
- Increased vaginal discharge (without pain or irritation);
- Strange tastes, smells and cravings for foods that previously disgusted you;
- Or, conversely, in the early stages of pregnancy you may find that you no longer enjoy some foods and drinks that you previously enjoyed;
- Loss of interest in smoking;
- The breasts become larger and there are diseases, as before menstruation;
- Veins may become more visible and nipples may darken and stand out.
In the early stages of pregnancy, frequent urination may be a concern. And such symptoms are easily confused with cystitis. This is why treatment without consulting a doctor can be harmful.
So, if you crave new foods, lose interest in certain foods or drinks you used to enjoy, such as tea, coffee or fatty foods, have a more sensitive sense of smell than usual, such as the smell of food or cooking, you often go to the toilet - talk to your doctor.
If you're sick all the time and can't suppress anything, see a therapist.
You may have hyperemesis gravidarum, a serious condition during pregnancy that causes severe vomiting and requires treatment.
Can pregnancy occur during menstruation?
Pregnant women sometimes experience bleeding that feels like a very light period, with some spotting. This is called “implantation bleeding,” which women confuse with real menstruation. This condition does not require treatment and, especially, the prescription of hormonal drugs - progesterone!
According to leading gynecologists, discharge in the early stages of pregnancy is almost always possible. However, implantation bleeding stops a little earlier than menstruation.
And this happens due to the fact that the fertilized egg, trying to attach to the wall of the uterus, causes slight bleeding.
Therefore, we can say with confidence that pregnancy does not happen if you have your period. If normal menstruation occurs, it means that the egg was not fertilized.
Delayed menstruation without accompanying symptoms is also not the main criterion for pregnancy. Since the reason may lie in a woman’s hormonal imbalance, which is provoked by stress, nervous strain, heavy physical activity or gynecological pathologies.
It is always very important to listen to your health and visit a gynecologist in a timely manner - this will help not only not to miss the first signs of pregnancy, but also gynecological pathologies.
What to do if you notice the first symptoms of pregnancy?
If you find clear signs of pregnancy in the first two weeks, you need to consult a gynecologist.
If pregnancy is confirmed, you need to listen to the doctor’s recommendations, get rid of bad habits (if any) and adjust the correct diet.
And of course, don’t forget about planned visits to the gynecologist, which are prescribed by the doctor on an individual basis.
Planned appointments for ultrasound examinations, tests, monitoring are the responsibility of the gynecologist managing the pregnancy.
During pregnancy, three scheduled ultrasounds are prescribed - once in the first trimester, in the second and sometimes in the third.
Additional unscheduled ultrasound examinations of a pregnant woman may be performed according to individual indications. This should not scare you, as it is necessary for making timely decisions to avoid certain complications.
Comprehensive support for women during pregnancy, qualified organization and support of childbirth is the main specialization of the Irkutsk City Perinatal Center. Here, all young mothers receive full medical care with an individual approach from doctors.
Difficult first trimester
The female body adapts to new conditions. Fatigue, drowsiness, and unstable mood are typical for a pregnant woman. There are problems with urination and bowel movements, acute reactions to tastes and smells. And at this time, the foundation of the baby’s health is laid. His nervous and circulatory systems are formed, and his heart begins to work intensively. Proper nutrition in the first trimester is a way to stabilize the mother’s condition and mitigate the risks of intrauterine anomalies.
Principles for creating a diet in the 1st trimester:
• Don't be greedy. Overeating increases the symptoms of toxicosis and provokes digestive failure. You need to eat in modest portions at intervals of 3-3.5 hours. • Take care of “building materials”. The basis for the formation of fetal cells is protein. From it the body receives 20 essential amino acids that it cannot produce on its own. The menu should include lean meat - turkey, chicken, veal. Twice a week you need to eat fish, alternating low-fat varieties (pollock, cod) with fatty ones (salmon, pink salmon, salmon). • “Agree” with the intestines. The problem for many women at the beginning of pregnancy is constipation. Fiber, which is found in raw vegetables, hard fruits, and bran, helps to cope with them. • Replenish supplies. During the formation of the nervous system, the baby squeezes iodine and B vitamins from the mother’s body. To prevent vitamin and mineral deficiency, shrimp, squid, seaweed and cauliflower, buckwheat porridge, eggs, and nuts should be introduced into the diet. • Do not experiment with drinks. It is recommended to drink water - still bottled or filtered. Adding freshly squeezed lemon juice will help calm nausea.
