Herpetic gingivostomatitis
This form of the disease develops due to the herpes virus type I.
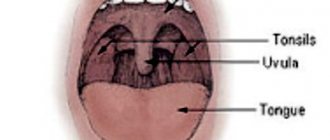
Its symptoms include round ulcers with a white coating, red at the edges, no larger than 0.5 mm in size, covering the mucous membrane of the mouth and gums. Acute gingivostomatitis is characterized by high (up to 38-39 degrees) temperature, bleeding and swollen gums, and inflamed lymph nodes. The number of ulcers sometimes reaches 15-20 pieces. Weakness occurs, problems with eating due to pain, appetite disappears, sleep is disturbed. These symptoms may be accompanied by signs of acute respiratory viral infection or catarrhal tonsillitis.
Other types of gingivostomatitis - allergic, plasmacytic and atypical - are much less common.
Causes of gingivostomatitis
For the development of ulcerative gingivostomatitis, a number of factors are necessary, the main one of which is a decrease in the body’s protective reaction.
The disease usually occurs when one or more of the following factors are present:
— An organism weakened due to illnesses; — Hypothermia, colds: — Chronic infections and diseases; — Inflammatory processes in the mouth, tartar deposits; — Chronic injury to the oral mucosa (for example, due to dentures); — Diseases of the immune system (including HIV); — Lack of vitamins, iron deficiency anemia; — Lack of oral hygiene measures for a long time; - An allergic reaction to toothpaste, medications or any food.
Acute herpetic gingivostomatitis
The incubation period most often lasts from 2 to 6 days, but can last up to 17 days. Acute herpetic gingivostomatitis, as a rule, affects children of toddler and preschool age, most often from 1 year to 3 years. In recent years, cases of illness in children 6–10 months of age, artificially fed from the first months of life, have become more frequent.
A generalized form of herpes is possible in a child born to a mother who does not have antibodies to the herpes simplex virus. Infection of such a child, who has not received passive immunity from the mother, leads to the development of a severe septic disease with damage to the serous membranes of the brain and internal organs. Extensive necrosis occurs in the oral cavity; most children die.
Herpetic gingivostomatitis is contagious. It occurs acutely with a pronounced disturbance of the general condition and local symptoms, depending on which mild, moderate and severe forms of the disease are distinguished.
Mild form of acute herpetic gingivostomatitis in children In mild form of acute herpetic gingivostomatitis, the general condition of the child is slightly disturbed, the body temperature is subfebrile, less often normal, the prodromal period is not always pronounced. The first clinical sign is pain when eating. Upon examination, the doctor detects hyperemia and swelling of the oral mucosa and individual, usually non-confluent, round-shaped erosions with a diameter of 1 - 5 mm, covered with fibrinous plaque. The rash is usually one-time, no new elements appear in the following days, the duration of the disease is 4-5 days.
Moderate and severe forms of acute herpetic gingivostomatitis in children Moderate and even severe forms of acute herpetic gingivostomatitis are more often diagnosed in children. The onset of the disease is acute, as in most other infectious diseases, body temperature is above 38°C, and in severe cases can reach 40°C, intoxication is pronounced: the child is lethargic, capricious, sleeps poorly, complains of a headache, appetite is significantly reduced even before the onset of the disease. erosions in the mouth. Some children experience nausea, vomiting, and stool disorders. Then catarrhal symptoms often appear: runny nose, cough, conjunctivitis. Usually during this period the child is examined by a pediatrician and in most cases diagnosed with an acute respiratory disease. However, with a careful examination of the maxillofacial area, the pediatrician may detect enlarged, painful submandibular, chin, cervical lymph nodes and initial signs of catarrhal gingivitis; the gingival margin is brighter in color than the rest of the oral mucosa, the apices of the interdental gingival papillae are not sharp, as is normal, but rounded.
On the 2nd, 3rd or (less often) 4th day of the disease, rashes of individual and grouped blisters with a diameter of 1 - 3 mm appear on the mucous membrane of the mouth, and often on the red border of the lips and facial skin. On the skin and red border of the lips, the vesicle stage is easily determined; at first the vesicles have transparent contents, after 1–3 days their contents become cloudy, then shrink into a crust. If the lining of the vesicle is damaged, skin erosion occurs. On the oral mucosa, intraepithelial vesicles quickly open and the doctor sees round-shaped erosions - aphthae. Aphthae are sharply painful, they are localized on the tongue, mucous membrane of the lips, cheeks, and less often on the palate, arches, and gums. With a massive rash, aphthae merge with each other and form extensive erosions of various shapes. The oral mucosa, free from erosion, is swollen, hyperemic, and the tongue is coated. The gingival margin is also swollen, hyperemic, and erosions often form along the edges of the gums. Salivation increases, but the saliva is viscous with an unpleasant odor.
The period of rash lasts 2–4 days, the child’s condition remains serious, some children refuse not only food, but also drink, which increases intoxication. Of great importance in the pathogenesis of the disease is secondary infection of erosions with endogenous mixed, primarily coccal, microflora of the oral cavity, which becomes pathogenic in a child weakened by a viral infection. Some children with severe forms of the disease develop deep ulcerative-necrotic lesions of the oral mucosa.
The duration of the disease depends on its severity and the effectiveness of treatment and lasts 7–15 days, aphthae heal without scarring, and the symptoms of gingivitis persist longer. The disease does not recur if stable immunity is developed. In recent years, many children have experienced relapses of the disease.
Acute herpetic gingivostomatitis should be distinguished from drug-induced stomatitis, erythema multiforme and similar syndromes, from diphtheria and other stomatitis in acute infectious diseases.
Severe form of acute herpetic gingivostomatitis in children (Pospischilla aphtoid)
Pospishill described a severe form of strictly herpetic gingostomatitis in children debilitated by infectious diseases. With this form of erosion, erosions occurred not only in the oral cavity and on the skin of the face, but also on the skin of the fingers, including near the nail plates, as well as on the genitals. Abroad, this disease is called Pospischilla aphtoid.
Gingivostomatitis in children
Most often in childhood, gingivostomatitis occurs, caused by the herpes virus.
