Every third appeal to an oncologist on social networks or on remote consultation portals is formulated something like this: “save, help, I have enlarged lymph nodes.”
As a rule, young people write, usually from 18 to 25 years old, and I don’t remember a case when it eventually turned out that the situation required treatment from an oncologist. Most often, enlarged lymph nodes were caused by a sore tooth, sore throat, conjunctivitis, and so on.
It is clear that fear and fears for one’s health in such cases force one to immediately run to an oncologist.
However, is everything so simple, and is it worth rolling your eyes about any treatment with an enlarged lymph node?
My personal statistics show: if a person comes for a face-to-face consultation, he is already one of those few whose situation was not limited to the banal “it got sick and went away.”
Let's take a closer look at how the lymphatic system works and understand the nature of enlarged lymph nodes.
Fact #2
Lymphatic vessels are not something abstract.
It is worth crossing or ligating them, for example, during surgery on the axillary lymph nodes for breast cancer, and lymphostasis is likely to develop - swelling of the limb, which, again, most likely will not go away.
The most visible to us from the point of view of examination - the so-called peripheral lymph nodes (in the neck, supraclavicular, axillary and inguinal) can increase, and this is in most cases a manifestation of reactive lymphadenopathy - an inflammatory reaction indicating the fight against infection.
Prevention and treatment of lymphadenopathy in Makhachkala
The essence of treatment for lymphadenopathy is to identify and treat the underlying disease. For example, if the pathology of the lymph nodes is caused by a bacterial disease, then a course of antibacterial therapy is prescribed. If the cause of lymphadenopathy is a viral infection, then antiviral treatment is carried out accordingly; in case of oncology, a complex of antitumor measures, etc. When choosing a treatment regimen, the doctor is guided by the individual characteristics of the patient’s body and the results of the examination. Self-medication is strictly prohibited. And the use of folk remedies is possible only in agreement with the attending physician. special measures to prevent lymphadenopathy in children . But the following will help minimize the likelihood of developing lymph node pathology:
- active lifestyle;
- good nutrition;
- increasing immunity;
- outdoor games;
- preventing frequent colds.
Parents are also required to take care of the child’s health, including timely visits to the doctor.
Fact #3
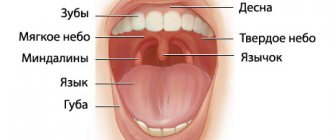
Most often, the cervical and submandibular lymph nodes become inflamed, because in the facial part of the skull there are many open mucous membranes and associated infections.
A sore throat, carious or rotten teeth, and ear and eye bacterial and viral infections are the most common causes of cervical lymphadenopathy. The axillary and inguinal nodes react according to the same principle.
Therefore, if a lymph node is bothering you, first of all you need to go to a therapist, dentist, or ENT doctor.
If the genesis of lymphadenopathy is unclear, the doctor will prescribe an ultrasound, and during this study, attention will be directed mainly not to the size of the lymph node, but to its shape and differentiation of the structure.
- Gallery
- Reviews
- Articles
- Licenses
- Vacancies
- Insurance partners
- Partners
- Controlling organizations
- Schedule for receiving citizens for personal requests
- Online consultation with a doctor
- Documentation
Lymphadenopathy is an increase in size, as well as a change in the shape of one or an entire group of lymph nodes of various origins, without signs of inflammation.
A person has about 600 lymph nodes. Normal sizes are up to 1 cm. The cervical, axillary, inguinal, and intra-abdominal lymph nodes are more often enlarged. Playing a protective role, lymph nodes are among the first to stand in the way of the spread of infections and other foreign antigens (allergens, tumor cells, etc.).
Until a child reaches 12 years of age, the lymphatic system is considered immature, although its formation begins in the early prenatal period. This explains the high incidence of lymphadenopathy among pediatric patients.
Among the causes of enlarged lymph nodes, infectious diseases occupy first place, then systemic diseases of connective tissue, and blood diseases.
