July 30, 2020
To talk about local inflammation, you must first understand what lymphadenitis is in general. This is an inflammatory process in the lymph nodes, sometimes accompanied by suppuration
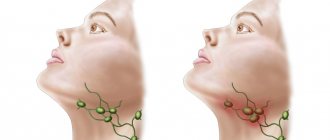
To talk about local inflammation, you must first understand what lymphadenitis is in general. This is an inflammatory process in the lymph nodes, sometimes accompanied by suppuration. It manifests itself through enlargement of one or more lymph nodes and can occur in several regions of the body at once. Clinical signs of the disease depend on the form and type of lymphadenitis: acute or chronic, regional (damage to lymph nodes of one anatomical group) and generalized (involvement of several groups of lymph nodes), serous, purulent, gangrenous, hemorrhagic, phlegmonous.
In the body, lymph nodes create a protective barrier against viruses, infections, cancer cells, participate in the formation of lymphocytes (special cells that destroy foreign microorganisms) and the production of phagocytes, antibodies (immune cells), participate in digestion and metabolic processes, distribute intercellular fluid between body tissues and lymph.
Normally, the lymph nodes are not palpable or are palpated in the form of elastic, small-sized formations that are not fused with adjacent tissues or with each other. Depending on the prevalence, the following types of lymphadenitis should be distinguished:
- local - enlargement of one lymph node in one of the areas (single cervical, supraclavicular lymph nodes);
- regional - enlargement of several lymph nodes in one or two adjacent areas (supraclavicular and axillary, supraclavicular and cervical, occipital and submandibular lymph nodes, etc.);
- generalized - enlargement of lymph nodes in three or more areas (cervical, supraclavicular, axillary, inguinal, etc.).
With axillary lymphadenitis, enlarged lymph nodes in the armpit are palpated. Symptoms of axillary lymphadenitis:
- Enlarged lymph nodes
- Painful sensations when palpating the affected area, turning the body, or moving
- Inflamed nodes are fused together with each other and adjacent tissues into one dense conglomerate
- The skin over the inflamed lymph nodes is hyperemic
- Symptoms of body intoxication appear - fever, weakness, headache, lack of appetite, feeling weak, muscle pain
Often the disease is accompanied by symptoms of the underlying disease; in addition, the patient may be bothered by:
- night sweats;
- weight loss;
- prolonged increase in body temperature;
- frequent recurrent upper respiratory tract infections;
- pathological changes on a chest x-ray;
- hepatomegaly;
- splenomegaly.
Causes of lymphadenitis
The function of the lymph nodes is to prevent the spread of infectious processes in the body. Any infectious agent that gets into them is destroyed by lymphocytes. When too many foreign microorganisms arrive, lymphocytes cannot cope with so many bacteria, the latter begin to actively multiply. This creates conditions for other types of leukocytes to penetrate into the site of inflammation, which causes an enlargement of the lymph nodes. One or more of them may become inflamed.
Inflammation can be nonspecific and specific. In the first case, the causes of the disease are bacteria and their toxins, viruses, and fungi. Lymphadenitis of the lymph nodes is caused by staphylococci and streptococci; they are pyogenic flora. The primary source of infection in the nonspecific form of the disease are boils, festering wounds, trophic ulcers, caries, erysipelas, and thrombophlebitis. In children, inflammation of the lymph nodes is often a complication of inflammatory processes in the ENT organs (tonsillitis, tonsillitis, otitis media, influenza), childhood infections (scarlet fever, mumps, diphtheria) and skin diseases (diathesis, pyoderma).
A specific type of disease is triggered by certain types of microorganisms:
- tuberculous mycobacterium;
- plague stick;
- Brucella (the causative agent of brucellosis);
- Treponema pallidum (the causative agent of syphilis);
- tularemia bacteria (causing tularemia);
- actinomycete (the causative agent of actinomycosis).
When infected with these types of microorganisms, special symptoms characteristic of a particular disease develop. Lymph nodes undergo specific changes, since infectious agents enter them with the flow of lymph.
Symptoms of lymphadenitis
Based on the nature of the inflammatory process, the following forms of the disease are distinguished:
- Acute lymphadenitis. The duration of the course is up to two weeks. Characteristic symptoms: pain and enlargement of regional lymph nodes, fever, headache, general weakness, loss of appetite, swelling and redness of the skin in the area of the affected node.
- Chronic lymphadenitis. The duration of the disease is 1 month or more. Develops with a sluggish infection or after untreated acute lymphadenitis. With this course, the pain syndrome is erased, but the lymph nodes themselves remain enlarged and dense. Lymphatic fluid retention and swelling are noted.
Lymphadenitis is classified according to the location of the inflamed lymph nodes into the submandibular, cervical, axillary and inguinal. All of them are characterized by similar symptoms: enlarged lymph nodes, pain, redness of the skin, intoxication syndrome. The differences are due to the location of the inflammatory focus.
Thus, with cervical lymphadenitis, there is a restriction in head movement; when turning or bending, the patient feels acute severe pain. If the lump is large, it can put pressure on the organs of the neck and cause difficulty breathing, changes in voice, and difficulty swallowing food.