The disease occurs in an acute form, usually of moderate or severe severity. Gingivostomatitis in a child begins with a sharp rise in temperature, lethargy, and headache. All these symptoms in children appear even before ulcers appear in the mouth, and they can easily be confused with signs of a cold or flu: there is a cough, runny nose, and sometimes diarrhea.
Upon examination, enlarged lymph nodes under the jaw and on the neck and reddened gums are detected. For 2-3 days, the oral mucosa becomes covered with ulcers, which are very painful. The illness lasts one to two weeks.
Treatment of gingivostomatitis consists of aseptic treatment and anesthesia of the oral cavity, as well as antiviral therapy and strengthening the immune system.
Primary infection
Most cases of primary infection are asymptomatic, and clinical lesions are observed in a minority of infected individuals. After an incubation period (2–14 days), the disease manifests itself in the form of herpetic gingivostomatitis or dermatitis.
Herpetic gingivostomatitis
The most common clinical manifestation of primary HSV-1 infection is gingivostomatitis in children and young adults. Fever for 2 to 7 days, malaise, myalgia, inability to eat, irritability, and cervical adenopathy are also typical. Exudative or ulcerative pharyngitis may be present. Multiple ulcerations appear in the back of the mouth; lesions on the oral mucosa may persist for 2-3 weeks. The most common complication of infection is dehydration in children due to refusal to take fluids by mouth, which may require hospitalization. In sexually active individuals, HSV-2 can cause a primary infection in the form of oral lesions and pharyngitis, which are associated with moderate to severe pain and systemic symptoms simulating bacterial tonsillitis.
Herpetic dermatitis
The usual localization of rashes is the circumference of the mouth, especially the red border of the lips, nose. In more rare cases, the rash is located in the area of the cheeks, temples, eyelids, ears - this localization is called simple gladiator herpes (Gladiatorum Herpes Simplex Virus), as it is often found in wrestlers. The rashes are grouped hemispherical blisters against a background of erythema and edema. 1–2 days before the rash appears, patients feel a burning sensation, tingling, itching in the places where the rash will appear in the future. The contents of the vesicles are transparent, then become cloudy. Closely located bubbles can merge into a multi-chambered continuous bubble. After the bubbles open, erosions and crusts form.
The process on the skin resolves within 10–14 days. In the case of a secondary infection, relapse continues for up to 3–4 weeks.
Atypical forms of herpetic dermatitis
- Zosteriform herpes simplex is characterized by the appearance of vesicles along one or another nerve of the face, limb, or buttocks. This form differs from herpes zoster in the absence of pain radiating along the nerve.
- The abortive form occurs in areas of skin with a thickened stratum corneum on the skin of the palms and fingers. It manifests itself as barely noticeable vesiculopapular elements, accompanied by itching, burning, and pain along the nerves.
- The edematous form occurs on skin with loose subcutaneous tissue - eyelids, lips. Due to severe swelling, the primary elements are not visible.
- The elephantiasis-like form is an edematous form with the development of persistent lymphostasis in the lesion.
- The ulcerative form is characterized by the formation of small ulcers at the site of ordinary herpetic eruptions. The ulcers slowly increase in size and do not epithelialize for a long time. If they persist for more than 3 months, then they are classified as AIDS-marker diseases.
- The hemorrhagic form is characterized by the appearance of blisters with bloody contents; the rash can be located on any part of the skin.
- The hemorrhagic-necrotic form occurs with necrosis at the site of the rash and the formation of scars.
Complications of primary infection
Common complications of a primary infection are:
- eczema herpetiformis in atopics;
- keratoconjunctivitis;
- autoinoculation;
- dissemination of HSV infection in other skin conditions such as Darier's disease, mycosis fungoides, ichthyosis vulgaris and congenital ichthyosiform erythroderma.
Recurrent infection
Based on the natural history of HSV-1, infection is now defined as a persistent chronic infection of sensory ganglia with varying degrees of epithelial expression. Up to 40% of people infected with HSV-1 have a clinical relapse at some stage. Asymptomatic spread of HSV-1 in saliva has been reported in 1-10% of adult cases.
Factors that provoke reactivation of the virus include:
- exposure to ultraviolet radiation;
- illness with fever;
- stress;
- premenstrual tension;
- surgical procedures;
- dental surgical procedures;
- dermabrasion, including laser therapy;
- neurosurgical interventions.
Most individuals who develop a recurrent infection have a prodromal phase with sensations of burning, itching, numbness and/or pain. This phase occurs over 6-12 hours and is followed by clinical symptoms. Groups of vesicles appear on an erythematous or papular base at the junction of the skin and mucous membranes on the lips and on the internal keratinized areas of the oral cavity, such as the gums and hard palate. The ulceration phase is very short, followed by a long crusting phase with an average duration of 133 hours. The total healing time is 7-10 days.
Atypical forms of recurrent herpes infection
Patients with immunodeficiency and HSV-1 infection have an increased level of viral activation - 70-80%. In such patients, ulcerations develop primarily around the mouth and within the oral cavity, both in keratinized areas and in areas where keratinization is absent.
- Herpetic geometric glossitis
was first described in 1993 as a characteristic pattern of HSV infection of the tongue in organ transplant patients and in HIV-infected patients. - A migratory form in which during each relapse the rash is located in new areas.
Complications of orofacial recurrent HSV infection
- eczema herpetiformis;
- recurrent eczema multiforme;
- nosocomial spread of infection, including neonatal herpes;
- herpetic whitlow in dentists and other health care workers.
Feline gingivostomatitis. New in treatment
Feline gingivostomatitis is an inflammation of the oral cavity (gums, corners of the mouth) with the formation of wounds or ulcers around the teeth and on the mucous membrane. Also, the process of inflammation can spread to the tongue, hard and soft palate, the mucous membrane of the inner surface of the lips and cheeks, to the parotid and submandibular lymph nodes.
The presence of dental calculus leads to the development of gingivostomatitis. They consist of deposits of microbes and organic substances held together by an inorganic matrix of hydroxyapatite, calcium and phosphorus (from saliva). Certain bacteria found in the folds of the gums produce toxins (hyaluronidase and lysosomal enzymes) which, when combined with a large influx of inflammatory cells, irritate the gums and release inflammatory cellular elements that lead to swelling, redness and loosening of the gums. Common bacteria that cause oral lesions in cats: Pasteurella spp., Fusobasterium nucleatum, Actinobacillus spp., Staphylococcus spp., Streptococcus spp., Pseudomonas spp.