Daily caloric intake is 2500-2700. Nutrient distribution: proteins - 110 g, carbohydrates - 350 g, fats (vegetable + animal) - 75 g.
What to do if you have high stomach acidity
09.10.2021
Increased stomach is a very unpleasant ailment that affects many people. In particular, its exacerbation or onset is provoked by poor nutrition. In this article we will talk about how to reduce high stomach , how to eat and what to avoid.
Causes of high acidity
One of the main reasons for increased stomach is poor nutrition. Stomach acidity can be caused by carbonated, sweetened drinks, smoked foods, various sauces, fried foods, some citrus fruits, chocolate, mint, alcohol, and smoking. Therefore, you should think about your diet if you feel that your acidity is starting to increase at least a little. Poor diet weakens the valve at the bottom of the esophagus , causing stomach acid levels to rise.
Increased stomach can also be caused by various diseases - diabetes , excess weight, stomach ulcers . These diseases also develop mainly due to an unbalanced diet. Frequent stress can also cause increased stomach .
Symptoms of high stomach acidity
With increased stomach , certain symptoms occur. There may be a burning sensation, pain, and acidity in the mouth . Sometimes it can even be a dry cough. Particular attention should be paid if you do not have a cold, but the cough constantly torments you, especially at night, when lying down.
If you experience even the slightest symptoms, it's important to take action because, over time, rising stomach acid can cause sores, worsen your mouth, and damage your teeth . Without changing anything in your daily routine and allowing the disease to grow, the condition only gets worse. It feels like something is constantly burning in my mouth And this is a very unpleasant and upsetting feeling. Some may not even fall asleep because of this.
Of course, there are medications that help reduce acidity or sometimes relieve symptoms. But the most important thing is to change your lifestyle, habits, diet , and give up bad habits.
What to do and what to eat if you have high stomach acidity?
To prevent acid from rising or not arising at all, this unpleasant sensation must first be started with a diet .
- Excessively fatty, spicy foods, unhealthy snacks, processed foods, and alcohol should be avoided.
- You should also not eat salted, smoked foods, canned food, chocolate or products made from it.
- Among vegetables, garlic, onions, radishes, cucumbers, and horseradish should be avoided. Avoid pepper.
- Acidity can also be caused by ice cream or cold drinks.
- Avoid fatty meats, fried meats, sour fruits and berries.
- You should also avoid coffee and all products containing caffeine.
- You can eat crackers, chicken, beef, lean pork, boiled or stewed fish, and omelet. Use pure unrefined olive oil for cooking.
- It is better to cook vegetables. You can eat boiled potatoes, pumpkin, carrots and beets. You can also include spinach, cucumbers, and salads in your diet. Fruits include avocado, watermelon, bananas, papaya, melon, and baked apples.
- You can eat different nuts - pistachios, pumpkin seeds, almonds, cashews, walnuts, pecans, sesame seeds.
Tightening the diet should take at least a month, and some other foods can be added gradually after improvement. The main thing is to take your time and monitor your well-being. You should try to introduce a diet and eat every 3 hours, but not much. If you are overweight, you should try to lose it, this will also help improve your well-being. Eat only while sitting, do not lie down after eating. In the evening, the last meal should be no later than three hours before bedtime.
Well, if you don't have such problems, try to avoid them and start eating right!
Published in Gastroentorology Premium Clinic
Second trimester - needs increase
By about 14-15 weeks, the woman’s well-being returns to normal - toxicosis goes away, physical and emotional activity increases. The baby begins to produce blood cells, strengthens bone tissue, the pituitary gland begins to work, the first hair and nails appear, bone mineralization progresses, and muscles begin to contract. To meet the increased needs of the child, the mother needs to eat more. At the same time, it is not the caloric intake that needs to be increased, but the amount of nutrients. At this time, both organisms need vitamin D, calcium, and iron.
