In some cases, tonsils may become enlarged without fever. Enlarged tonsils without fever require the same attention and treatment approach to avoid the development of complications.
Author:
- Chuprikov Roman Sergeevich
ENT pathology expert
3.45 (Votes: 33)
Tonsils (tonsils) are an important organ of the human immune system, involved in protecting the body from harmful carriers and preventing their spread. Their main task is to identify pathogenic microorganisms and produce antibodies to fight them.
Enlarged tonsils themselves are not a disease, but a symptom. They can increase:
- with infection;
- with genetically determined hypertrophy;
- for blood diseases (lymphoproliferative diseases);
- for autoimmune diseases;
- for allergic inflammation and swelling.
Usually these processes are accompanied by an increase in temperature, but in some cases the tonsils can enlarge without an increase in temperature. This often forces one to delay a visit to the doctor, since temperature is considered a marker of the disease. But enlarged tonsils without fever require the same attention and treatment approach to avoid the development of complications.
Under what conditions can tonsils be enlarged without fever?
Without an increase in temperature, the tonsils can become inflamed due to:
- Allergies. Enlarged tonsils often occur in people prone to allergies. Allergens include various substances - animal hair, dust, pollen, food, insects, household chemicals.
- Fungal infection. The following symptoms are observed: sore throat, dry mouth, visible cheesy coating on the mucous membrane.
- Dry air. Due to constant inhalation of dry air, the mucous membrane of the larynx dries out, causing the tonsils to swell. Working in polluted conditions also leads to this.
- Smoking. Tobacco smoke burns the mucous membrane, which can result in swelling of the tonsils.
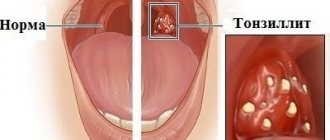
- Some forms of sore throat (tonsillitis). The biological meaning of an increase in temperature during infectious diseases is to accelerate the death of pathogenic carriers in an environment with high temperatures. Consequently, if the body temperature has not increased, it means that the number of infectious carriers that have entered the body is small. Usually, if the infection was minor, then the person easily and quickly suffers from this illness. But with enlarged tonsils and no temperature, we can talk about an untreated acute inflammatory process in the tissues of the tonsils and its transition to chronic. In this case, the recovery process will take longer, and in addition, there is a possibility of complications developing. Both variants of pathologies require examination and prescription of correct treatment by an otolaryngologist.
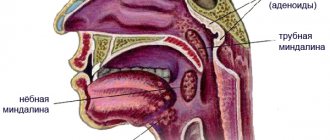
The structure of the tonsils and their number
Tonsils or otherwise tonsils consist of lymphoepithelial porous tissue. They are located in the nasopharynx in a circle and are part of the Pirogov-Waldeyer (pharyngeal-lymphatic) ring.
They are divided into paired and unpaired, there are 6 of them in total. The first group includes:
- Palatal. They are located on both sides of the pharynx in a depression formed by the tongue and soft palate.
- Pipe. Located next to the auditory tube.
Unpaired formations:
- Pharyngeal or nasopharyngeal. Located on the posterior fornix of the pharynx.
- Lingual. The location is the back of the root of the tongue.
Functions of the tonsils:
- Barrier. They trap and neutralize bacteria and viruses.
- Immunogenic. B and T lymphocytes are formed in the follicles of the tonsils.
- Hematopoietic. Active during the neonatal period.
- Enzymatic. The tissues of the organs secrete some enzymes necessary for the initial stage of digestion in the oral cavity.
The tonsils are also involved in the formation of voice timbre, so their defeat leads to hoarseness.
Features of the condition with enlarged tonsils without fever
Even at normal body temperature, but in the presence of pathological processes in the body, a person may feel completely unwell. Inflammation of the tonsils without fever, regardless of the cause, can interfere with a normal lifestyle and be accompanied by:
- headache;
- sore throat;
- lack of appetite;
- difficulty swallowing;
- dryness and sore throat;
- enlarged lymph nodes and pain on palpation;
- fatigue, weakness, drowsiness, decreased performance, irritability.
Chronic tonsillitis during pregnancy
It is very important to pay attention to the disease during pregnancy. When planning a pregnancy, even in the case of a compensated condition, that is, a condition outside of an exacerbation of tonsillitis, it is highly advisable to carry out a planned course as prescribed by a doctor. This will reduce the bacterial load on the entire body in general and on the palatine tonsils in particular.
It is very encouraging that doctors are now referring pregnant women and women who are just preparing for pregnancy for treatment of tonsillitis. Unfortunately, in some cases one of the reasons for not carrying a pregnancy to term is this disease, although at first glance it is hard to believe, tonsillitis is a traffic jam, the treatment of which and other manifestations may seem in no way related to pregnancy.
Before conceiving a child, it would be correct to examine the future father of the child for the disease and, if necessary, treat it as well. This will significantly reduce the risk of developing chronic tonsillitis in the unborn child. And, on the contrary, the worse the condition of the future father and especially the mother, the risk of developing the disease in the child increases many times over.
Before pregnancy, it is very important to carry out comprehensive treatment of the symptoms of chronic tonsillitis. But even during pregnancy, it is recommended to repeat the course, preferably in the second trimester, when the woman’s condition is perhaps the most comfortable. It is important to note that physiotherapeutic procedures cannot be carried out during pregnancy, but it is highly desirable to wash the palatine tonsils using a vacuum method, followed by treatment with antiseptic solutions.
