Symptoms of the disease
This pathology occurs in type I diabetes mellitus, but can also occur in type II diabetes. Therefore, at the first signs of illness, immediately consult a doctor to prescribe treatment.
Symptoms include:
- Abdominal pain.
- Vomit.
- Cardiopalmus.
- Acetone smell on your breath (or other unusual odor).
- Dehydration of the body (dehydration).
- Disorientation in space, confusion.
- Unconsciousness (or coma).
Ketone bodies are found in urine.
Causes of the pathological condition
Ketoacidosis appears in the following cases:
- When a very low dose of insulin is administered.
- Eating large amounts of carbohydrates.
- Missing a dose of insulin.
- Excessive physical activity.
- Severe stress.
- Excessive alcohol consumption.
- The presence of an infectious disease.
- Using ecstasy or cocaine.
When blood sugar levels are significantly higher than normal, hyperglycemia occurs in the body and the number of ketone bodies increases.
Prevention of diabetes complications:
- correct treatment regimen - correctly selected drug and dose (sugar levels are always normal);
- fulfilling all doctor's orders;
- weight normalization;
- normal motor activity;
- sufficient sleep;
- balanced diet;
- regular examinations by an endocrinologist, vascular surgeon, neurologist, ophthalmologist, podologist, nephrologist.
Professional medical supervision, patient self-discipline and a healthy lifestyle can reduce diabetes complications to a minimum or even prevent them altogether.
Mechanism of development of diabetic ketoacidosis
If there is a lack of insulin, the body cannot convert glucose into the energy it needs. Fat consumption begins. When they are used, ketone bodies accumulate in the body, the content of which rapidly increases. Ketone bodies cannot enter the blood due to the lack of insulin. They pass through the kidneys into the urine. A high content of by-products quickly poisons the body and leads to complications.
A patient who knows about the causes, symptoms, methods of prevention and treatment can avoid the occurrence of diabetic ketoacidosis.
Ways to reduce odor
First of all, you need to determine the cause of halitosis. If diabetic halitosis with a characteristic ammonia odor is complemented by putrid, sour, rotten “odors,” you should undergo an examination of the internal organs, including:
- laboratory tests of urine and blood;
- ultrasound of the abdominal cavity (with kidneys).
If necessary, the treating endocrinologist may prescribe additional diagnostic procedures. To eliminate ketoacidosis, it is recommended to adjust the diet. In the daily menu, it is necessary to reduce the amount of protein foods and fats, replacing them with complex carbohydrates (porridges, vegetable dishes, fruits allowed for diabetes).
The following methods can be used to weaken the antipathetic amber:
- mint candies and tablets (for diabetics, the absence of sugar in the composition is important), mint leaves;
- anise seeds, juniper berries;
- sprays for mouth freshening with an antiseptic effect;
- pharmaceutical mouth rinses with eucalyptus, mint, menthol extracts
- decoctions of herbs with antibacterial properties (chamomile, sage, etc.) for rinsing;
- vegetable oil for rinsing the mouth (a five-minute procedure will help freshen your breath for a long time, but the oil should not be swallowed).
Regular oral hygiene is a prerequisite. When choosing a toothpaste, you should consult your dentist.
How to check your ketone levels?
As DKA develops, symptoms appear quickly. If one or more signs are present, blood and urine are tested for ketone bodies. They appear in the blood much faster than in the urine. To prevent poisoning of the body, perform the following measures:
- A blood test is performed to check for the presence of ketone bodies. If your home glucose meter can do this, use it. All you have to do is insert the required test strip.
- Study the result obtained. A value up to 0.6 mmol/l does not require any action. This indicator is considered the norm. An average level of 0.6-1.5 mmol/l indicates the beginning of the formation of ketone bodies in the body. Over the next 1.5-2 hours, you may need the help of a doctor. A high content of ketone bodies (more than 1.5 mmol/l) requires immediate medical attention and behavioral caution.
The attending physician is informed of the diagnosis and adheres to the prescribed recommendations.
Halitosis test
When visiting a dentist, testing for halitosis is carried out using a special halitometer. The five-point scale of the device allows you to evaluate the result from “0” - no odor, to “5” - pronounced and sharp. At home, you can test yourself using a sterile pharmaceutical mask. You need to put it on and exhale forcefully.
In case of diseases of the teeth and gums, an environment favorable for the growth of bacteria is created in the oral cavity - the cause of an unpleasant odor
The freshness of your breath will be determined by the intensity of the perceptible “aroma”. Instead of a mask, you can use a cup or plastic bag, which must be pressed tightly to the mouth, take a deep breath and exhale as forcefully as possible. Another option is a wrist test. To do this, you need to lick this area of your hand, wait 20 seconds and smell.
Important! You can carry out independent manipulations to determine halitosis in the absence of rhinitis (runny nose) or other pathologies associated with a difficult sense of smell.
Treatment
DKA requires immediate hospitalization and intensive care. With correct measures taken, the condition resolves within 24 hours. Perform the following actions:
- Blood sugar levels return to normal.
- They flood the body.
- Restores mineral balance.
With timely detection and correct diagnosis, ketoacidosis resolves without complications or with minimal negative consequences. If there is delay, coma or death occurs. Control of nutrition and blood glucose levels is the main prevention of the development of DKA.
Late chronic types of complications of diabetes mellitus
Diabetic micro- and macroangiopathy
Damage to the walls of large vessels and capillaries, accompanied by a violation of the functional state of the blood.