Mandatory foods in the diet:
• to provide calcium - cheese, cottage cheese, milk, almonds, sesame seeds; • sources of vitamin D - fatty fish, cod liver, eggs, butter, flaxseed, olive oil; • for the prevention of iron deficiency - beef and pork liver, cocoa, beans, cabbage, apples, blueberries, greens (spinach, parsley, mint). In the second trimester, it is important to control the amount of table salt and fluid you drink. This will help avoid surges in blood pressure and cardiac overload. Recommended values: calories - 2800-3000, proteins - 120 g, fats - 85 g, carbohydrates - 400 g.
The main causes of an unpleasant taste in the mouth during pregnancy
Why might pregnant women have an unpleasant taste in their mouth—bitter or sour? Experts say that there may be several reasons for this phenomenon, so to understand what causes this unusual taste, you need to pay attention to other symptoms. A sour taste may be a sign of hormonal imbalance, lack of vitamins or diseases of the digestive system.
Physiological and hormonal changes in the body
During pregnancy, significant hormonal and physiological changes occur in a woman's body. In the early stages, many suffer from toxicosis, which manifests itself in the form of nausea, heartburn, and vomiting. In this case, a sour or bitter taste periodically appears in the oral cavity, especially in the morning.
In the second and third trimesters, the reason for the appearance of a sour or bitter taste is not toxicosis, but the growing uterus. Starting from the middle of the term, the uterus begins to increase in size, displacing neighboring organs. It puts pressure on the liver, gall bladder and stomach. As a result, the woman experiences belching and heartburn, which is accompanied by a bitter and sour taste.
Another reason for a strange taste in the morning is high progesterone levels. This hormone has the property of relaxing muscles to reduce the tone of the uterus. At the same time as the myometrium, the esophageal sphincter also relaxes slightly, causing stomach acid to be released into the esophagus.
Various diseases
During pregnancy, many chronic diseases become aggravated. If a woman has previously had problems with the gastrointestinal tract, they can manifest themselves in the form of bitterness and acidity. If you feel unpleasant symptoms, the expectant mother should immediately consult a gastroenterologist for advice.
The table provides a list of diseases that cause an unpleasant taste in the mouth.
| No. | Name of the disease | general characteristics | Associated symptoms |
| 1 | Gastritis | Inflammation of the gastric mucosa, in which atrophy of epithelial cells occurs and glands are replaced by fibrous tissue. | Dyspepsia, burning in the stomach. |
| 2 | Stomach ulcer | A defect in the gastric mucosa causing trophic disorders. | Sour belching, heartburn, weight loss, pain in the epigastric region on an empty stomach. |
| 3 | Gastroesophageal reflux disease | The reflux of stomach contents into the esophagus, which leads to damage to its lower section. | Heartburn, sour belching, cough, sore throat, dry mouth. |
| 4 | Cholecystitis | Inflammation of the gallbladder. | Pain in the right hypochondrium, gradually shifting to the lumbar region and epigastrium, repeated vomiting, high temperature, over time the skin acquires a yellowish tint. |
| 5 | Cholelithiasis | Formation of stones in the gallbladder and ducts. | Sudden cutting pain in the right hypochondrium. |
Lack of vitamins and microelements
A sour or metallic taste in the mouth appears due to a lack of iron and vitamin C. A decrease in hemoglobin levels in the blood is a common occurrence during pregnancy, so doctors often prescribe vitamin complexes and iron-containing preparations to women.
Vitamin deficiency and lack of microelements are usually accompanied by poor health and chronic fatigue. Hair and nails become brittle, skin turns pale. Ulcers and wounds appear on the oral mucosa.
Third trimester - diet correction
From the 27th week of pregnancy, the female body begins to prepare for childbirth, and the baby begins to be born. At this time, gastronomic fads give way to heartburn, constipation, shortness of breath, swelling, and rapid weight gain.