Treatment of enlarged tonsils without fever
Before prescribing treatment, it is necessary to establish the cause of inflammation of the tonsils.
If the cause is an infectious or fungal infection, then the patient is prescribed a course of antibacterial therapy, treatment of the throat and mucous membranes with special preparations, infusions into the larynx, rinsing the tonsils, and taking vitamin complexes to support the immune system.
If conservative treatment is ineffective, a tonsillectomy may be prescribed - surgical removal of the tonsils. Most often, this is an indication for the treatment of chronic tonsillitis, which occurs with toxic-allergic manifestations and seriously interferes with a person’s comfortable life.
If swelling of the tonsils is associated with external factors - smoking, working in unsuitable conditions, attacks by allergens, the doctor will advise correction of lifestyle or environmental conditions, and taking supportive medications.
Causes
The development of the disease is closely related to frequent sore throats (acute tonsillitis). Very often, incompletely cured tonsillitis leads to chronic tonsillitis. Very often, tonsillitis is an exacerbation due to the accumulation of plugs in the tonsils - caseous-necrotic masses, which are often confused with food debris.
Main reasons for development
- Unfavorable working conditions. The greatest influence is exerted by gas and dust levels in the air at work.
- Poor environmental conditions, pollution from vehicle exhaust gases, harmful emissions into the atmosphere.
- Low quality of consumed water.
- Weak (low) immunity.
- Severe hypothermia of the body.
- Stressful situations.
- The presence of chronic diseases in the nasal cavity, paranasal sinuses and oral cavity - dental caries, purulent sinusitis, etc., which often leads to infection of the tonsils.
- Irrational or poor nutrition, in which excess amounts of proteins and carbohydrates are consumed.
- Heredity (mother or father suffers from chronic tonsillitis). It is very important for a woman to undergo one or two courses of treatment for tonsillitis during pregnancy (depending on the severity of the process) in order to minimize the likelihood of the disease developing in the unborn child.
- Frequent overwork, fatigue syndrome, inability to fully rest.
- Smoking and alcohol abuse.
Prevention
To prevent pathological enlargement of the tonsils, you must adhere to the following recommendations:
- Increase immunity: eat properly and well, exercise, exercise, give up bad habits, and maintain proper sleep patterns.
- Avoid provoking factors: do not overcool, humidify the air in the room, remove allergens from the environment.
- Treat infectious diseases promptly at the very beginning and prevent them from becoming chronic.
- Carry out preventive gargling and rinsing of tonsil lacunae. These procedures are carried out in our clinic, and our doctors will be happy to advise you about them.
If you are concerned about enlarged tonsils without fever, make an appointment with otolaryngologists at the Ear, Nose and Throat Clinic - you will receive comprehensive consultations and quality treatment.
What other tonsils are there in the pharynx?
Other tonsils that form the lymphoid pharyngeal ring are: adenoid vegetations, or, more simply, adenoids, which are not a paired organ. They are located in the dome of the nasopharynx. It is impossible to see them with the naked eye. In order to recognize the condition of the adenoids, it is necessary to perform an endoscopic examination of the nasopharynx. Inflammation of the adenoids is called adenoiditis and is more common in children.
Also in the pharynx there is a lingual tonsil, located at the root of the tongue, which, like the adenoids, is an unpaired organ.
There are also tubal ridges, which are also called tubal tonsils. They are located at the entrance to the pharyngeal mouth of the auditory tube. The tube ridges are located deep in the nasopharynx, on the lateral (medial) surfaces of the nasopharynx on the right and left. Tubal tonsils perform an important function - they protect against infection entering the auditory tube. Since each of the tonsils of the lymphoepithelial pharyngeal ring deserves separate close attention, in this article we will only talk about the palatine tonsils and chronic tonsillitis. Other tonsils and the pathology they cause will be described in detail separately, in other relevant ENT articles.
How is inflammation treated?
The tactics for treating enlarged tonsils in a child consists of treating the underlying disease that caused this symptom (taking antibiotics, antiviral or antifungal drugs), and influencing them directly to regenerate the affected tissues. The latter includes:
- washing the tonsils from pathogenic microorganisms and mucus with antiseptic solutions;
- reducing swelling - taking antihistamines and ultraviolet irradiation;
- UHF therapy, which improves blood microcirculation;
- exposure to ultrasound to free the lacunae of the tonsils from pus, which can accumulate in them;
- laser exposure to destroy infection and its pathogens.
Chronic tonsillar pathology occupies a special place among chronic lesions of the ENT organs. This is due to both the relatively rapid chronicization of the process in the palatine tonsils and the possibility of the development of generalized, even fatal, complications, as well as the peculiarities of the course and influence on the body of associated (metatonsillar) diseases. According to various authors, from 4 to 35% of the population suffer from chronic tonsillitis, while in different regions of the Russian Federation there is an increase in the number of patients suffering from this pathology.
Chronic tonsillitis, being a classic example of a focal infection, is essentially a chronic infectious-allergic disease with a local inflammatory reaction in the palatine tonsils, which makes it possible to develop a whole set of complications based on the activity of β-hemolytic streptococcus, its antigens and various pathogenicity factors , in which streptolysins play a key role.