Submandibular lymphadenitis is accompanied by pain in the jaw during talking or eating, but is rarely bothersome at rest. With the axillary type of the disease, hand movement is impaired, swelling of the upper limb on the affected side increases and its sensitivity is impaired.
Inguinal lymphadenitis is characterized by swelling of the legs on the affected side. This manifestation is due to a violation of the outflow of lymph and compression of large vessels in the groin area. If suppuration occurs, the body temperature can rise to 40 degrees, the patient feels weakness and pain in the lower abdomen.
WHAT DOES LYMPHADENITIS THREATEN?
22.Mar.2021
The infection can enter the lymph node from a wound, boil (boil), panaritium, diseased tooth and other sources. The inflammatory process is accompanied by pain and enlargement of the lymph node, headache, weakness, general malaise, and increased body temperature.
In the case when suppuration of the lymph nodes themselves occurs, the symptoms become more pronounced: intense pain appears, the skin over the lymph nodes becomes red, the previously clearly defined nodes merge with each other and the surrounding tissues, and become immobile.
Of practical importance are primarily superficial and deep lymphadenitis of the face and neck. In the facial area, there are buccal, parotid and mandibular lymph nodes.
In the tissue on the outer surface of the body of the lower jaw and in front of the place of attachment of the masticatory muscle, the so-called supramillary or mandibular lymph nodes are located. The deep nodes are located between the lobules of the parotid gland, corresponding to the level of the earlobe.
Acute inflammation begins with a feeling of some awkwardness when moving the head, dull pain in the area of the affected node or group of nodes. Enlarged lymph nodes are clearly visible on palpation, but they are somewhat painful and have a dense elastic consistency. General disturbances at the beginning of inflammation may be absent or mild.
If the course is unfavorable, the inflammation can turn purulent: the node becomes inactive, “fused” with others, forming a group. Body temperature rises to 37.2-37.8 °C. Changes characteristic of ulcers appear in the blood. The patient becomes unwell, weak, loses appetite, etc. In turn, the inflamed lymph node gradually melts and leads to the formation of a fistula tract (with the disease becoming chronic).
Chronic specific lymphadenitis, as a rule, affects the mandibular, submandibular, premaxillary and cervical nodes. Sometimes it is combined with damage to the lymph nodes in other parts of the body, including bronchial and retroperitoneal. The course of chronic lymphadenitis is very diverse, which depends on the stage of the disease, the number of affected lymph nodes, the reaction of the tissues surrounding the node, etc. The diagnosis of inflammation of the lymph nodes is established only during a medical examination. Self-treatment is also contraindicated.
Elena Averkina
, oncologist, Nyagan City Clinic
Diagnosis of lymphadenitis
Recognizing acute lymphadenitis is not difficult. To make a diagnosis, anamnesis and a set of symptoms are studied. Difficulty can arise when infection of the lymph nodes is complicated by other concomitant diseases. In all cases, it is first necessary to determine the location of the primary purulent focus. In case of chronic disease, the patient is prescribed a puncture biopsy of the lymph node and histology.
To diagnose lymphadenitis, a general blood test is required. Based on its results, they judge not only the presence of the inflammatory process, but also its scale. Laboratory signs of lymphadenitis will be an increase in the total number of leukocytes and an increase in the erythrocyte sedimentation rate. With an active purulent process, a decrease in the level of monocytes and eosinophils is detected.
Diagnostic examination involves instrumental methods - ultrasound. With its help, you can determine the shape and size of the lymph nodes, their connection with surrounding tissues, and the presence of an abscess. If necessary, computed or magnetic resonance imaging and x-ray contrast lymphography are used.
Nonspecific lymphadenitis should be differentiated from other diseases, such as lymphogranulomatosis, leukemia, juvenile rheumatoid arthritis, chronic granulomatous disease, systemic lupus erythematosus, as well as metastases from malignant tumors.
Treatment of lymphadenitis
Treatment of inflamed lymph nodes is carried out in two directions:
- determining the source of the inflammatory process and eliminating it;
- relief of chronic and acute inflammatory process in the lymph node.
First of all, it is necessary to take measures to eliminate the underlying disease that led to infection of the lymph nodes. If purulent inflammation develops, the patient is hospitalized in a hospital, where the abscess is surgically opened.
What situations can lead to a reaction of the inguinal lymph nodes? First of all, these are various inflammatory diseases of the pelvic organs (mainly the reproductive and urinary systems), external genitalia, perineum and thighs. This may be infection of skin lesions, local inflammation in the form of a boil or carbuncle, erysipelas of the lower extremities, fungal infection, syphilis or herpetic infection, bacterial or viral disease of the genitourinary tract - chlamydia, ureaplasmosis, tuberculosis and others, primary damage to the lymph nodes with tularemia, plague, as well as generalized infections – HIV infection, tick-borne rickettsiosis and others.