Other causes of gingivostomatitis include:
- a diet containing a high percentage of starch and vitamin D;
- viruses (of all infectious factors, Feline calicivirus (FCV) is most often associated with gingivitis and lymphocytic stomatitis; FHV, FIV and FeLV are less common);
- anodontia/oligodontia - reduced number or complete absence of teeth;
- eosophilic granuloma complex (usually perioral lesions (eg, basal cell carcinoma)) and other skin lesions;
- oncological formations in the oral cavity.
Genetics also have an influence (juvenile gingivitis in cats of Abyssinian, Persian and Maine Coon breeds) and the structure of the oral cavity (in Persian breeds, other breeds with brachycephalic syndrome).
Clinical signs of gingivostomatitis. Diagnostics
An attentive owner can easily identify the signs of gingivostomatitis in a pet. The animal becomes lethargic and apathetic, sometimes showing aggression and irritability. A visual examination of the oral cavity shows red, swollen gums.
Cats with gingivostomatitis often stop eating. They experience polydipsia (frequent drinking of water) and anorexia. Excessive salivation (hypersalivation), sometimes mixed with blood, is common. If the cat does try to eat, it may become awkward, even causing pieces of food to fall out of its mouth. Sometimes a hungry animal swallows large pieces of food without chewing, which can lead to stomach upsets. The cat washes itself more often, carefully rubbing the area of its mouth, as if something is bothering it there.
Gingivostomatitis is easily diagnosed visually - the veterinarian will see red, inflamed gums and oral mucosa. Next, you need to determine the type of disease to determine the causes of inflammation and prescribe the optimal course of treatment. Therefore, diagnostics may include additional procedures:
- mucosal inoculation for various types of pathogenic microflora;
- blood and urine tests;
- virological tests.
The most common catarrhal stomatitis is the beginning of all complicated stomatitis and the development of gingivostomatitis. Classic signs are intense redness, swelling, sore gums, increased salivation, and unpleasant odor. The saliva is viscous and smells unpleasant.
In addition to catarrhal, stomatitis is classified as follows:
- fibrinous (white discharge);
- ulcerative (weeping ulcers on the mucous membrane);
- gangrenous (a complication of ulcerative disease, a strong foul odor is added to the symptoms);
- hemorrhagic (pink discharge mixed with blood);
- papillomatous;
- uremic syndrome;
- autoimmune stomatitis and others.
Gingivostomatitis can develop into a chronic form that is extremely difficult to treat.
Gingivostomatitis can develop into a chronic form that is extremely difficult to treat
Treatment
Depending on the type of infection detected, the doctor prescribes a course of treatment, which may include:
Antiseptics:
- Lugol's solution - shows excellent disinfecting properties: to treat ulcers directly - smear or spray (important: long-term use is avoided, as it can provoke the proliferation of Pseudomonas aeruginosa, which is not affected by iodine);
- Chlorhexidine 0.05% - for washing the mouth or treating wounds and ulcers directly;
- Dentavedin/Metrogil Denta - used up to 3 times a day, applied in a thin layer to sore gums or placed directly into the sockets in case of tooth extraction;
- Stomatidin - irrigate the mouth during inflammation or cauterize ulcers, wounds or sites where papillomas are removed.
Anti-inflammatory medications - to reduce redness and/or soreness. There are two main types used:
- corticosteroids - can be given as tablets or injections (These drugs are good for reducing inflammation; they also have the positive side effect of stimulating appetite, which is very important for this problem. However, long-term use of steroids can cause unwanted side effects in the body);
- non-steroidal anti-inflammatory drugs (NSAIDs) - are considered safe and are widely used in these cases (Usually in the form of injections or drops that are administered into food or directly into the mouth. NSAIDs are recommended for use in combination with gastroprotectors (due to the negative effect on the gastrointestinal tract), the course should last no more than 5 days (exception: the drug Metacam, a course of up to 14 days is possible)).
Antibiotic therapy:
- Lincomycin 10% - a course of 3 to 7 days at a dose of 2 ml/10 kg for intramuscular administration and 1 ml/10 kg for intravenous administration;
- Amoxicillin 15% - single injection in a dose of 1 ml/10 kg under the skin or into the muscle; If necessary, you can re-inject after 48 hours.
Immunostimulants - to stimulate the immune system and enhance the body's response to the inflammatory process. Apply:
- Stimulus - 0.5 ml/kg once a day, up to 10 days;
- L-cin - 0.5-1.0 ml/animal, depending on weight, once a day, course - 5 days.
Dental care . Any tartar will aggravate the inflammation, even if it is not the main cause. In more severe cases, it is possible to remove all molar teeth. If conservative treatment is not possible, surgical removal of the affected mucosal tissue that has undergone changes is performed.
Diet - complete refusal of milk (the milk environment is beneficial for the development of bacteria), transferring the cat to food that is easier to accept (usually canned soft food). Food should be at room temperature.
In some cats, stress also plays a role in initiating outbreaks of gingivostomatitis. Removing stressors or giving the cat a "safe" place can help in these cases.
Treatment of gingivostomatitis most often takes place at home with a visit to the veterinarian on a set schedule. In this case, the owner’s main task is to strictly follow the recommendations.
In complex advanced forms, the veterinarian may recommend inpatient treatment with round-the-clock monitoring, administration of medications and supportive drugs through a drip. In some cases, the animal may require surgical intervention (removal of teeth or parts of the mucous membrane).
You should also keep in mind that not all treatments are suitable for cats. There are cases when an animal does not respond completely to treatment, regardless of the procedures performed. Therefore, some animals require repeated treatment or constant monitoring and therapy throughout their lives.
Experience with the use of the drug Ciprocoline
Based on market needs, the Ukrainian created a combination drug Ciprocolin containing two antibiotics: ciprofloxacin and colistin sulfate. As a result of the synergy of these active ingredients, it was possible to create a formula whose activity is higher than that of its individual components.