It is known that most acute inflammatory diseases characterized by damage to the ENT organs, in the absence of adequate therapy, tend to become chronic. However, the pathology associated with the palatine tonsils has pronounced distinctive features both in the formation of chronic inflammation and in the strict phasing of the development of this pathological process. In the natural physiological functions of the palatine tonsils, normal and pathological processes interact so closely that, despite the large number of diverse studies that have been carried out on this problem, until now it has been practically impossible to establish an absolutely definite “point of no return” when irreversible pathomorphological changes occur in the structure of the palatine tonsils, and radical treatment methods, in particular tonsillectomy, are already required. The lack of a consensus solution on this issue in the modern medical community only further aggravates the problem.
Thus, very often in routine clinical practice, when choosing further tactics for patient management, doctors are guided primarily by anamnestic data on the number of sore throats and peritonsillar abscesses suffered, focusing more on subjective sensations than on objective clinical symptoms and data from laboratory research methods. Meanwhile, the currently existing classification of chronic tonsillitis B.S. Preobrazhensky—V.T. Palchun (and the diagnostic criteria embedded in it), developed at one time at the Department of Otorhinolaryngology of the Russian National Research Medical University named after. N.I. Pirogov, allows you to clearly differentiate various forms of chronic tonsillar pathology and gives a clear indication of further tactics for managing this patient [1, 2]. Unlike existing classifications of chronic tonsillitis, this classification reflects the stages of development of the pathological process in the structure of the palatine tonsils and the influence of these processes on the body as a whole in accordance with the main pathogenetic links of this disease. At the same time, the comments to this classification directly state the need to perform tonsillectomy in patients with chronic tonsillitis of the toxic-allergic form (TAF) II, as well as, in case of ineffectiveness of conservative therapy, in patients with chronic tonsillitis TAF I. However, despite this, it is regrettable to state that in the medical environment and especially in the therapeutic community, there is still an opinion about the need to preserve the palatine tonsils as an immunocompetent organ by any means, even despite the possible severity of general somatic symptoms and the obvious failure of the palatine tonsils in conditions of profound changes in its structure against the background of pronounced chronic changes .
That is why, when choosing a treatment method for a patient with chronic tonsillar pathology, it is necessary, first of all, to be guided by the knowledge that has been accumulated on this problem at present, and to objectively assess the risk of complications that can lead to the development of, including lethal symptoms, and the classification of chronic tonsillitis B.S. Preobrazhensky - V.T. Palchuna should be the main guideline for detailing the diagnosis and, on this basis, choosing tactics for further management.
The stages of development of pathomorphological changes in the structure of the palatine tonsils, as well as the formation of general and local associated diseases (metatonsillar complications), reflected in the classification of B.S. Preobrazhensky—V.T. Palchun, are largely determined by the biological properties of the main etiologically significant microorganisms [3].
According to the results of many studies conducted in recent decades, among the microorganisms that claim to be the leading etiological factor in the development of chronic tonsillitis, one can find a large number of pathogens with different properties, including streptococci, staphylococci, Haemophilus influenzae, lymphotropic viruses, etc. In accordance with According to the results of these studies, chronic tonsillitis is considered to be a polyetiological disease. Considering this issue from the perspective of clinical microbiology, it should be noted that in most cases, causally significant microorganisms are primarily bacteria growing in the distal parts of the crypts of the palatine tonsils. Since these sections of the tonsils have an extremely low oxygen content, the dominant flora growing on the surface of the mucous membrane of the tonsil crypts are microorganisms with an anaerobic type of metabolism, which are represented by peptococci and bacteroides. prevotella, fusobacteria, etc. However, the leading role in the development of chronic changes in the palatine tonsils, as well as local and general complications of chronic tonsillitis is given to β-hemolytic streptococcus of the serological group, A ( S
.
pyogenes
) - a microorganism that also uses anaerobic respiration for its life. At the same time, the palatine tonsils are the only natural reservoir of pyogenic streptococcus in the macroorganism [4, 5].
And it is this fact that in most cases determines the development of toxic-allergic manifestations in the human body, leading to the formation of common diseases associated with chronic tonsillitis. Among these diseases, acute rheumatic fever and post-streptococcal glomerulonephritis should be particularly highlighted, which, as a rule, lead to pathology of the cardiovascular and urinary systems, and also worsen the quality of life and, ultimately, shorten it [6-8].
S
.
pyogenes
are microorganisms that are gram-positive cocci, having a classic type of arrangement for streptococci - in the form of a chain, giving complete lysis of red blood cells (beta-hemolysis) on blood agar and belonging to the serological group, A in the antigenic classification of streptococci by R. Lensfield. Streptococcus pyogenes has significant resistance to physical and chemical environmental factors. The only natural reservoir of pyogenic streptococcus in the macroorganism is the distal sections of the lacunae of the palatine tonsils.
The pathogenesis of pyogenic streptococcal infections is associated with the activation of these microorganisms in the deep sections of the lacunae of the palatine tonsils, their subsequent invasion into the structures of the lymphoid tissue of the tonsils due to the presence of a large number of extracellular enzymes - streptokinase, which catalyzes the conversion of plasminogen into the proteolytic enzyme plasmin, hyaluronidase, which destroys hyaluronic acid, which is the main a component of connective tissue, streptodornase (DNAase), which destroys elements of the genome of connective tissue cells, etc. The production of membrane-damaging toxins O- and S-streptolysins specific to this pathogen leads to the development of systemic intoxication, cardiotoxicity, which is explained by the suppression of energy processes in the mitochondria of myocardial cells under conditions of O-streptolysin activity, which also has hemolytic activity and immunogenic properties. The action of S-streptolysin together with the antichemotactic factor (peptidase C5a) is associated with the suppression of the activity of phagocytic cells and the destruction of mitochondrial membranes of cells in the lesion. The specificity of clinical symptoms of damage to the palatine tonsils is primarily due to the action of these pathogenicity factors.