Causes
Occurs during decompensation of diabetes - with large daily fluctuations in the levels of glucose, proteins and fats. Aggravating factors of development are obesity, hypertension, smoking.
Signs
Due to metabolic disorders, the vessels of target organs are affected - the heart and limbs, the retina and the renal glomeruli. Because of this, the supply of oxygen to tissues is reduced, hormonal balance and metabolic processes are disrupted.
As a result:
- visual functions deteriorate;
- cardiovascular and renal failure develops;
- brain activity and nerve conduction are disrupted;
- Trophic ulcers develop on the arms and legs.
Without treatment, angiopathy progresses and can lead to complete blindness, amputations of limbs, heart attacks and intoxications, and deterioration of mental abilities.
Treatment
Diabetic angiopathy requires correction of the treatment regimen, as well as normalization of weight and blood pressure, and cessation of smoking. In addition, the doctor may prescribe drugs that strengthen the vascular wall - flavonoids, venotonics and phlebotonics.
Diabetic polyneuropathy
Damage to nerve endings up to complete ischemia - loss of sensitivity in the affected areas.
Causes
Develops with elevated blood sugar levels - when the drug or dose is chosen incorrectly.
Signs
Manifested by pain, loss of sensitivity, numbness, and night cramps. If large nerve fibers are damaged, loss of balance may occur.
Treatment
The goal of treatment is compensation of diabetes mellitus. Also indicated are drugs that improve neuromuscular conduction and symptomatic drugs for pain and cramps.
Diabetic encephalopathy
Damage to brain structures - mainly neurons and white matter. It develops slowly and imperceptibly, so it often appears in the later stages.
Causes
Typical metabolic disorders associated with long-term diabetes mellitus. In addition, risk factors are atherosclerosis, hypertension, and increased levels of C-peptide in the blood.
Signs
- deterioration of mental activity – mild to moderate (dementia rarely develops);
- emotional instability;
- increased anxiety;
- tendency to depression;
- chronic fatigue syndrome.
Treatment
Regular cognitive screenings and maintaining normal blood sugar levels. To improve brain activity, nootropic, antioxidant, antiplatelet and vasoactive drugs, vitamins B, E and alpha-lipoic acid are prescribed.
Diabetic foot syndrome
Purulent-necrotic and ulcerative lesions of the feet.
Causes
The condition occurs due to complex changes against the background of diabetic pathologies of blood vessels, nerves and tissues.
Signs
It manifests itself as increased trauma and infection of tissues, purulent-necrotic processes, which may require amputation.
Treatment
- control and correction of blood glucose levels;
- control and correction of blood pressure and cholesterol levels;
- professional foot care, monthly examinations by a podiatrist;
- unloading the foot;
- antiseptics and antibiotics for signs of wound infection;
- painkillers;
- drugs that improve nerve conduction;
- medications that improve blood flow.
When phlegmons and abscesses form, surgical opening is indicated. According to indications, angioplasty and stenting are performed. In extreme cases, gentle resections or amputations may be necessary.
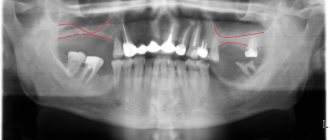
Diabetic nephropathy
Damage to kidney structures due to diabetic metabolic disorders.
Causes
Elevated blood sugar levels cause increased pressure in the glomeruli. Because of this, the kidneys begin to excrete protein in the urine. Over time, this causes fibrosis of the kidney tissue. A factor that worsens the prognosis is concomitant atherosclerosis.
Signs
The disease remains asymptomatic for years and eventually leads to kidney failure. Its symptoms are a sharp decrease in daily urine volume and critical disruption of urinary processes.
Treatment
Selecting the correct treatment regimen allows you to prevent the process and even cause its reverse development in the early stages of the disease. Specific treatment is carried out with ACE inhibitors or angiotensin receptor blockers. Nephroprotectors are often prescribed; in severe cases - hemodialysis.
For elevated cholesterol levels, statins are indicated, and for hypertension, antihypertensive drugs are indicated. Diabetics with nephropathy are prescribed a diet with moderate restriction of animal protein. It is also important to normalize your weight and quit smoking.
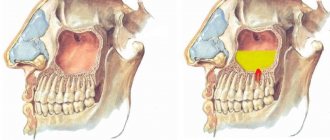
Diabetic retinopathy
Damage to the vessels of the retina of the eyeballs.
Causes
Develops due to decompensation of diabetes. Due to increased blood glucose levels, the barrier properties of the retinal tissues decrease, the lumen of the vessels and the blood flow in them increase, the inner wall of the vessels is damaged, and the capillaries become permeable. Due to repeated hemorrhages, degeneration of the ocular structures develops.
Signs
Diabetic retinopathy is manifested by deterioration of vision up to complete blindness. Possible eye pain.
Treatment
Annual examination by an ophthalmologist specializing in diabetes, monitoring of sugar levels and dietary therapy. Animal fats are replaced with vegetable fats, fast carbohydrates are excluded, and lipotropic foods are introduced into the diet - fish, oatmeal and cottage cheese - to normalize cholesterol levels.
The menu also includes more fruits and vegetables (except starchy ones). Vitamin therapy and angioprotectors are often prescribed. At stages 3 and 4 of diabetic angiopathy, laser photocoagulation may be recommended.