There are other inflammatory diseases that lead to enlargement of the lymph nodes, but they are all accompanied by a different clinical picture, where inguinal lymphadenopathy is far from the first place. Palpable lymph nodes should always alert the doctor, because often malignant tumors metastasize to the lymph nodes, and generalized blood tumors (leukemia) and local tumors of the lymphatic system (lymphomas and lymphogranulomatosis) are always accompanied by damage to the lymph nodes. Metastases to the inguinal lymph nodes can give rise to tumors of the external and internal genital organs: uterus, ovaries, prostate, bladder; the skin itself (melanoma), rectum. The main manifestation, as the name suggests, is enlarged lymph nodes. However, it is especially important to identify additional symptoms, which can provide necessary information for further diagnosis. Detection of visible inflammatory changes in the skin or external genitalia, urination disorders, and pathological discharge from the urinary or genital tract most likely indicate an infectious etiology. Frequent changes of sexual partners and neglect of barrier methods of contraception indicate the possibility of contracting sexually transmitted infections (syphilis, HIV, chlamydia, trichomoniasis, gonorrhea).
A tumor etiology can be suspected in the presence of symptoms of chronic intoxication - prolonged low-grade fever, sweating, weight loss, weakness, coagulation disorders with multiple hemorrhages and many others, as well as most often dense, painless lymph nodes. Diagnosis and treatment of inflammatory diseases associated with inguinal lymphadenitis in men is carried out by a urologist and andrologist, and in women by a gynecologist and urologist, and for specific infections, consultation with an infectious disease specialist may be indicated. Suspicion of tumor processes requires a consultation with an oncologist.
For diagnosis, it is especially important to identify additional symptoms during a conversation and physical examination. Additional methods of laboratory and instrumental diagnostics include a general analysis of urine, blood, biochemical blood test, taking samples for testing for bacterial, viral and fungal infections, cystoscopy (examination of the bladder cavity), vaginal examination in women, rectal examination, ultrasound, MRI , CT and other imaging methods of the pelvic organs and other areas to search for the primary tumor, the use of cytological and histological (biopsy) methods to verify the diagnosis (if a tumor is suspected).
Treatment of inguinal lymphadenitis itself is possible when the nature of the underlying disease is established. For inflammatory diseases, most often this is drug therapy - antibacterial drugs, antiviral and antifungicidal drugs are used to treat inflammation. The prognosis for inguinal lymphadenitis is favorable in most cases.
Drug treatment: drugs most often prescribed
Treatment is complex and includes the use of various groups of medications. It is customary to use the following drugs for lymphadenitis:
- Antibiotics. To eliminate the source of infection (Amoxicillin, Cefazolin, Cefuroxime, Vancomycin, Lincomycin).
- Analgesics. To eliminate pain syndrome (Tramadol, Trimeperidine).
- Non-steroidal anti-inflammatory drugs. They have antipyretic and anti-inflammatory effects (“Ketoprofen”, “Ibuprofen”, “Paracetamol”).
- Antihistamines. Helps relieve the inflammatory process (Cetirizine).
- Antiseptics for topical use (Vishnevsky ointment).
In addition to drug treatment, physiotherapy methods are used - UHF. Ultrahigh-frequency therapy accelerates the elimination of the inflammatory process and enhances local tissue immunity. This method of treatment is contraindicated when the patient has a persistent increase in body temperature, has a tumor process, tachycardia, or muscle pain.
Frequently asked questions about lymphadenitis
What is submandibular lymphadenitis?
This is an inflammation of the lymph nodes that are located under the lower jaw. This form of the disease develops in the presence of an infectious focus in the oral cavity. This could be caries, periodontitis, gum disease, tonsillitis. It is accompanied by symptoms such as pain at the location of the node and redness of the skin above it, increased body temperature, pain during eating and during conversation, general malaise, and headache.
How long does it take to treat lymphadenitis?
The duration of treatment for the disease depends on a number of factors: the form of the disease; the presence of a purulent process; causative agent of lymph node inflammation. To completely eliminate the inflammatory process and eliminate pathogenic microbes in uncomplicated lymphadenitis, the course of treatment will be about two weeks. In the chronic form of the disease, therapy is long-term.
Is it possible to warm a lymph node?
Thermal effects on the inflamed lymph node are allowed when the inflammatory process has not yet been complicated by the formation of pus. It is believed that warming compresses with camphor oil or infusion of medicinal herbs help relieve pain and inflammation. However, you should consult your doctor before undertaking warming procedures, as such actions may worsen the infection. If the skin over the inflamed lymph node is red, then warming it is contraindicated, as this is a sign of suppuration.
Why does lymphadenitis occur?
Like any inflammation, lymphadenitis occurs due to the activity of bacteria: streptococci and staphylococci. The causes of submandibular lymphadenitis are diseases of the oral cavity and infection that enter directly into the lymph nodes as a result of diseases such as:
- caries, pulpitis, periodontitis;
- gum disease;
- chronic diseases (for example, tonsillitis);
- syphilis bacteria;
- tuberculosis bacillus;
- external infections that enter the body as a result of injury.