In addition, a feature of the cell wall of pyogenic streptococcus can be considered the presence of a large number of surface protein structures, in particular M-protein, which is an important adhesin of these microorganisms. M-protein ensures binding to collagen, fibronectin, as well as serum proteins - fibrinogen, components of the complement system, as well as other elements of various organs and systems, causing activation of the primary phase of development of metatonsillar complications. The ability of pyogenic streptococcus to penetrate into epithelial cells with the development of the phenomenon of internalization is associated with the presence of M-protein. Streptococcus pyogenes has a hyaluronic capsule that protects it from immunological surveillance authorities and is a factor in antiphagocytic activity.
In addition, S
.
pyogenes
has and synthesizes a large number of substances that have the properties of superantigens, cause mitogenic activity and lead to polyclonal proliferation of T lymphocytes. Superantigens of streptococci include pyrogenic exotoxins (SPE A, SPE B, SPE C, SPE D), the mitogenic factor SPE F and, probably, type-specific M proteins [2, 9]. Pyrogenic toxin, A (Spe A), whose gene is localized on a temperate bacteriophage, is associated with the most severe forms of streptococcal infection. The gene encoding this toxin is detected in ½ of cases of scarlet fever and rheumatic fever. The pyrogenic toxin B gene is localized in the chromosomal DNA of the cell and is a cysteine proteinase that is capable of breaking down fibronectin in the macroorganism. In patients with invasive forms of streptococcal infection (cellulitis, pneumonia, necrotizing fasciitis), there is an increased level of antibodies to pyrogenic exotoxin B (SPE B). In addition, the production of SPE B by streptococci was combined with a high risk of developing acute post-streptococcal glomerulonephritis [10, 11].
It has now been proven that streptococci can not only attach to the cells of the macroorganism, but also penetrate them. Thus, A. Osterlund [12], examining the tonsils of children with recurrent tonsillitis, identified streptococci located inside the cells, and 30% of failures in the treatment of chronic tonsillitis are associated with the presence of the pathogen intracellularly.
It should also be noted that β-hemolytic streptococcus persists in the structure of the mucous membrane of the crypts of the palatine tonsils not in the form of planktonic cultures, but in the form of pathological biofilms, which determine not only protection from exogenous environmental factors, but also resistance to various methods of therapeutic intervention [13, 14].
In the development of the stages of the clinical picture of tonsillitis (which are reflected in the classification of B.S. Preobrazhensky - V.T. Palchun), several factors associated with pyogenic streptococcus take part: 1) a toxic factor that determines the pathological effect of streptolysins on the cardiovascular, nervous and endocrine system, which is manifested by general intoxication, fever, etc.; 2) a septic factor, which is associated with the influence of enzymes of the pathogenicity of beta-hemolytic streptococcus, resulting in a local inflammatory reaction in the structure of the palatine tonsils and further invasion of microorganisms deep into the tissues with the possibility of further generalization of the process, often hematogenously, up to the development of tonsillogenic sepsis, severe reaction of lymph nodes, etc.; 3) an allergic factor (a complex of surface substances of pyogenic streptococcus), which causes sensitization of the macroorganism to beta-hemolytic streptococcus and antigens of destroyed body tissues, which then leads to the development of glomerulonephritis, myocarditis, etc. [2].
Analyzing all of the above, we have to state that the pathogenicity factors of streptococcus pyogenes and its biological properties directly affect the nature of the clinical course of tonsillar pathology and its complications, which proves the leading role of this microorganism in the genesis of chronic tonsillitis.
Features of the anatomical and histological structure of the palatine tonsils, along with the biological properties of pyogenic streptococcus, also make a significant contribution to the development of chronic inflammation in them. Being part of the lymphoepithelial pharyngeal ring, the palatine tonsils are not only the largest in size, but also the most complex structure among all the elements of this ring, which largely determines the development of a focus of chronic infection.
Thus, it is known that the palatine tonsil consists of lobules that have a complex structure. From different parts of the connective tissue capsule of the tonsil, bundles of connective tissue run towards the pharynx surface, forming the basis of the lobules (stroma). Then these main cords branch into smaller ones that penetrate the entire amygdala. The tonsil parenchyma is a group of lymphoid follicles located in a finely looped connective tissue network. In the center of such more or less rounded follicles there is a zone that, when preparing a microslide, has a lighter color - the so-called germinal center, where young lymphocytes are formed, which, as they develop, are gradually pushed towards the periphery of the follicle. An important feature of the palatine tonsils, which determines both normal physiological and pathological processes, is the presence of crypts. They begin on the pharynx surface and go deep into the tonsil, branching like a tree. The crypts, like the entire pharyngeal surface of the tonsil, are lined with stratified squamous epithelium in 6-8 rows.
