The powerful lymph nodes located around the pharynx cannot cope with the attack of the pathogen, so the body begins to produce antibodies that can find pathogenic bacteria, paralyzing their activity.
As a result, streptococci are defeated, but the child’s body produces so many antibodies that, in addition to foreign cells, the body’s own tissues, primarily the heart and joints, begin to suffer. Therefore, it is always better to entrust the treatment of sore throat in a child to a qualified doctor.
In 10% of cases, sore throat in children can be caused by Staphylococcus aureus, rarely pneumococcus, Haemophilus influenzae, chlamydia and fungal flora. Viral pathogens (adenoviruses, herpes virus) more often attack the body of children under 3 years of age.
How and why does infection occur?
Infection occurs by airborne droplets, from a sick person, by using shared utensils and eating contaminated food, as well as by a number of other factors:
- weakened immunity;
- hypothermia or consumption of cold foods and drinks;
- mouth breathing (for chronic adenoiditis, deviated nasal septum);
- irritation of the nasopharyngeal mucosa with a runny nose;
- recent viral diseases;
- inflammatory diseases of the ENT organs (sinusitis, sinusitis, otitis);
- caries and other oral infections.
Secondary tonsillitis in children can occur against the background of scarlet fever, diphtheria, mononucleosis, as well as blood diseases.
In any case, a sore throat develops rapidly, in a matter of hours, and is especially acute in children, accompanied by the main symptoms—a sore throat when swallowing and an increase in body temperature.
Causes and routes of infection
The very name of the disease already makes it clear that the source of infection is a variety of viruses. These can be herpes viruses, influenza, Coxsackie viruses, ECHO viruses, adenoviruses, enteroviruses and others. Therefore, the disease is conventionally divided into adenoviral, influenza and herpetic.
The disease is highly contagious: you can become infected during a conversation, by sneezing, through dishes, toys, and food. Viruses that enter the body reach the surface of the tonsils and settle there. From the moment of infection, the patient remains a source of infection for another 30 days. Many factors increase the likelihood of developing the disease:
- cold season;
- improper and unbalanced diet;
- lack of personal hygiene;
- hypothermia (for example, caught in the rain, eaten cold ice cream);
- smoking in front of a child;
- bad ecology;
- climate change;
- weak immunity;
- the presence of a chronic source of infection in the body (for example, chronic tonsillitis);
- carious teeth;
- allergic reactions;
- tuberculosis, diabetes and other diseases;
- stressful situations.
Sore throats caused by influenza viruses or adenoviruses usually occur during the cold season, especially during outbreaks of epidemics, when the body's defenses weaken. Herpetic sore throats are more common in the summer. In order to understand in time that we are dealing with viral tonsillitis, it is necessary to be able to distinguish the main symptoms of the disease in a child.
Sore throat in children: forms and clinical manifestations
Depending on the nature of the change and the degree of damage to the tonsils, several forms of angina are distinguished.
Catarrhal sore throat
A mild form, characterized by enlargement and redness of the tonsils, as well as the absence of purulent lesions. The child feels dry mouth, a whitish coating appears on the tongue, and the cervical lymph nodes are slightly enlarged. In addition to a sore throat that gets worse when swallowing, the child feels a sore and burning sensation. The temperature rises to 38 degrees, children complain of weakness and headache.
Follicular tonsillitis
A serious disease in which the tonsils become covered with purulent pinpoint follicles. On days 2-3, the ulcers open, leaving wounds that heal quickly. There is severe pain in the throat, radiating to the ear, making it difficult to swallow, children refuse to eat and drink. The lymph nodes are enlarged and painful when pressed lightly. Fever and chills are accompanied by a temperature of up to 40 degrees, vomiting, convulsions and fainting are possible.
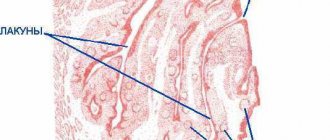
Lacunar tonsillitis
In the lacunae, between the lobes of the tonsils, islands of yellow purulent plaque appear, which tend to unite into wide purulent foci. The symptoms are similar to those of purulent follicular tonsillitis, but are more pronounced and are accompanied by severe intoxication of the body. It hurts the child to turn his head, his mouth opens with difficulty, which makes speech slurred.