Fortunately, lymphadenopathy of a specific tumor nature in children makes up no more than 10% of the total morbidity. A malignant form of the tumor process, which predominates in childhood, is lymphosarcoma. Rarely, enlarged lymph nodes in children occur with severe allergic reactions and helminthic infestations. You need to know that the use of a long course of certain antibiotics and antifungal drugs can provoke the development of a generalized form of lymphadenopathy, the signs of which gradually disappear after discontinuation of the drugs.
Infectious causes of enlarged lymph nodes are varied - these are:
- viruses;
- bacteria;
- fungi;
- parasites.
Infectious diseases that most often occur with enlarged lymph nodes:
- viral (Epstein Barr virus, cytomegalovirus, other herpetic viruses, measles, rubella, viral hepatitis, HIV);
- parasitic (toxoplasmosis, etc.);
- chlamydial infection;
- mycoplasma infection;
- fungal diseases (scarlet fever, diphtheria, tick-borne borreliosis, listeriosis, yersiniosis, etc.);
- mycobacterial (tuberculosis).
If an infectious cause of enlarged lymph nodes is suspected, an epidemiological history is important:
- contact with domestic animals (for example, cats);
- eating undercooked meat, raw water;
- going out into nature;
- swimming in ponds;
- visiting exotic countries.
If lymph nodes are enlarged, you should contact the following specialists:
- infectious disease specialist;
- hematologist;
- surgeon;
- oncologist (if necessary).
Services and prices
Primary appointment (examination, consultation) with an infectious disease specialist
2,200 rub.
Repeated appointment (examination, consultation) with an infectious disease specialist
2,100 rub.
Primary appointment (examination, consultation) with a pediatric surgeon
2,200 rub.
Repeated appointment (examination, consultation) with a pediatric surgeon
2,100 rub.
Ultrasound examination of lymph nodes
1,300 rub.
Isaev Andrey Aleksandrovich Head of Department, pediatric surgeon Doctor of the highest category Work experience: 43 years
Make an appointment
Fact #5
Lymph nodes enlarge during cancer because cancer cells enter the lymphatic vessels draining a certain area, which then settle in the “filters” (lymph nodes) in the form of metastases and begin to grow there.
Such lymph nodes do not shrink after treatment of infectious diseases, but only increase, merging with other lymph nodes into conglomerates, extending beyond the lymph node and fixing it in the surrounding tissues. Such lymph nodes are rarely painful, they are dense, very dense.
Often in cancer, lymph nodes are affected by a “chain” that is clearly visible on palpation. With lymphomas, conglomerates are often visible from the outside. Of course, with such manifestations you need to go to an oncologist and hematologist.
For suspicious nodes, a biopsy will be performed in the absence of other causes. This is either a puncture with a needle and collection of material, or an operation to completely remove the lymph node for histological examination.
Diagnostics
To establish the true causes of enlarged lymph nodes, you need to undergo a comprehensive diagnostic examination in a clinical setting. First of all, it is necessary to conduct a thorough history taking to establish the cause of the enlarged lymph nodes in the child. Next, a study is carried out to determine the presence of tumor formations, skin lesions, and the presence of inflammatory processes.
In our medical network clinics in Makhachkala, various types of laboratory and instrumental studies are carried out. To identify the causes of lymphadenopathy in children, specialists usually conduct a set of diagnostic examinations, which includes:
- general and biochemical blood tests;
- general urine analysis;
- X-ray of the chest area;
- ultrasound examination of internal organs;
- magnetic resonance imaging (MRI);
- computed tomography (CT);
- lymph node biopsy with histological and cytological analysis.
Consistency of lymph nodes
Dense lymph nodes, especially if accompanied by redness, increased local temperature, fluctuation, are often detected in infectious diseases.
Dense lymph nodes and without redness are often detected in viral infections and systemic diseases [5].
Dense, hard, immobile lymph nodes are a finding in malignant diseases.
Normally, the lymph nodes are soft, elastic, mobile (easily displaced upon palpation).