In some places of the crypts the epithelial cover is interrupted (areas of physiological angization). Here contact between microorganisms and lymphocytes occurs. It is the areas of physiological angization that provide contact of microorganisms with the mantle zone of the follicles. Microorganisms growing on the surface of the crypts freely penetrate into the lymphadenoid tissue exposed in these breaks in the epithelium. In this way, a natural biological mechanism is formed that ensures the penetration of an infectious agent from the external environment into the lymphoid tissue of the tonsil, which leads to the initiation of the development of the germinal center of the follicles of the palatine tonsil, the differentiation of B-lymphocytes into highly specific plasma cells capable of synthesizing high-avidity antibodies. Immune control ensures the death of microorganisms that have penetrated into the parenchyma of the NM. In this case, the source of infection is inactivated by the general immune factors of the macroorganism. The bacteria die, but retain particles of their antigenic structure, which is an additional stimulus for the activation of local and general immunological reactions.
Recognition of antigenic structures of microorganisms also occurs due to Toll-like receptors. At the same time, a number of authors note that not only lymphocytes express Toll-like receptors (TLRs) on their surface, which play a key role in the recognition of microorganisms. These receptors are found in epithelial cells of the tonsils, primarily in the cryptal and luminal cells [15]. The detection of these receptors in the epithelium of the tonsils may indicate its functional role as antigen-presenting cells, and this also serves as confirmation that in conditions of a normally functioning tonsil, the lining of the crypts is not damaged.
Thus, the very structure of the amygdala, namely tree-like branching crypts with 4-6 orders, contributes to the formation of acquired immunity, increasing the time of contact of the pathogen with immune cells. However, in situations where the outflow of contents is delayed beyond a certain time, the lacunae acquire the ability to cystic expansion. Under these conditions, the crypt epithelium begins to be affected for a long time by toxins of microorganisms, which subsequently take a direct part in the formation of various toxic-allergic manifestations. That is why the delay in the outflow of the contents of the lacunae is one of the important mechanisms for the development of chronicity of the process, and also takes part in the genesis of associated pathology, the further systemic impact of the formed chronic focus of infection on the macroorganism and the formation of gross pathomorphological changes in the tissues of the tonsils themselves.
The starting point in the development of chronic tonsillitis is a violation of the local immune status of the mucous membrane of the palatine tonsils, which, together with the effects of bacterial toxins and sometimes lymphotropic viruses on the crypt epithelium, can lead to its thinning and the formation of areas of no longer physiological, but pathological angization. This allows etiologically significant microorganisms to penetrate into the deep cellular layers of the mucous membrane, deep into the tonsil parenchyma, into the blood vessels and initiate further pathological processes.
It should be noted that in modern literature there is little data on the changes that occur in the palatine tonsils at different forms and stages of chronic tonsillitis at the cellular level. The research conducted at our department helped to complement the understanding of the physiology and pathophysiology of the palatine tonsils in conditions of the formation of chronic inflammation in them. During the study, the autoradiography method was used to evaluate the histoarchitecture of the palatine tonsils, as well as to determine the functional activity of microorganisms located in the tonsillar parenchyma, both normally and in patients with chronic tonsillitis. The essence of the method was the use of radioactive precursors of nucleic acids (3H-thymidine, 3H-uridine). The accumulation of 3H-thymidine by the cell demonstrates the ability of these cells to synthesize DNA, i.e., indicates their proliferative activity. The synthesis of RNA, which is the template for protein synthesis, reflects the functional activity of the cell. In addition, the cell's ability to absorb and accumulate radioactive tracers makes it possible to differentiate viable bacteria and normally functioning tonsil cells from nonviable cellular debris.
According to the results of these studies, in the tissues of unchanged palatine tonsils, microorganisms were found exclusively on the surface of the mucous membrane of the crypts, while the epithelial cells of the palatine tonsils had a normal structure, were characterized by a normal nuclear structure, and the absence of pathological proliferative activity. In addition, in healthy palatine tonsils, only individual endothelial cells showed insignificant functional activity, i.e., they synthesized RNA.
During the formation of a chronic focus of infection and the development of toxic-allergic forms, on the contrary, a violation of the cytoarchitectonics of the tonsil tissue was observed: the growth of connective tissue into the lymphoid tissue, the appearance of individual foci of necrosis, signs of destruction of the walls of microcirculatory vessels, and necrotic changes in the epithelial lining of the crypts appeared. A characteristic feature of patients with toxic-allergic forms of chronic tonsillitis was the detection of microorganisms in the tonsil tissue. At the same time, microorganisms absorbed both 3H-uridine and 3H-thymidine, which indicated not only their functional (protein synthesis), but also proliferative activity. Moreover, some functionally active microorganisms were compactly located in the structure of the pathologically altered vascular endothelium. It is necessary to understand that the formation of connective tissue, microabscesses, granulations inside the parenchyma of the tonsils contributes to the isolation of microorganisms, as well as their resistance to conservative treatment methods. Pathomorphological changes that occur in the palatine tonsils lead to the loss of the immune function of the latter.
In addition, a detailed study of tonsil follicles using various immunohistochemical markers provides insight into the processes occurring in the tonsils at the cellular level. A study on the Ki-67 cell proliferation marker in patients with hypertrophic tonsillitis and a negative test for β-hemolytic streptococcus group A in comparison with patients with chronic tonsillitis and laboratory-confirmed streptococcal presence indicates a predominance of cell division in patients without an infectious process in the tonsils, in difference from patients with chronic tonsillar pathology associated with pyogenic streptococcus. At the same time, markers of apoptotic and anti-apoptotic activity demonstrate a picture of degenerative changes in the structure of the palatine tonsils in patients with chronic tonsillar pathology. Thus, changes in caspase-3, Fac/CD95, Fax suggest the predominance of cell death processes in the tonsils with chronic inflammation caused by a bacterial nature.