When administered orally, ciprofloxacin irrigates the inflamed areas in the oral cavity and begins to be absorbed directly into the oral cavity. Entering the blood, it penetrates all organs and tissues of the body, reaching maximum concentration after 1-2 hours. Therapeutic concentration lasts up to 24 hours. The mechanism of action of ciprofloxacin lies in the inhibition of bacterial DNA gyrase, which prevents the process of DNA replication, thereby disrupting the integrity of the bacterial cell membrane and its death. Ciprofloxacin hydrochloride quickly eliminates R-plasmids, which prevents the development of resistance of microorganisms to the drug.
Ciprofloxacin is effective against gram-positive and gram-negative microorganisms, namely: against E.coli, Staphylococcus spp., Streptococcus spp., Pseudomonas spp., Salmonella spp., Shigella spp., Enterobacter spp., Klebsiella spp., Proteus spp., Campylobacter spp. ., Brucella spp., as well as Mycoplasma spp. and Chlamydia spp.
Colistin sulfate is an antibiotic that is synthesized by the aerobic spore-forming bacillus Bacillus polymyxa. Colistin sulfate has a bactericidal effect on gram-negative bacteria (E. Coli, Salmonella spp., Pasteurella spp., etc.). Colistin sulfate binds to phospholipids of the cytoplasmic membrane, increasing its permeability to components, which leads to destruction of the bacterial cell.
Cyprocoline is a powder that, after dissolving in plain water, turns into a white suspension. It has a sweetish taste and smell of bacon, which is attractive to animals. Used to treat dogs, cats and poultry for all types of stomatitis and gingivitis; mixed and secondary infections in diseases caused by microorganisms sensitive to ciprofloxacin and colistin.
Cyprocoline is administered orally. It is set with a dosing syringe at the rate of 1 ml of the finished suspension per 1 kg of animal weight.
Watering is carried out once a day. The course of treatment is 7-10 days, depending on the clinical signs and severity of the disease. After drinking the drug for use in dentistry, it is advisable not to feed or water the animal for 2 hours to ensure longer contact of the drug with inflammation in the oral cavity.
Clinical case
The owners of a Thai breed cat named Solomon contacted the WSW CLINIC of Dr. Velichko (Kyiv). Age 8 years. Weight 5 kg. Lives in an apartment. Vaccinated. Oral hygiene is carried out periodically, removing plaque from teeth using cotton pads with chlorhexidine. Recently, the owners have noticed that the cat has become slower and more careful in eating and, while washing its face with its paw, rubs its mouth area more often.
Upon careful examination, the veterinarian discovered intense redness, swelling, soreness of the gums, and deposits of tartar on the molars and premolars of the upper and lower jaws.
A diagnosis was made of gingivostomatitis in the initial stage. It is proposed to remove supragingival tartar and plaque using ultrasound. The manipulation was carried out under sedation with the drug Relax.
View of the animal's teeth during the initial examination at the clinic
Home treatment prescribed:
- Chlorhexidine 0.05% - for sanitation of the mouth after each meal, 30 days:
- Cyprocoline - drinking 5.0 ml of the prepared suspension once a day, course 10 days;
- Metrogyl Denta - treat inflamed areas of the gums with a thin layer once a day at night, 30 days;
Visit the doctor again after 60 days.
According to the owners, after 3 days from the start of treatment, the cat showed positive dynamics. The animal's condition has improved, it actively consumes food while eating, and there is no pain syndrome.
There is also a significant improvement in gum health in the mouth. The redness and inflammation that was caused by the presence of tartar has disappeared.
The course of treatment was continued according to the doctor’s recommendations.
Thus, the drug Ciprocoline in the complex treatment of gingivostomatitis showed positive dynamics.
Recommended by veterinarians in practice for the treatment of dental problems.
Drinking the drug Ciprocoline at home
The full text of the article was published in the journal VET TOPic (Veterinary Topic), No. 4/2021.
Gingivostomatitis causes and symptoms
Gingivostomatitis is an infectious disease that occurs when the gums and other parts of the oral mucosa are damaged by bacteria or viruses. Occurs in children and adults. The pathology is accompanied by symptoms of inflammation and the formation of painful ulcers. It often develops in very young children when infected with the herpes virus. There may be other reasons, for example, past infectious diseases, poor hygiene.
Features of gingivostomatitis
The infection can occur in mild and severe forms. In the second case, general symptoms of intoxication appear, the patient’s temperature rises, and appetite disappears.
The dentist sees the disease during an external examination. Additionally, a biopsy may be prescribed for differential diagnosis. Therapy comes down to ridding a person of unpleasant symptoms and eliminating the source of infection. Often antibiotics are required, but only a doctor can prescribe them, since, for example, with a viral form without the risk of complications, they are not needed.
The doctor must carry out professional teeth cleaning, remove dental plaque, carry out antiseptic treatment, and prescribe frequent mouth rinses. All this is necessary to prevent the spread of infection.
Symptoms
The manifestations of the disease differ from person to person, depending on its severity, type, and general health. Gingivostomatitis can be acute or chronic.
The following symptoms are characteristic of this disease:
- Single or multiple ulcers on the oral mucosa and gums.
- Pain while eating, talking, brushing teeth.
- Swelling of the gums, their hypertrophy.
- Unpleasant smell.
- Fever, weakness.
- Inflammation of the lymph nodes.
Types of disease
Vincent's gingivostomatitis is an ulcerative-necrotic type of pathology. The mucous membrane becomes covered with a gray coating and ulcers. There is a putrid smell.
The herpetic form, which is provoked by the herpes virus, is accompanied by the appearance of gray ulcers with red rims. In acute cases, the general condition suffers, the temperature rises to 39. The gums bleed and swell. The number of ulcers can reach more than 20 pieces. Additionally, symptoms of sore throat may appear.
Allergic and atypical forms of the disease also occur, but they are diagnosed very rarely.
Causes of the disease
For the development of gingivostomatitis, certain conditions are required so that pathogenic microorganisms can penetrate the tissue and cause a pathological process. The main one is weakened immunity.
Other risk factors include:
- Past infectious diseases.
- Chronic infections.
- Hypothermia.
- Stress.
- Chronic damage to the mucosa.
- Immunodeficiency, HIV.
- Vitamin deficiency.
- Allergy.
- Poor oral care.
- Iron-deficiency anemia.
Publications in the media
Acute herpetic stomatitis is a viral infection of the oral mucosa.