Consolidation of the lymph nodes may be associated with fibrosis or hemorrhage into it, immobility and cohesion are possible with the germination of metastases, or inflammation of surrounding tissues (tuberculosis, sarcoidosis).
Enlargement of lymph nodes can be generalized (enlargement or change in 2 or more unrelated groups of lymph nodes). Often generalized lymphadenopathy is accompanied by an enlarged liver and spleen, and a rash may be present. Generalized lymphadenopathy is not always a sign of serious pathology [5].
Localized lymphadenopathy is often found in children (palpation of the cervical, less often inguinal lymph nodes).
Most often, lymphadenopathy is localized and affects the nodes of the neck and head (3:1) [7].
In most cases, lymphadenopathy resolves on its own or after adequate treatment [5]. If lymphadenopathy does not resolve within 3–4 weeks, it is advisable to consider additional testing [5].
Diagnosis and treatment
The doctor makes the diagnosis based on external symptoms and accompanying complaints of the patient. Most often, the disease affects the glands on both sides. Sometimes the symptoms of the disease practically do not appear, except for inflammation of the salivary glands. Once ill, a small patient may refuse to eat, he may experience dry mouth and inflammation behind the ears.
The child is hospitalized only in case of complications or an epidemic. At home, the patient must be isolated from family members for 10 days and kept in bed.
It is necessary to adhere to a dairy-vegetable diet, grind food to reduce pain when swallowing, eat in small portions and drink plenty of warm teas, decoctions, and fruit drinks. You should avoid sour juices and fatty foods.
Doctors often prescribe:
- antipyretic,
- antihistamine,
- vitamins.
Gargling with a soda solution and dry warm compresses applied to the throat area are indicated. To relieve pain, you can tie a warm scarf around your neck and make a warm oil compress with heated vegetable oil.
In some cases, the doctor prescribes physical therapy, for example, ultraviolet radiation, diathermy. In severe cases, intravenous detoxification therapy with glucose solution is prescribed.
You can get a referral for them and undergo them at the children's clinic or at the SANMEDEXPERT clinic in Moscow Central Administrative District at the Baumanskaya metro station.
Prevention
To avoid mumps, a vaccination is necessary, which is done in any children's clinic according to the vaccination calendar, that is, after a year, often together with the measles and rubella vaccine. However, if a child has a decrease in immunity, for example, with leukemia, then the vaccine is contraindicated. Vaccinations for small allergy sufferers are given with special care. Normally, vaccination should be carried out under the supervision of an allergist.
Lymphadenopathy in children: key diagnostic points 03/21/2016
Lymphadenopathy in children: key diagnostic points
Larisa Anatolievna Peresada, pediatric hematologist, Candidate of Medical Sciences, receives consultations at:
Children's clinic, Kyiv, st. Tatarskaya, 2-E
Children's clinic on the Left Bank, Kyiv, st. Dragomanova, 21-A
Lymphadenopathy is a condition of hyperplasia (enlargement) of lymph nodes. This term is a preliminary diagnosis that requires further clarification during clinical and laboratory examination and dynamic observation.
The main causes of lymph node hyperplasia in children can be grouped into the following groups:
- infectious, which in turn are of a viral, bacterial, fungal, parasitic nature,
- associated with a malignant disease (leukemia, lymphoma, solid tumor metastases),
- as part of immunological disorders: hemophagocytic lymphohistiocytosis, Langerhans cell histiocytosis, Kawasaki syndrome, as well as in autoimmune diseases: autoimmune lymphoproliferative syndrome, systemic lupus erythematosus, juvenile idiopathic arthritis, sarcoidosis, congenital immunological defects,
- congenital metabolic diseases - storage diseases (for example, Niemann-Pick disease, Gaucher disease),
- associated with taking certain medications (phenytoin, hydralazine, procainamide, isoniazid, allopurinol, dapsone).