The expression of markers of anti-apoptotic activity, such as Bcl-2 and surferin, also demonstrates their predominance in the palatine tonsils of patients with chronic tonsillar pathology [16].
The penetration of pathogens into the tonsil parenchyma, in addition to the events described above, is characterized by a slight increase in the volume of lymphoid follicles, disorganization of reticular fibers, and subsequently their death with replacement by connective tissue and the development of a scar process [2, 17]. All this gradually leads to a decrease in the total area of active lymphoid tissue in the tonsil and contributes to the “burying” of microorganisms between scar tissue, and also creates conditions for the development of reactive complications of chronic tonsillitis.
Thus, chronic inflammation developing in the structure of the tonsils radically changes the cytoarchitectonics of the palatine tonsils, transforming them from functionally active immune structures into a dangerous focus of the infectious process in the body, leading to its sensitization and the development of toxic-allergic manifestations.
The issue of treatment of patients with chronic tonsillar pathology remains, perhaps, one of the most controversial in otorhinolaryngology. And if making a diagnosis of “chronic tonsillitis”, as a rule, does not cause difficulties, then deciding on the stage, phase, form of the disease and, as a consequence, the choice of treatment method, raises a large number of questions and is often based on the subjective feelings of the doctor.
Along with the classical bacteriological method for diagnosing chronic tonsillitis and identifying the pathogen, in recent years a large number of new methods have been developed not only for diagnosing chronic tonsillitis, but also for assessing the functional state of the tonsils.
A method for assessing the functional state of the palatine tonsils by cytological examination of the contents of their crypts in chronic tonsillitis is proposed.
E.V. Tyrnova and G.S. Maltsev propose a biochemical method for diagnosing chronic tonsillar pathology, based on the determination of C-reactive protein, rheumatoid factor and antistreptolysin-O in blood serum [18].
V.M. Tsirkunov et al. [19] propose a method for diagnosing the degree of activity and stage of chronicity of chronic tonsillitis, based on a biopsy of the palatine tonsils.
L.A. Dyukov et al. [20] propose a method for quantitative scoring of the state of intestinal microbiocenosis in patients with chronic tonsillitis with the determination of the dysbiosis index as a method of additional diagnosis of various forms of chronic tonsillitis.
However, none of these methods are widely used in clinical practice for various reasons. But it is the timely and correct determination of the form of the disease that guarantees success in treatment and protects the patient from complications.
In the current conditions, based on the polyetiology of chronic tonsillitis, the lack of a generally accepted instrumental or functional diagnostic method, the danger of developing local and general complications, the classification of chronic tonsillitis proposed by B.S. Preobrazhensky and V.T. Palchun, not only has not lost its relevance, but, on the contrary, is acquiring primary importance in the choice of treatment methods for this disease and makes it possible to establish strict indications for surgical treatment.
The undoubted advantage of the classification of chronic tonsillitis under consideration is its clear focus on the etiology, pathogenesis of the disease, the risk of developing concomitant and associated diseases, as well as a reflection of the stages of development of the process in the macroorganism both at the systemic and cellular levels.
Thus, with a simple form of chronic tonsillitis and the absence of signs of systemic changes in the macroorganism, courses of conservative therapy are possible.
In case of chronic tonsillitis TAF I degree, when microorganisms penetrate into the tonsil parenchyma and progressive inflammatory changes develop, leading to sclerosis of the parenchyma, the walls of blood vessels are damaged and their lumen increases, the patient is shown a test course of conservative treatment, including local (washing the lacunae of the palatine tonsils) and systemic antibacterial therapy. If success is achieved with this treatment, it may be continued. However, dynamic monitoring of the patient is necessary so as not to miss the moment of transition of the disease to the next form. If there is no effect from the test course of therapy, surgical treatment is indicated.
A characteristic feature of stage II TAF is the formation of microfoci of necrosis in the structure of the tonsillar, which leads to complete functional failure of the tonsil, expressed in atrophy and death of the follicles. In the tonsils, decay processes prevail, microbial cells are found in the lumen of blood vessels along with cellular and microbial detritus, and metatonsillar complications develop. With this form of chronic tonsillitis, there is no need to talk about the possibility of conservative treatment of a source of chronic infection in the body, and the only method to cure the patient and prevent the development of complications is to remove the tonsils.
A timely tonsillectomy not only cures the patient and protects him from serious complications, but is also cost-effective. In a study conducted in 2002 by N. Bhattachatyya and L. Kepnes [21], patients were observed after tonsillectomy (average follow-up duration 37.7 months). In addition to the subjective improvement in quality of life, during the 12 months after surgery, there was a decrease in antibiotic consumption by an average of 5.9 weeks per year. The number of days of disability associated with chronic tonsillitis decreased by an average of 8.7 days per year. The number of disease-related visits to the doctor decreased by an average of 5.3 visits per year. And taking into account all the economic costs of the operation, the break-even point occurs 2 years after the operation.