Viral (herpetic) sore throat
Most often, the development of the disease is facilitated by vitamin deficiency and weakened immunity. The tonsils become covered with red blisters, which burst, leaving small ulcers in their place. In addition to a sore throat, symptoms are acute respiratory in nature: cough, runny nose, abdominal pain, indigestion, as well as stomatitis and conjunctivitis. Lack of timely treatment of herpetic sore throat in children can lead to serous meningitis.
Fungal tonsillitis
A relatively mild form of sore throat that occurs in children under 3 years of age. It is distinguished by a coating of white, curdled flakes on the tonsils and, with proper treatment, goes away within a week.
What causes the disease
In adults, in most cases (from 50 to 80%) sore throats are caused by viruses. And in children, bacterial sore throats are more common. They are more severe and often lead to complications. It's all about a harmful microorganism called "group A beta-hemolytic streptococcus." When it “sticks” to the tonsils and interacts with the lymphoid tissue, a new substance is formed, the structure of which is similar to our own tissue. The body understands that something foreign has entered it and needs to be dealt with. But in the end, it produces antibodies against its own tissues, which are similar to the structures that appeared as a result of the activity of the microbe. It kind of confuses them. That is why, as a result, not only the throat suffers, but also the joints, heart, kidneys and other organs and systems. Therefore, angina is considered a general disease with a predominant lesion of the palatine tonsils. And if hospitalization is necessary, a patient with a sore throat is sent to the infectious diseases department, not the ENT department of the hospital.
Why is a sore throat dangerous?
As practice shows, only in half of the cases are enlarged tonsils and sore throat caused by purulent sore throat. Many diseases, such as diphtheria or Epstein-Barr virus, have symptoms similar to sore throat. Therefore, only a qualified doctor with modern diagnostic equipment and a well-equipped laboratory can accurately determine the disease and prescribe the necessary treatment.
Each causative agent of sore throat is sensitive to a certain type of antibiotics prescribed by a doctor depending on the diagnosis.
Remember!
Incorrect or untimely treatment of sore throat in children, as well as relying on folk remedies for “red throat” can lead to serious complications and irreversible consequences.
Delay in diagnosis and prolonged treatment provoke the development of rheumatoid arthritis, vascular diseases, heart diseases (including rheumatic endocarditis), renal failure and many chronic diseases leading to disability.
Diagnostics
A consultation with an otorhinolaryngologist begins with collecting the patient’s medical history and complaints. The ENT doctor finds out how long the symptoms of inflammation have been appearing and whether any treatment has already been carried out. Direct examination includes palpation of the neck, parotid and occipital areas. Then the ENT doctor examines the oral cavity and pharynx. If necessary, an endoscopic examination of the pharynx is performed. He assesses the condition of the mucous membranes, palatine tonsils (their size, the presence of plaque on them or purulent plugs in them).
The patient may also be prescribed laboratory tests: a general blood test, a throat smear. If complications are suspected, serological blood tests, X-rays, electrocardiography, etc. are additionally performed.
After suffering a sore throat, a child may be diagnosed with myocarditis, arrhythmia, heart murmurs, pyelonephritis, renal failure, and rheumatism. If an infection from the tonsils enters the bloodstream and spreads throughout the body, sepsis may develop.
Complications of sore throat
The reason for the development of complications is often a late start of treatment, incorrect selection of antibiotics and a sharp weakening of the immune system2.
- Streptococcus has an allergenic effect on the body3, creates the preconditions for the development of nephritis (inflammation of the kidneys), myocarditis (inflammation of the heart muscle), rheumatism, manifested by the development of heart defects and inflammation of the joints, systemic connective tissue diseases, such as systemic lupus erythematosus, Sjogren's syndrome, systemic vasculitis , scleroderma.