In the process of differential diagnosis, it is fundamentally important for the doctor to answer a number of questions. Are the lymph nodes really enlarged? Are we talking about localized or generalized lymph node hyperplasia? Does the process progress over time? Is there evidence to support an infectious etiology? Is there a suspicion of a malignant process? For example, the location of the lymph nodes - supraclavicular - always gives reason to suspect a malignant etiology. The most common task in pediatric practice is the need to distinguish the infectious from the malignant nature of lymph node hyperplasia. For this, there is a certain step-by-step algorithm, since it is not clinically possible in all cases to distinguish the age norm of the post-infectious state of the lymph nodes.
So, the signs of typical physiological lymph nodes under the age of 10 years: palpable in the cervical, submandibular, inguinal areas, size less than 1 cm (submandibular less than 2 cm), soft-elastic consistency, mobile, painless.
In children, the infectious etiology of lymphadenopathy is found in most cases. In this case, both a local infection and a systemic infectious process can lead to enlargement of the lymph nodes.
Signs indicating the infectious nature of the condition:
- visible local entrance gates of infection (teeth, tonsils, aphthae on the oral mucosa, traces of scratching in allergic dermatitis, other skin lesions),
- local pain/hyperemia (redness),
- there is an indication of a systemic childhood infection (for example, rubella, scarlet fever).
The primary assessment, as already mentioned, is to identify the location of enlarged lymph nodes. It is important to determine whether the lymph nodes of one group are hyperplastic or whether the process is widespread. In children, the neck area is most often involved. In this case, bilateral (two-sided) damage to the lymph nodes of the neck is characteristic mainly of viral etiology (adenovirus, cytomegalovirus, Epstein-Barr virus, herpes virus type 6, HIV), and a similar picture can occur with streptococcal sore throat. Acute unilateral damage to the lymph nodes in the neck area is predominantly characteristic of the staphylococcal nature of the disease, while the entrance gate of infection is the tonsils.
Subacute (chronic) course of the disease occurs, for example, with cat scratch disease, atypical mycobacteria, tularemia (which is rarely remembered, but there are currently facts of registration of this disease in Europe).
Auxiliary for diagnosis are a hemogram (general blood test) + ESR, determination of C-reactive protein, as well as ultrasound of the lymph nodes. Both blood tests and ultrasound images have their own characteristics during the inflammatory process.
One of the stages of the differential diagnosis algorithm is the prescription of antibacterial therapy, which is justified and appropriate for hyperplasia of the cervical group of lymph nodes. With an infectious etiology, the undoubted effect occurs within 10-14 days. This situation is interpreted as lymphadenitis.
The average observation period usually lasts 2 weeks. This time is enough to determine whether regression has occurred, whether the condition remains unchanged, or whether the disease is progressing.
If there is no positive dynamics on your own or after antibiotic therapy, or it is initially difficult to explain the hyperplasia of the lymph nodes with a clear infectious cause, the algorithm provides for the expansion of diagnostic measures. These include:
- determination of the level of LDH (lactate dehydrogenase), ferritin, uric acid in the blood, because an increase in these parameters may be indirect markers of a neoprocess;
- in-depth search for infectious agents that sometimes cause a subacute/chronic state of lymph node hyperplasia (with an appropriate history and clinical picture!) - examination for Epstein-Barr virus, cytomegalovirus, herpes virus type 6, as well as bacteria that cause cat scratch disease, brucellosis;
- HIV testing - if lymphadenopathy persists for more than 1 month;
- Mantoux test;
- Ultrasound + Dopplerography of the involved group of lymph nodes;
- Ultrasound of the abdominal organs;
- X-ray of the chest organs.
Here is an indicative diagnostic scheme, which is subject to correction in each specific case.
Particular attention is paid to lymph nodes more than 1.5 cm in diameter, dense on palpation, especially if they are accompanied by the so-called B-symptoms. It should be clarified here that B-symptoms include: a) profuse night sweats, b) an increase in temperature over 38°C, c) a decrease in body weight by 10% or more within 6 months. Such symptoms can be recorded with tuberculosis, AIDS, invasive intestinal diseases (amoebiasis, for example), and Hodgkin's lymphoma. As a rule, in such situations there is no time for observation, and it is advisable to perform an open biopsy of the lymph node for diagnostic purposes.