Even taking into account the obvious differences in the tactics of treating chronic tonsillitis, which are a consequence of fundamental differences in the issues of financing and organization of medical care, the place of scientific research in clinical practice, the capabilities of health insurance systems in Russia and abroad, the understanding of the inevitability of eliminating the source of infection for the patient’s health remains the same . In this case, the main guideline for deciding the choice of therapeutic treatment tactics or the need to perform tonsillectomy should be the form of chronic tonsillitis in accordance with the classification of B.S. Preobrazhensky–V.T. Palchuna. In this regard, and also taking into account the stated modern ideas about the etiology, pathogenesis and clinical picture of chronic tonsillitis, it is worth thinking about the need for widespread use of this classification in the practice of otorhinolaryngologists in Russia. We invite specialists to take part in a discussion on this issue on the pages of the magazine.
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Information about authors
Palchun V.T. — e-mail; https://orcid.org/0000-0002-3521-7424
Kryukov A.I. — e-mail; https://orcid.org/0000-0002-0149-0676
Gurov A.V. — e-mail; https://orcid.org/0000-0001-9811-8397
Ermolaev A.G. - e-mail; https://orcid.org/0000-0003-2642-5173
Corresponding author:
Gurov A.V. — e-mail: [email protected]
Palchun V.T., Kryukov A.I., Gurov A.V., Ermolaev A.G. Palatine tonsils: physiology and pathology. Bulletin of Otorhinolaryngology
. 2019;84(6):11-16. https://doi.org/10.17116/otorino20198406111
CONSEQUENCES OF TONSILLECTOMY
Tonsil removal surgery is successful in most cases. A huge role is given to the professionalism of the operating doctor, anesthesiologist and other specialists who monitor the patient’s well-being. If you contact a competent otolaryngologist, who has the necessary technical equipment, and follow the doctor’s recommendations before surgery and in the postoperative period, then the risk of complications is minimized.
When the first signs of malaise and deterioration in health appear, you should consult your doctor. Since the pharyngeal tonsils have a rich vascular network, after tonsillectomy there remains a risk of bleeding. Therefore, if the doctor discovers prerequisites for blood loss, the operation is postponed or additional medications are prescribed to prevent bleeding during surgery or in the first days after it.
The first week after surgery is considered the most dangerous. During this period, tissue healing and rejection of fibrin formed at the site of the removed tonsil occurs. Do not take any action on your own. Contact qualified specialists of the Clinic who will provide the necessary amount of medical care and prevent the development of serious complications.
After tonsillectomy, cases of relapse of the disease cannot be excluded. But the high professionalism of our Clinic’s surgeons and the use of innovative technology make it possible to minimize any risks and ensure maximum infectious safety for our patients.
The difference between tonsillotomy and tonsillectomy
Tonsillotomy is an operation in which enlarged tonsils are removed not entirely, but partially. This type of surgical intervention is indicated for patients with grade III hypertrophy of the palatine tonsils, when they occupy the entire space from the anterior palatine arch to the uvula. During a tonsillotomy, part of the enlarged tonsils is removed. Tonsillotomy, in contrast to the more radical method of complete removal of the tonsils, allows them to preserve their protective functions. This method is also recommended for treating children.
Complications of tonsil cysts
A cyst on the tonsil is a chronic source of infection that can behave in an unknown way, causing various complications. The neoplasm in the pharynx is constantly rubbed with food, which leads to the formation of a chronic inflammatory process. The longer the patient does not seek medical help, the longer the infection progresses; along with the bloodstream, infectious pathogens are carried to all cells and organs, disrupting their normal functioning.
A long-term infectious process is accompanied by general intoxication of the body. Toxins produced during the activity of pathogenic microorganisms disrupt the functioning of the liver and kidneys, provoke the development of chronic fatigue syndrome, reduce immunity and make a person vulnerable to even the most harmless infections.
Only an otolaryngologist can choose the treatment for a cyst on the tonsils, based on the results of pharyngoscopy. If the doctor suspects the development of a malignant process, a consultation with an oncologist will be required. Other studies may also be prescribed: rhinoscopy, audiometry, computed tomography and magnetic resonance imaging of the brain, otoscopy. In advanced cases, the tumor can grow into nearby tissues, including brain structures.
What to do if your child is sick
If a child is diagnosed with inflamed tonsils, the doctor will recommend what to take in this case. It is important to control the process and prevent it from becoming chronic. Separately, the doctor will dwell on recommendations for prevention. If you follow all the advice, inflamed tonsils in a child can be cured quickly and without relapse.
What to take
Drug treatment for children is most preferable to surgical removal of tonsils. Inflamed tonsils in a child are treated with antibacterial drugs, but if they do not bring results, the doctor changes them to antifungal drugs.
When you call a doctor, he will advise you on what to take if your child has inflammation of the tonsils and will prescribe a list of medications and safe antibacterial agents. Strepsils or Faringosept lozenges will help relieve sore throat. In children from the age of three, sprays can be used to irrigate the throat.
Are antibiotics needed?
Treatment with antibiotics is necessary for purulent inflammation of the tonsils. The doctor will prescribe the patient a course of broad-spectrum medications. The following groups are generally recommended:
- penicillins – Amoxicillin, Flemoxin solutab, Amoxiclav;
- macrolides – Azithromycin, Vilprafen;
- cephalosporins – Ceftriaxone, Cephalothin.
Prescriptions can be adjusted, but usually the course is at least ten days. If therapy is ineffective, the treatment regimen is changed.
Recovery in the postoperative period
The operation requires the patient to remain in the hospital for several days. After the operation, the patient is transferred to a ward for further medical supervision.