A properly composed menu will help you adjust your well-being in the 3rd trimester. What should be done:
• Reduce the amount of protein foods. A protein surplus leads to kidney dysfunction and the accumulation of uric acid. • Avoid heartburn triggers - sour foods, black coffee, fried foods. • Replace 50% of animal fats with vegetable oils. They contain essential polyunsaturated acids Omega-3 and Omega-6, which are not synthesized by the body, but are needed for the absorption of minerals and vitamins. • Limit salty foods. Salt is the cause of edema, unstable functioning of the kidneys, heart, and blood vessels. • Set a limit on sweets. Simple carbohydrates quickly turn into extra pounds, causing flatulence, dyspepsia, and skin problems. • Eat more vegetables, fruits, berries, greens. Natural sources of vitamins provide energy and strengthen the immune system - this will come in handy during childbirth. Standards for KBJU: calories - 2900-3100, proteins - 100 g, fats - 75 g, carbohydrates - 400 g.
Causes of discomfort
The taste in the mouth tells about the health of the whole body.
The reasons for the appearance of acid in the oral cavity can be both diseases of various organs and a joyful event - the onset of pregnancy.
Possible diseases that cause an unpleasant aftertaste:
- increased acidity of gastric juice;
- excess production of hydrochloric acid;
- disturbances in the gastrointestinal tract - pancreas, reflux disease;
- periodontal diseases;
- the presence of crowns or fillings made of different metals in the oral cavity - such combinations form a galvanic couple and a physical and chemical reaction of electrolysis takes place in the oral cavity;
- electrolyte imbalance;
- dehydration of the body;
- taking medications;
- impaired bile formation and liver pathology - as a result of eating fatty and heavy foods; pregnancy in the middle and late stages - the growing uterus compresses the stomach and hydrochloric acid refluxes into the esophagus and oral cavity.
All these processes are accompanied by additional symptoms. Therefore, if you regularly experience an unpleasant sensation in the oral cavity, you should undergo a comprehensive examination.
If at the same time there is pain in the epigastrium, nausea, and stool disorder, then you need to urgently contact a medical institution.
The following video will familiarize you with the causes of sour taste in the mouth:
What should you not eat or drink?
There is no place for harmful foods in a properly composed diet for a pregnant woman. Throughout the perinatal period, the following are blacklisted:
• fast food; • flavored snacks; • hot sauces; • smoked meats; • products containing many preservatives; • alcohol.
The expectant mother is advised to limit the consumption of sausages, confectionery products, and sweet pastries. You also need to be careful with citrus fruits, strawberries, mushrooms, and coffee. It is advisable to exclude packaged juices, bottled tea, sweet cocktails, and soda from the grocery basket.
Dieting is difficult, but necessary. This will help minimize the harmful effects on the fetus, maintain pregnancy, improve well-being, avoid weight gain, and the development of gestational complications - preeclampsia, pyelonephritis, diabetes.
Newspaper "News of Medicine and Pharmacy" Gastroenterology (348) 2010 (thematic issue)
During pregnancy, a woman's stomach is especially vulnerable. Pregnancy is often accompanied by increased acid production, although it is possible that it may decrease. It is known that with increased stomach acidity, an increase in appetite is characteristic. However, it is not recommended to load the stomach with high acidity during pregnancy. During pregnancy, the stomach produces more hydrochloric acid not so much to increase appetite, but to increase the bactericidal properties of its contents.
An unpleasant feeling of slight heat or burning in the pit of the stomach, sour belching - all these symptoms are combined into one term “heartburn”. During pregnancy, heartburn is caused by hormonal and physical changes in a woman's body. It is observed in approximately 50% of women during pregnancy at any stage, but more often in the second and third trimesters, and is provoked by the consumption of abundant fatty, fried and spicy foods. Its occurrence is due to the reflux of acidic (much less often alkaline) gastric contents into the lower esophagus and its irritating effect. As is known, in pregnant women the tone of the lower esophageal sphincter is significantly weakened, which is the result of the action of progesterone, and an enlarged uterus by the 25th week contributes to an increase in intra-abdominal pressure, which prevents complete closure of the sphincter. Progesterone also reduces contractions of the esophagus and intestines, slowing digestion. The feeling of heartburn is accompanied by a feeling of melancholy and depressed mood.