Etiology and pathogenesis. The disease is caused by HSV and is one of the clinical forms of manifestation of primary herpetic infection. Transmission of infection occurs by contact and airborne droplets. The incidence of children from 6 months to 3 years is explained by the disappearance of AT received from the mother.
Clinical manifestations. A viral disease has five periods of development: incubation, prodromal, period of disease development, extinction and clinical recovery. Depending on the severity of general intoxication and local manifestations in the oral cavity (area of damage), the disease can occur in mild, moderate and severe form.
• The disease begins acutely with general malaise, weakness, headaches, nausea, lack of appetite; is accompanied by a rise in body temperature, reaching 41 °C or more in severe forms. Enlargement and tenderness of the submandibular and, in severe cases, cervical lymph nodes are determined.
• When the body temperature rises, against the background of hyperemia and swelling of the oral mucosa, lesions appear on the lips, cheeks and tongue (from 2–3 to several dozen, depending on the severity of the disease).
• In severe forms of the disease, the lesions are localized not only in the oral cavity, but also on the skin of the face, earlobes and eyelids.
• At the initial stage, gingivitis is detected, accompanied by severe bleeding of the gums.
• With the addition of fusospirillary microflora, gingivitis becomes ulcerative-necrotic in nature.
• Hypersalivation is noted, although the saliva becomes viscous and viscous. Bad breath develops. Lips are dry, cracked, covered with crusts, there is maceration in the corners of the mouth.
• The severe form is accompanied by profuse salivation and damage to the skin with the appearance of aphthae-like elements. Young children may develop delusional states.
• Violation of the general condition is confirmed by laboratory data.
• Depending on the severity and intensity of treatment, recovery occurs within 1–3 weeks. Aphthae heal without scarring.
Diagnostics. Changes characteristic of an acute inflammatory process are detected in the blood. The content of lysozyme in saliva decreases, IFN is absent. The pH of saliva changes: first to the acidic side, then to the alkaline side. The cytological picture is nonspecific. In the first days, the virus is detected in the contents of the vesicles. Subsequently, the FN titer is determined.
Differential diagnosis. With other viral diseases (foot and mouth disease, etc.) and allergic lesions.
TREATMENT
Regime and diet. It is necessary to follow a diet: predominantly liquid or semi-liquid food and plenty of liquid (tea, fruit juices, fruit infusions). Before feeding, the oral mucosa is anesthetized with a 5% anesthetic emulsion. After eating, be sure to wash or rinse your mouth.
Drug treatment. Determined by the stage and severity of the process. It is recommended to treat the child’s oral cavity with a solution of proteolytic enzymes (trypsin, chymopsin, pancreatin, etc.), which help dissolve plaque, and IFN. Applications are made with antiviral ointments (oxalic, bonaftone, etc.). Later keratoplasty is used. General treatment is required, including antiviral drugs and vitamins.
Forecast. Usually favorable. An unstable, non-sterile immunity occurs. The herpes virus usually remains in the body for life. Transition to a chronic form is possible.
Prevention. It is necessary to take precautions due to the highly contagious nature of the disease.
ICD-10 • B00.2 Herpetic gingivostomatitis and pharyngotonsillitis
Current issues of severe herpetic infection in adults
Currently, the number of patients with recurrent herpes infection caused by herpes simplex viruses (HSV) types 1 and 2 of various localizations is steadily increasing. The most common localization in adults is anogenital and labial. Many issues of the pathogenesis and treatment of severe and extremely severe herpesvirus infection are still not resolved.
The HSV species belongs to the family Herpesviridae, subfamily L-Herpesviridae, a species of HSV. There are two main types of virus - HSV 1 and HSV 2. Infection is possible with either one or two types of pathogen. HSV is capable of invading various cells of the human body: skin cells, mucous membranes of the urogenital and gastrointestinal tracts (GIT), respiratory tract, central and peripheral nervous system, liver, vascular endothelium, as well as blood cells - lymphocytes, etc. [ 1]. The place of permanent residence (lifelong persistence) of HSV is the paravertebral sensory ganglia. HSV is transmitted by direct contact; the pathogen can be transmitted through household contact and vertical routes (from mother to fetus), as well as through transfusion and parenteral routes through instruments during surgical interventions, dental procedures, etc.
As you know, most people are infected with HSV. The primary immune response to infection occurs latently or with herpetic eruptions with a local and general inflammatory reaction. In individuals with a normal immune response, HSV multiplication (replication) is under immunological control, and relapses are extremely rare or do not occur throughout life. The antiviral defense of the body involves nonspecific defense factors that destroy or block viruses: macrophages and other cells producing interferons (IFN) α, β and γ, a number of interleukins (IL) (tumor necrosis factor (TNF), IL-6, etc.) , natural killer cells and factors that form a specific immune response against a particular virus: cytotoxic T lymphocytes (CTL) (CD8+ T lymphocytes) and B lymphocytes, responsible for the production of specific antibodies that block the replication of the virus and viruses located outside the cell. For adequate functioning of these cells and maintaining the immune response, appropriate production of IFN and IL is necessary.
Under the influence of various exogenous and endogenous factors that damage the immune system, control over viral replication may weaken and, accordingly, the development of relapse. Recurrence of HSV infection can be triggered by other infectious diseases, hypothermia, excessive insolation, mental or physical stress, intoxication of various origins, including alcohol consumption, cyclical changes in hormonal status (menstruation), especially with an imbalance of hormone levels in women, sudden changes in climatic zones and etc.
With long-term chronic infection, viruses have a multifaceted adverse effect on the human immune system. HSV directly damages cells of the immune system (lymphocytes, macrophages and natural killer cells). By synthesizing suppressor proteins and chimeric proteins, viruses inhibit many immune reactions: HSV can block the action of IFN, disrupt the recognition of infected cells and other protective reactions. In addition, the high mutational activity of the viral genome also contributes to the escape of the virus from immunological control.