In addition, there are cases when lymph node hyperplasia is accompanied by changes in blood tests - anemia and thrombocytopenia. If autoimmune diseases and congenital immune defects are excluded, a bone marrow puncture is necessary for diagnostic purposes.
The review does not list all, but the most common causes of lymphadenopathy. It is also important to remember that the knowledge and clinical experience of the doctor is sometimes more important than the pedantic implementation of the schemes, and the diagnosis for each patient may have individual characteristics.
Based on materials from the German Society of Pediatric Oncology and Hematology:
Minisymposium on infectious diseases in children (University Hospital Bern, Switzerland, 2012)
Management of Lymphadenitis Minisymposium Infectiologie 25. October 2012.
Child's age
Lymph nodes are usually not identified/palpated in newborn babies due to their small size and soft consistency.
In young children, cervical, axillary and inguinal lymph nodes can be identified.
In children under 5 years of age, during a routine examination by a pediatrician, palpable lymph nodes are detected in 44% of cases, in children with any diseases - in 64% of cases [2].
The presence of palpable lymph nodes is not always a manifestation of any pathology. And also palpable formations may not be lymph nodes at all, but, for example, a congenital anomaly (cyst, hygroma).
Normally, lymph nodes in children grow until 8-12 years of age, then decrease slightly [3].
Localization of lymph nodes
When lymph nodes are enlarged, it is important to determine the cause/source of the changes. Palpation of inguinal or axillary lymph nodes is unlikely to be associated with the disease, cervical - possibly supraclavicular - probably (further assessment and differential diagnosis are required) [2].
Often, enlargement of the supraclavicular lymph nodes on the right is associated with a tumor or infection of the mediastinum, and on the left – with metastases of an abdominal tumor. When palpating the supraclavicular lymph nodes, an additional examination is recommended - CT or MRI of the chest [5]. Read more in the article “Management of lymphadenopathy in children.”
Lymph node size
Often the exact size of the lymph nodes is difficult to determine by touch. The size largely depends on the specific group of lymph nodes.
In principle, any lymph node, if it is detected by touch, is already considered enlarged. However, some groups of lymph nodes filter lymph from large areas of the body and can be detected even in healthy children [4].
Thus, in children, cervical, occipital, posterior ear, axillary lymph nodes can be palpated - no more than 0.5 cm - cervical, submandibular - no more than 1 cm, inguinal - no more than 1.5 cm. Occipital and posterior ear lymph nodes can more often be detected in small children, cervical and inguinal - in children over 2 years old.
Lymphadenopathy is a condition characterized by an increase in lymph nodes in size and/or quantity and/or a change in their consistency.
According to many observations, the incidence of enlarged lymph nodes depending on age is [4]:
| Occipital | Posterior ears | Submandibular | Cervical | Absence | |
| 0—6 months | 32% | 13 | 2 | 2 | 62 |
| 7-12 months | 26 | 13 | 3 | 26 | 52 |
| 1 year | 10 | 7 | 18 | 28 | 52 |
| 2 years | 8 | 6 | 20 | 45 | 32 |
| 3 years | 7 | 0 | 26 | 33 | 41 |
| 4 years | 0 | 0 | 25 | 55 | 35 |
| 5 years | 0 | 5 | 21 | 63 | 26 |
Normal size of lymph nodes
It is believed that lymph nodes should be up to 1 cm in diameter (but definitely not exceed 2 cm [2]), inguinal - up to 1.5 cm, ulnar, behind the ear - up to 0.5 cm [5,6].
These sizes are not strict, especially for children in the first years of life (babies are just encountering different antigens and developing their immunity, more details in the article “Causes of enlarged lymph nodes”).
When assessing lymph nodes, it is also necessary to evaluate their consistency, mobility, shape, density, and changes in the skin over the surface.