Another symptom typical of stomach pathology is pain. The nature of pain in stomach diseases may indicate not only the disease, but also the presence of complications. Thus, the occurrence of burning pain in patients with gastritis or peptic ulcer may indicate the addition of solarium. Pregnant women with chronic gastritis with reduced gastric secretion usually experience a feeling of heaviness and fullness in the epigastric region. This feeling also appears with pyloric stenosis. In pregnant women with chronic gastritis with preserved secretion, the pain is often dull and aching. The intensity of pain in stomach diseases can vary. With chronic gastritis, pain in the epigastrium is usually low-intensity, and with gastric ulcer, and especially with duodenal ulcer, the pain is usually severe. With a perforated ulcer, the pain intensity is so high that pain shock is possible.
According to a number of authors, chronic duodenitis occurs in pregnant women much more often than is diagnosed, is observed in the first trimester of pregnancy or 4-5 weeks before birth and is characterized by cyclical exacerbations (spring - autumn). The clinical picture is dominated by pain; night and hunger pains are typical; eating reduces them. The goal of drug treatment for chronic duodenitis in pregnant women is to achieve remission of the disease. In the uncomplicated course of chronic gastritis or duodenitis, the patient’s condition is not significantly disturbed, and the disease does not have a noticeable effect on the course of pregnancy and its outcome. When vomiting during pregnancy occurs, treatment of gastritis or duodenitis should be combined with treatment of early toxicosis.
The literature describes isolated information about the course of pregnancy against the background of Ménétrier's disease. Analysis of literature data does not allow us to draw conclusions about the etiology of the disease, although the role of cytomegalovirus is assumed. Along with the complaints characteristic of chronic gastritis, pregnant women experience lethargy and possible swelling of the lower extremities. It was noted that in the second half of pregnancy the disease is severe, but it is not a contraindication for pregnancy. During pregnancy, the diagnosis is established on the basis of gastroscopy, in which the gastric mucosa is pale gray, swollen, easily vulnerable, eroded, with the presence of hemorrhages. Treatment is symptomatic, since, according to most researchers, gastrectomy outside pregnancy is indicated.
Peptic ulcer disease in pregnant women is quite common, but the exact incidence is difficult to estimate, since diagnosing peptic ulcer disease during pregnancy is difficult. The chance of encountering this disease in pregnant women has increased significantly, although in the vast majority of cases pregnancy softens the clinical course of peptic ulcer disease. The reason for the favorable course of peptic ulcer disease in pregnant women has not been fully studied. Some researchers believe that this is the result of altered secretory (decreased production of hydrochloric acid and increased mucus production) and motor functions of the stomach in the direction of reducing it and increasing blood supply. It has been established that during pregnancy, in 40% of cases, remission of gastric and duodenal ulcers occurs due to the high level of progesterone in the body, which stimulates the production of mucus, which is a protective mechanism of the gastric mucosa. Perhaps the overproduction of sex hormones, namely estrogens, plays a role. It has been established that estrogens perform a protective function, increase the intensity of regenerative processes, and improve blood supply to the gastroduodenal area. For most women, the disease does not affect the process of bearing and giving birth to a child. However, exacerbation of peptic ulcer disease during pregnancy, although unlikely, is still possible (in 10% of cases). Most pregnant women associate it with excessive anxiety, fear of the upcoming birth and its outcome, probably because pregnancy itself is stressful for a woman. The main symptoms of a peptic ulcer are: pain in the epigastric region (under the stomach), belching of air, food, nausea, sometimes vomiting, constipation, flatulence, weight loss. Peptic ulcer disease is dangerous due to its complications, one of which is gastrointestinal bleeding, which sharply increases the risk of fetal death. Massive bleeding during pregnancy is an indication for emergency surgery.
Stomach cancer is quite rare in pregnant women. The authors note that for stomach cancer in pregnant women, the first symptoms appear at 15–16 weeks of pregnancy. Pain in the epigastric region, lack of appetite, nausea, vomiting are noted, melena is possible, but the symptoms are unclear and the clinical picture is blurred. The diagnosis is established on the basis of fibrogastroscopy with biopsy. Treatment is only surgical, since conservative treatment is not effective. According to most authors, the prognosis for the mother and fetus is unfavorable.