Chronic, often recurrent HSV infection can provoke the development of autoimmune conditions (antiphospholipid syndrome, autoimmune thyroiditis, autoimmune vasculitis, etc.). In addition, when HSV is integrated into the genetic apparatus of cells, neoplastic transformation of cells is possible. Thus, HSV is one of the increased risk factors for developing body and cervical cancer and other cancers. Also, HSV infection is one of the leading causes of spontaneous abortions, premature births, and the birth of children with pathologies of the central nervous system and internal organs. HPHI is associated with many “diseases of civilization” - atherosclerosis, coronary heart disease in people under 50 years of age, etc. Severe HPHI can be a marker of cancer and AIDS [7].
Depending on the number and severity of relapses, mild, moderate and severe courses of the disease are distinguished (Table 1).
In severe cases of HSV infection, the simultaneous appearance of several lesions (for example, in the genital area, lips, wings of the nose), as well as the sequential occurrence of rashes of different localization (one relapse against the background of another), the duration of the exacerbation can reach 16–20 days. At the site of the rash, patients feel heat, burning, pain, tension and/or itching of the skin. A group of bubbles filled with transparent content appears on the infiltrated skin. Bubbles can merge into a continuous multi-chamber element. Their transparent contents then become cloudy. The bubbles subsequently open, forming small erosions, or dry out and turn into crusts. A secondary bacterial infection may develop. With relapses, HSV often affects the same areas of the skin. As a rule, with severe infection, the physical and mental condition of patients worsens significantly. In some patients, during the period of relapse, weakness, fever, chills, myalgia, cephalalgia, arthralgia, irritability, sleep disturbance, emotional lability increase or appear; severe depressive states requiring drug correction may also develop. According to US health authorities, HSV infection of anogenital localization is the cause of depression and suicide in approximately 10% of cases. The severe course of the genital form of HSV infection with frequent relapses leads to disruption of the patient’s normal sexual function; the disease often creates conflict situations in the family and at work. Treatment of patients with severe HSV infection is a complex task and should include both drug therapy and psychological adaptation of the patient.
In patients with severe HSV infection, in most cases there is no persistent and significant clinical effect in response to episodic courses of combination therapy (antiviral and immunotropic drugs, restorative drugs). As a rule, such patients change many medical institutions in search of adequate help.
As the disease progresses, many adverse reactions to medications or intolerance to them appear; in some cases, HSV resistance to acyclovir, IFN-a, and other drugs develops. Immunostimulants used empirically may provide relief when taken, but in many cases they are ineffective and even worsen the clinical course of the disease. Manifestations of secondary immunodeficiency worsen, other infections occur, subdepressive states turn into persistent mental disorders, patients lose faith in recovery and in the ability of modern medicine to help them.
To develop modern approaches to the treatment and control of HSV infection and a more in-depth understanding of the pathogenesis of the disease, we studied the state of various parts of the antiviral defense and the cytokine system in patients with severe and extremely severe HSV infection of anogenital and labial localization, as well as the degree of infection ( systemicity of the disease) and the frequency of combination with other herpesvirus infections.
We examined 102 patients suffering from severe HSV infection for more than 2 years (28 men and 74 women, average age 34 ± 1.5 years) and having a relapse rate of more than six per year.
Moreover, 60 patients had from 6 to 11 relapses of HSV infection per year, and 42 patients had from 12 to 20 relapses. In most patients, anogenic or mixed localization of herpes predominated. The average duration of severe disease was 9.3 ± 1.2 years. The control group consisted of 32 practically healthy volunteers (14 men and 18 women, average age - 32 ± 1.6 years). The analysis of a number of parameters studied included the results of an examination of patients with a mild course of the disease (36 people - 10 men, 26 women, average age - 33.4 ± 2.1 years, with a relapse rate of 2.9 ± 0.8 per year). During relapses, the patients' complaints were characteristic. Depression, irritability, memory loss and other disorders of the physical and mental state and cognitive functions were common.
Many patients had a history of repeated courses of antiviral and/or immunotropic therapy, which had an ambiguous effect: either a short-term positive effect on the course of HSV infection, or worsening and development of relapse during or after the cessation of immunocorrection. Such anamnestic data reflect the severity of immune deficiency and the inadequacy of empirical therapy without assessing the immune status and individual selection of immunocorrectors, as well as restorative therapy - immunorehabilitation [5].
When examining patients with severe HSV infection, many markers of secondary immunodeficiency were identified in the form of chronic infectious and inflammatory diseases of various localizations, with a mixed nature of the microflora and, in most cases, its resistance to repeated courses of antibiotic therapy. Of 102 patients with chronic severe HSV infection, the following were identified:
- 86.3% had chronic recurrent diseases of the respiratory tract (chronic pharyngitis, chronic tracheitis, chronic laryngitis, chronic bronchitis, chronic sinusitis, repeated otitis);
- 88.2% had chronic recurrent diseases of the urogenital tract of mixed origin (cystitis, urethritis, vulvovaginitis, adnexitis, salpingoophoritis, prostatitis);
- 50–70% have astheno-vegetative and astheno-depressive syndrome, the formation of chronic fatigue syndrome;
- 91.2% had dysbiosis of the intestinal flora, chronic inflammatory diseases of the gastrointestinal tract (chronic enterocolitis, chronic gastroduodenitis);
- 25–30% have pseudo-allergic skin reactions (itching, urticaria, dermatitis).
These data indicate the need for an integrated approach to the treatment of severe HSV infection, taking into account the complications of secondary immunodeficiency.
The presence of HSV infection was confirmed based on medical history, clinical data, and the detection of HSV deoxyribonucleic acid (DNA) by polymerase chain reaction (PCR) in discharge from the rash. The study of immune status included determination of the main subpopulations of lymphocytes CD3+, CD4+, CD8+, CD72+, CD16+, activation markers of lymphocytes of the major histocompatibility complex - HLa-DR+, CD11b in peripheral blood using monoclonal antibodies. The content of immunoglobulins (Ig) a, M, G, and circulating immune complexes (CIC) in blood serum was also determined. The functional activity of neutrophils—the production of reactive oxygen species that provide bactericidal activity—was determined using the nitroblue tetrazolium test (NBT test). The stimulated NBT test was studied by incubation in vitro with a Staphylococcus aureus culture. Interferon status was assessed by the level of serum IFN and production of IFN a by leukocytes upon stimulation with New Castle disease virus and IFN ( upon stimulation with phytohemagglutinin. Quantitative content of cytokines (IFN α, IFN γ, TNF α, IL-1β, IL-2, IL-4 IL-6) in blood plasma/serum was determined by enzyme-linked immunosorbent assay (ELISA) using test systems (ProCon, St. Petersburg, and Vector-Best, Novosibirsk).