The first day is the most unpleasant for the patient, since it is not recommended to swallow, eat or drink, and the patient may also experience severe pain. Bed rest is observed for 2-3 days. If the tissues heal well and there are no signs of bleeding, the patient can be discharged for further outpatient observation. On average, a patient is discharged from the hospital within a week. The tissues finally heal within three weeks. All this time, the patient may experience pain and discomfort in the throat, as well as periodic fever.
For 10-20 days after the operation, that is, throughout the recovery period, the patient is recommended to follow a diet: hot, cold, sour, spicy foods should be excluded, as well as the consumption of rough food in the form of cookies, gingerbread, crackers, since such food can irritate the injured area. It is recommended that the food be soft: in the form of baby food, cereals, and various soufflés.
In the postoperative period it is prohibited:
- play sports, lift weights, as exercise can lead to bleeding
- visit baths, saunas, take a hot bath
- consume hot foods and drinks
As noted above, pain is the most unpleasant ailment that accompanies the patient throughout the recovery period from the first day after surgery. The pain may bother the patient at rest, or may intensify when swallowing and talking. To improve the patient's well-being and reduce pain in the postoperative period after tonsillectomy, drugs for general and local anesthesia are used. The local drugs used must also have an anti-inflammatory effect.
The degree of enlargement of the tonsils.
There are four stages of enlargement of the tonsils. At the first stage, the tonsils occupy a third of the space between the pharynx and the palate. In this case they are said to be slightly enlarged. Symptoms of the disease do not manifest themselves in any way.
At the second stage, the tonsils already occupy half of the free space. There is discomfort when swallowing liquids, food and breathing. Tissue hypertrophy is average.
In the third stage, swallowing becomes very difficult as the lymphoid tissue increases to an impressive size.
The fourth stage is characterized by severe hypertrophy, when the tonsils completely block the pharynx. This condition interferes with proper breathing and nutrition.
If inflammation of the tonsils begins, without timely treatment, the stages quickly replace each other.
Laser tonsil removal
In medicine, carbon dioxide or diode lasers are used. The cells of the body contain from 60 to 90% fluid. When a laser is applied to an area of tissue, its temperature rises and the liquid begins to evaporate and the protein molecules dry out.
Since the laser energy is mainly distributed at a depth of 2-3 mm, the result is a sequential stratification effect with simultaneous cauterization (coagulation) of small blood vessels. Therefore, the laser cut is almost bloodless. This effect is important - blood loss during surgery is significantly reduced, and the surgeon, working on a dry surface, has a larger field of view.
Advantages of the laser tonsil removal method
When removing tonsils, the destructive and coagulating effects of a laser beam are involved. The first allows the tissue to be removed, the second clots the blood at the incision site and seals the vessels, which prevents bleeding and infection of the wound.
Contraindications to tonsillectomy
Contraindications can be absolute, when surgery is completely excluded for the patient, and relative, when there are reasons that postpone surgery until these reasons are completely eliminated.
Absolute contraindications to tonsillectomy:
- blood diseases
- some heart diseases
- tuberculosis
- cirrhosis of the liver
Relative contraindications to tonsillectomy:
- ARVI and influenza
- exacerbation of chronic diseases
- menstruation
- pregnancy
Testing to confirm the need for tonsillectomy
This diagnosis of “decompensated form of chronic tonsillitis” is established on the basis of a set of data, including the history of the disease, clinical picture, laboratory data (biochemical blood test with determination of antistreptolysin-O, rheumatoid factor, C-reactive protein, study of the immunological function of the palatine tonsils), and also the presence of complications: rheumatism, infectious nonspecific polyarthritis, diseases of the heart, kidneys, thyroid gland, purulent complications (peritonsillar abscess), information about the ineffectiveness of previous conservative treatment.
Study of the functional state of the palatine tonsils
Surgical removal of tonsils
If we talk about the removal of the tonsils, then the operation to completely remove the tonsil tissue is called a bilateral tonsillectomy.
Partial removal of the tonsils is called a bilateral tonsillotomy.
It is extremely rare that the palatine tonsil is removed routinely on one side. There is also a practice of a number of hospitals (they like to do this in the Pirogov City Clinical Hospital No. 1) of removing the palatine tonsil or tonsils in case of a paratosillar abscess. This operation is called abscessonsillectomy. But it must be remembered that against the background of severe pain caused by an abscess, removal of the tonsil is extremely painful. Due to the purulent process, it is impossible to provide adequate anesthesia. Therefore, it is necessary to anesthetize the peri-almond tissue only with strong anesthetics: Ultracaine and Ultracaine DS-forte.
Routinely, palatine tonsils can be removed under local anesthesia or general anesthesia. Previously, this operation was performed only under local anesthesia.
Fortunately, there is now modern equipment that allows removal of palatine tonsils under general anesthesia or under anesthesia using cold plasma coagulation - Coblator.
Preoperative preparation
Directly for the operation, it is necessary to undergo a preoperative examination, the scope of which is determined by the doctor after the examination.
Preoperative preparation is standard:
- Laboratory tests - general blood test, blood biochemistry, blood for RW, HIV, hepatitis B and C, coagulogram, Rh factor, blood group.
- Instrumental data - ECG, fluorography or chest x-ray.
- Conclusion of specialists - therapist (pediatrician) and dentist about the absence of contraindications to surgical intervention.