Gastric resection is one of the most common operations for gastric disease. It is known that pregnant women with a resected stomach are more likely to develop digestive system disorders, which is explained by the depletion of compensatory capabilities in this category of women. However, the issue of the influence of pregnancy on the health of women with a resected stomach and on the course of pregnancy itself in this category of women has not yet been sufficiently studied and is poorly covered in the literature.
Pregnancy imposes significant restrictions on the choice of diagnostic methods and on determining treatment tactics. X-ray examination of the stomach is not recommended for pregnant women, therefore the only diagnostic method for stomach pathology is esophagogastroduodenoscopy, although its implementation can be difficult.
Since therapy aimed at destroying Helicobacter pylori is not carried out during pregnancy, diagnosis of this infection is carried out after childbirth (a breath test is performed if necessary). Antacids are recommended for use during exacerbations of peptic ulcer disease in pregnant women. Antacids containing aluminum, calcium, or magnesium are considered safe and effective in treating heartburn during pregnancy. However, magnesium-containing antacids should be avoided during the third trimester of pregnancy because they may trigger preterm labor. In addition, antacids containing sodium bicarbonate should be avoided to avoid the occurrence of metabolic alkalosis. In addition, it is possible to prescribe enveloping and astringent agents of plant origin - decoctions of chamomile, St. John's wort.
H2-blockers of histamine receptors are also undesirable for pregnant women. However, it has been established that ranitidine is the only histamine H2 receptor antagonist that has been well studied during pregnancy. In a double-blind, placebo-controlled study, JD Larson et al. (1997) proved that ranitidine, taken several times a day by pregnant patients with heartburn (if antacids are ineffective), reduced its severity. No adverse effects on the fetus have been reported. A study on the safety of ranitidine by JE Richter (2003) showed that pregnant women who took it from the first trimester throughout pregnancy gave birth to healthy children. Taking proton pump inhibitors for acid-dependent conditions by pregnant women is undesirable and is possible only if antacids are ineffective. More recently (May 2010), new evidence has emerged showing an increased risk of hip, wrist and spine fractures with long-term or high-dose use of proton pump inhibitors, as well as a more than doubling of the risk of having a baby with heart defects. Only when the threat to the mother's health outweighs the potential risk to the fetus is it possible to prescribe short-term courses of proton pump inhibitors. Recently, evidence has emerged that lansoprazole and pantoprazole are priority representatives of this class of drugs, since their relative safety in pregnant women has been studied. Due to the fact that the range of medications for acid-dependent gastric conditions during pregnancy is limited, dietary measures play an important role. In addition, it is recommended to limit physical activity, semi-bed rest, split meals, and strict adherence to diet No. 1 during the period of exacerbation of the disease.
Diet rules
The principles of constructing a diet during the perinatal period differ little from the general rules of healthy eating. After all, pregnancy is not a disease.
Organizing a proper diet includes:
• Refusal of junk food and drinks. Carcinogens, preservatives, flavorings, flavor enhancers, and alcohol increase perinatal risks. • Control of KBJU. Helps maintain stable weight and nutritional balance. • Daily consumption of healthy foods containing protein, minerals, vitamins. These substances are necessary for the development of the fetus and the health of the mother. • Compliance with the drinking regime (1.5-2 liters per day). Clean water ensures normal blood flow, regulates the functioning of the urinary organs and intestines. • Small meals: 5-6 times a day with an interval of 3-4 hours. This schedule helps you not to overeat and properly absorb nutrients. • Cooking foods in healthy ways. Cooking dishes by boiling, stewing, and baking allows you to reduce calories, reduce the load on the digestive organs, and get rid of nausea and heartburn. • Limiting salt. A slight salt deficiency during pregnancy reduces the load on the kidneys and heart muscle and prevents the appearance of swelling. • Limit on fast carbohydrates. The body gets glucose from sweet foods, the main source of energy, so you can’t give them up completely. But excessive passion for confectionery products leads to metabolic failure, obesity, and the development of insulin resistance. • Keeping a food diary.