In addition, a PCR study of biological materials was carried out for the presence of DNA of HSV types 1 and 2 and other herpes group viruses: cytomegalovirus, human herpes virus (HHV) type 6, Epstein-Barr virus. The amplification programs we used made it possible to detect viral DNA at a level corresponding to their active replication. The presence of active viral replication was confirmed by semi-quantitative PCR studies and serological tests.
As a result of the study, laboratory signs of secondary immunodeficiency were found in patients with severe HSV infection.
| Figure 1. Frequency of detection of different IgG values in patients with severe HSV infection |
Thus, the majority of patients (91%) did not have an adequate increase in IgG production in response to recurrent HSV infection (Fig. 1). With a recurrence rate of HSV infection of 6–11 relapses per year, a low level of IgG was detected in 25% of patients; with a frequency of 12–20 relapses per month, it was detected in 64.3% of patients. More than 70% of patients had an increased level of CEC by 1.5–2.0 times the normal level. It is known that long-term circulation of CEC can lead to their deposition on the vascular endothelium and serve as one of the factors in the formation of autoimmune pathology.
In the majority of patients with severe HSV infection (70%), disturbances were found in the system of natural and/or specific cytotoxicity (Fig. 2) - a decrease in the content of mature activated natural killer cells CD16+ (less than 11%), T-killers and/or CTLs CD8+ (less than 27%). It is important to note that a pronounced decrease in the level of CD8+ (which also includes suppressor cells) in most cases was combined with an increase in the level of CD4+ and the immunoregulatory index, which is a risk factor for the formation of autoimmune processes. As is known, natural and specific cytotoxicity systems play a leading role in antiviral defense.
| Figure 2. Frequency of detection of disturbances in the system of natural and specific cytotoxicity in patients with severe HSV infection (n = 102) |
In patients with severe HSV infection during relapse, the number of natural killer cells was significantly lower than normal and 2 times lower than the average for persons with mild disease. In almost half of the patients with HSV infection, the identified disorders were combined with disimmunoglobulinemia and deficiency of IgG production. The level of HLa-DR+ lymphocytes, which reflect the production of IL-2 and carry the DR+ receptor, necessary for recognizing virus-infected cells and other immune reactions, was reduced in 39% of patients with HSV infection (its increase was noted only in 17.4% of patients).
The detected disturbances in cytotoxicity systems and their activation markers during HSV infection indirectly indicate an insufficient level of production of IL-2 by T-helper type 1 cells, one of the most important links in the cytokine network, necessary for a complete antiviral immune response.
When studying the functional state of neutrophils in patients with severe HSV infection, an increase in the spontaneous NBT test was detected in almost half of the cases. However, the parameters of the stimulated NBT test and the stimulation index, on the contrary, were significantly reduced in the majority of patients, which indicates that their reserve abilities of neutrophils were depleted.
When studying the interferon status of patients during an exacerbation of HSV infection, differences were identified between mild and severe disease. Thus, the level of serum IFN in patients with mild disease was increased by 2 times compared to the control group (p < 0.05). In severe cases of infection, on the contrary, relapse was accompanied by a low level of serum IFN. The stimulated production of IFN a and IFN g was also reduced, and to a significantly greater extent precisely in cases of severe HSV infection.
Thus, the majority of patients with HSV infection showed severe deficiency of the interferonogenesis system, which correlates with data on the depletion of the reserve abilities of neutrophils in these patients.
We also studied the content of the main pro-inflammatory ILs (IL-1β, TNF α, IL-2 and a number of other ILs) in the blood serum during the period of relapse and during the period of illness outside of rashes. It turned out that in patients with severe HSV infection on days 2–3 of relapse there is no adequate response from pro-inflammatory ILs. In the majority of patients (90%), insufficiency of IL production was detected, and in approximately 10% of patients the studied ILs were not detected in the blood. It should be noted that during the non-rash period, a long-term increase in the level of one or two types of cytokines was also detected.
During a PCR examination of patients with severe HSV infection (the main group), the Epstein–Barr virus (in 76.5% of cases) and HHV type 6 (in 63.5% of cases) were most often found in the oropharyngeal area. Cytomegalovirus infection was detected in 11.0% of patients in this group (in the epithelial cells of saliva, urethra, cervical canal, and in urine sediment). In cases of mild HSV infection (comparison group), the DNA of the above viruses was detected significantly less frequently (Table 2). In general, in severe cases of the disease, the proportion of patients with HSV monoinfection was only 5%, and in mild cases it was about 72% (Table 3).
Thus, it was found that in 95.6% of patients with HSV infection with severe disease, other viruses of the herpes group actively replicate, which allows us to consider this form of the disease as a mixed viral severe infection.
Above, we noted the serious problems that arise in the treatment of HSV infection. As our studies have shown, a major role in the pathogenesis of the disease is played by secondary immunodeficiency, often combined with impaired cytokine production, as well as the presence of a mixed viral herpetic infection. In addition, against the background of these powerful interrelated factors, infectious and inflammatory diseases of the mucous membranes are added to the underlying disease. As a rule, these factors are not taken into account when treating patients with HSV infection.
Treatment of HSV infection should include suppression of viral replication during the period of exacerbation, as well as the formation of a complete immune defense in order to prevent relapses. Previously, we outlined in detail the principles of treatment for IPHI [3, 4]. To stop the exacerbation of herpes infection, acyclic nucleotides (acyclovir, valacyclovir, famciclovir) are used, the action of which is associated with the ability to disrupt the process of HSV replication at the stage of viral DNA synthesis and assembly of viral particles. The effectiveness of acyclic nucleotides depends on their bioavailability, the sensitivity of the virus to the drug, the adequacy of the dose, the duration and frequency of treatment, and the timing of the start of treatment. Prescribing these drugs from the first day of relapse (acyclovir - in a daily dose of at least 1000–1600 mg) helps to quickly stop it (Table 4).
For patients with HSV infection with frequent relapses (six or more relapses per year), in order to prevent them, suppressive administration of acyclic nucleotides is recommended for a long time, which can lead to drug remission during the treatment period. At the same time, a decrease in the frequency of relapses after cessation of treatment (compared to the period before therapy) is observed in only 20% of patients [2]. Acyclic nucleotides of the new generation - valacyclovir and famciclovir, compared to acyclovir, have higher bioavailability with the possibility of two- and three-fold administration, but these drugs are very expensive.
After a year of continuous antiviral therapy, treatment is interrupted to assess the number of relapses. For patients whose relapse rate continues to be unacceptably high, it is advisable to restart treatment [2]. With long-term or frequent therapy with acyclic nucleotides, side effects (gastrointestinal pain, dizziness, etc.) may occur; in some cases, virus resistance to this group of drugs develops. Agents that suppress HSV replication also include glycyrrhizic acid (found in licorice), IFN α (reaferon, viferon, realdiron, etc.) and inducers of its synthesis (amixin, cycloferon, ridostin, poludan, etc.). In case of severe and prolonged course of HSV infection, in the case of a course of use of these drugs during monotherapy, an insufficient clinical effect is noted; with long-term use, known side and undesirable effects develop. IFN a represents only part of the antiviral defense of the immune system and cannot replace its other parts if they fail. In addition, as mentioned above, herpes viruses are able to block the action of IFN α. As clinical experience and our data show [5, 6], the use of immunocorrectors without assessing the immune status, individual selection and control of their action is ineffective or can lead to increased immune dysfunction or hyporeactivity of a number of immune components due to inadequate stimulation. It should be emphasized that the prescription of drugs for topical use (ointments containing acyclovir, sodium foscarnet; epigen intim spray (glycyrrhizic acid), bonafton) is only auxiliary in nature, since blistering rashes on the skin are only one of the manifestations of severe HSV infection. The herpes virus, as shown in the literature and our experience, can replicate in other cells and organs (in the oropharyngeal region, lymph nodes, rectal mucosa, etc.). In addition, our research shows that severe HSV infection is, in fact, not a mono- but a mixed viral infection that develops against the background of secondary immunodeficiency, which changes the view on the examination and treatment of these patients.
We will indicate the principles of examination and treatment of patients with severe HSV infection.
Necessary examinations:
- General clinical examination - for the presence of concomitant diseases and infections (respiratory organs, gastrointestinal tract, urogenital tract - ultrasound examination, magnetic resonance therapy, etc.).
- PCR to detect HHV 4 and 6, cytomegalovirus, hepatitis viruses and intracellular infections (chlamydia, etc.).
- Complete immunological examination.
- Study of hormonal status.
- Study of tumor marker levels over time.
- Carrying out rheumatic tests in dynamics.
- If necessary, oncology search.
Treatment of exacerbation:
- Acyclic methods (acyclovir, valacyclovir, famciclovir) orally for 7–14 days.
- Locally: bonafton, acyclovir, Zovirax, Epigen, etc.
- Detoxification - according to the severity of the condition (enterosorption, plasmapheresis, hemosorption).
- Replacement complex immunotherapy (intravenous Ig, thymic peptides, IFN α and γ, IL preparations).
- Antioxidants comprehensively according to survey data.
- Metabolics.
- Vitamin therapy.
- Laser therapy.
- If necessary, treatment in a hospital.
Treatment of concomitant diseases: treatment and correction of identified concomitant disorders, diseases - chronic infections of the respiratory tract, urogenital tract and gastrointestinal tract, dysbacteriosis, hormonal dysfunctions, metabolic syndrome, depression, etc.
Relapse prevention:
- Eliminate provoking factors (occupational hazards, cold, nervous and physical overload, alcohol abuse, etc.).
- Eliminate other factors that suppress the immune system (poor diet, lack of sleep, smoking, physical inactivity, etc.).
- According to the examination, repeated courses of replacement immunotherapy, other types of immunocorrection, immunorehabilitation.
- The use of IFN, IFN inducers, glycyrrhizic acid preparations, isoprenazine (bivalent drugs with antiviral and immunotropic effects) in a course regimen.
- Prolonged courses of abnormal nucleotides.
- Antioxidants.
- Vitamin therapy, metabolism.
- Dynamic observation.
In conclusion, it must be emphasized that the heterogeneity of disturbances in the immune system during HSV infection requires a differentiated approach to their correction. It seems important to further study the cytokine response in dynamics during severe disease. It is advisable to study the effect of cytokines IL-2 (roncoleukin), IFN γ (gammaferon, ingaron) and other drugs, accompanied by individual selection of treatment regimens, on the course of the disease.
Literature
- Khakhalin L.N. Herpes simplex viruses in humans // Consilium Medicum. 1999. T. 1. No. 1. P. 5–18.
- European standards for the diagnosis and treatment of sexually transmitted diseases. M.: Medical literature, 2003. pp. 102–110.
- Malashenkova I.K., Didkovsky N.A. Principles of immunocorrective therapy for secondary immunodeficiencies associated with chronic viral-bacterial infection // Russian Medical Journal. 2002. T. 10. No. 21. P. 973–977.
- Malashenkova I.K., Didkovsky N.A., Tanasova A.N., Shchepetkova I.N., Levko A.A. Principles of therapy for herpesvirus infection // Doctor.Ru. 2004. No. 4. pp. 26–30.
- Malashenkova I.K., Didkovsky N.A., Levko A.A. On the role of individual selection of immunocorrectors // Pharmateka. 2004. pp. 118–122.
- Levko A. A. The importance of individual selection of immunocorrectors in the complex therapy of chronic recurrent prostatitis caused by urogenital infection: abstract. dis. ...cand. honey. Sci. M., 2005.
- Shulzhenko A. E., Vikulov G. Kh., Tutushkina T. V. Herpetic infections - present and future // Difficult patient. 2003. No. 4. T. 1. P. 6–15.
N. A. Didkovsky , Doctor of Medical Sciences, Professor I. K. Malashenkova , Candidate of Medical Sciences Zh. Sh. Sarsaniya , Candidate of Biological Sciences A. N. Tanasova, I. N. Zuikova, I. A. Zuikov, N. M Khitrik Research Institute of Physico-Chemical Medicine, MMA named after. I. M. Sechenova, Moscow