The diet for pregnant women has its bonuses. A woman will master healthy menu recipes, get used to eating right, and easily get into shape after giving birth. Of course, you shouldn’t make a cult out of food, forgetting about your own comfort and appearance. Special underwear for pregnant women will help you feel confident, and hypoallergenic products will take care of the beauty of your skin - stretch mark creams, gels, balms. Today, all products for pregnant women and nursing mothers can be ordered from an online pharmacy with home delivery.
Acid-dependent diseases during pregnancy
Heartburn during pregnancy is a very common complaint. It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
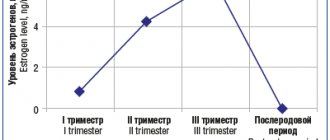
The main factors responsible for such a high prevalence of GERD during pregnancy include hormonal changes, such as hyperprogesteronemia (increased levels of the hormone progesterone) and hyperestrogenemia (increased levels of estrogen hormones), as well as increased intra-abdominal pressure due to the growth of the uterus and fetus.
The effect of gestational hormones in the first trimester of pregnancy is due to the fact that, without affecting the basal tone of the lower esophageal sphincter (LES), they reduce the increase in pressure of this sphincter in response to various physiological stimuli, including food intake. In the second and third trimesters of pregnancy, progesterone and estrogen reduce the basal tone of the LES to 50% of the initial level, the maximum reduction occurs at the 36th week of gestation. After successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called “pregnant heartburn”.
Heartburn in pregnant women usually does not lead to the development of esophagitis, complications of GERD (strictures, ulcers, bleeding) and does not require serious drug treatment.
If a woman suffered from GERD before pregnancy, during gestation the complaints may worsen and require examination and drug treatment.
The diagnosis of GERD during pregnancy is established primarily on the basis of complaints, medical history and objective examination. X-ray examination in pregnant women - due to a possible damaging effect on the fetus - is not used; pH-metry and manometry can be used, but the need for its use is doubtful.
Esophagogastroduodenoscopy (EGD) is the method of choice for diagnosing GERD in pregnant women, but it should be used only for strict indications, such as a history of complications of GERD and the ineffectiveness of drug therapy.
Treatment of GERD in pregnant women should be based on changes in lifestyle and nutrition: avoiding a horizontal body position immediately after meals, sleeping with the head of the bed elevated (15 cm), avoiding physical activity that increases intra-abdominal pressure (including wearing corsets, tight belts, bandages). The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, and pay special attention to normalizing stool.
First-line drugs for the treatment of GERD in pregnant women include antacids and alginates. If these drugs are ineffective, it is permissible to prescribe prokinetics (metoclopramide), histamine H2 receptor blockers and (if strictly indicated) proton pump inhibitors (PPIs).
H2-histamine blockers are the most commonly prescribed group of drugs for pregnant women. They are classified as risk category B by the US Food and Drug Administration (FDA) (“drugs that have been taken by a limited number of pregnant women without evidence of an effect on the incidence of congenital anomalies or harm to the fetus”). Russian instructions allow only cimetidine and ranitidine with the caveat: use during pregnancy is possible only if the expected effect of therapy exceeds the potential risk to the fetus. Famotidine and nizatidine are contraindicated in the Russian Federation for pregnant women.
Despite the fact that the FDA also classifies most PPIs as risk category B, in Russia there are stricter restrictions on the use of this group of drugs in pregnant women. Thus, lansoprazole is contraindicated in the first trimester; in the second and third trimesters, its use is possible only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole is contraindicated during pregnancy.
Pregnancy has a beneficial effect on the course of peptic ulcer disease: 75–80% of women experience remission of the disease, and it does not have a noticeable effect on its outcome. However, some patients may experience an exacerbation. Most often this is observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2–4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer disease does not have a negative effect on fetal development.
Treatment of peptic ulcer in pregnant women includes adherence to generally accepted “regime” measures and diet; taking non-absorbable antacids in usual therapeutic doses (1 sachet 3 times a day 1 hour after meals and adsorbents 1 sachet 3 times a day 1 hour after meals). If there is no effect, H2-blockers are prescribed (ranitidine 150/300 mg once at night); if they are insufficiently effective, as well as if complications develop, we can take PPIs (omeprazole 20–40 mg, lansoprazole 30–60 mg, pantoprazole 40 mg). mg, in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection is not carried out in pregnant women.