- Aggressive streptococcus can penetrate from the tonsils into the surrounding tissues, causing the formation of paratonsillar and retropharyngeal abscesses, periadenitis (inflammation of the lymph nodes), phlegmon - diffuse purulent inflammation of the tissues.
- The list of complications of tonsillitis includes otitis (inflammation of the middle ear), sinusitis (damage to the paranasal sinuses).
- The infection can enter the blood, spread throughout the body and cause the formation of purulent foci in other organs (septicopyemia).
Sore throat and acute tonsillitis in children should be taken seriously.
Consultation with a pediatrician and ENT doctor is necessary in any case, even if at first glance the patient’s condition does not cause much concern!
Self-medication is fraught with the development of complications - all parents should understand this.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Sore throat. Tonsillitis, tonsillitis or...?
Authors : Snitsar Andrey
What, are these different things? Who cares? Tonsillitis and tonsillitis are acute inflammation of the palatine (most often) tonsils. I’m not talking about cross-sectional ones, but ask a medical student, a GP (general practitioner, family doctor), a specialist - an ENT specialist, and even an inexperienced infectious disease specialist, and in response you may get a bewildered shrug of the shoulders: it doesn’t matter, don’t engage in scholasticism.
I love this topic in my teaching work; I often ask this question to students. And “mine” know the difference, but they learn it later, after the discussion. The immediate answers are:
— Tonsillitis is a chronic disease, and tonsillitis is acute.
To this I answer that I mean acute tonsillitis. They are thinking.
— Tonsillitis is not a purulent inflammation, but a sore throat is purulent.
“No,” I say. - And tonsillitis can be purulent, and tonsillitis can be catarrhal, without purulent overlays.
Silence.
And it’s rare that someone in the group will say that a sore throat is of streptococcal etiology, and tonsillitis... not only. And even if he says it, the thought still stalls further, does not develop, there is no generalization, no understanding of the importance of the nuance. And the point is precisely in etiology, i.e. in the cause that caused the inflammation. But again, not only this. Confused? Be patient. And still, the reader will now be indignant: so what? Who cares? It’s still inflammation, the treatment is still the same - antibiotics. Why are you, doctor, casting a shadow on the fence! And I actually opened a medical website at random (not Wikipedia!) and read: “Sore throat (in everyday life) is an acute infectious disease primarily affecting the tonsils, caused by bacteria, viruses and fungi. Synonym: acute tonsillitis." That is, the truth doesn’t matter to them.
I don't agree, sorry. And I will try to convey my thoughts.
Sore throat is an independent disease, a separate nosological form. It was isolated because it is common and only affects the tonsils. The key word is ONLY. Sore throat, difficulty swallowing, purulent plaque on the tonsils, as a result - general symptoms: fever, intoxication (weakness, pain in the joints, muscles) ... everything!
Everything else, when in addition to damage to the tonsils there are other complaints and symptoms - tonsillitis. Doesn't matter? OK. Let's begin.
Diphtheria. At first glance, everything is the same: sore throat, plaque on the tonsils, temperature, intoxication... But! A completely different pathogenesis, the key role of the exotoxin, fatal damage to the heart, kidneys and nervous system, except for the tonsils, the damage to which is relatively insignificant (experts, do not be indignant! - I am now emphasizing the differences) - in this case they play only the role of localization of the pathogen - diphtheria sticks, which sits in them and produces poison (the same exotoxin). And it is he, carried by blood, that is the cause of all disasters and deaths. And most importantly - here it is! - different treatments! An antibiotic - yes, but without anti-diphtheria serum the patient will most likely die or remain disabled. But there is no need to treat a sore throat with serum.
Mononucleosis. At first glance, everything is the same: ... I won’t list it - see the paragraph on diphtheria, as in the future. In addition to the tonsils, the blood system, liver, spleen, and the entire lymphatic system are affected - multiple enlargement of the lymph nodes (and not just those next to the tonsils), a protracted course, fraught with long-term unpleasant consequences if the disease is not diagnosed in time and correctly treated - up to oncology and paralysis. It is often “missed” and treated like a sore throat. And the disease is viral. That is, antibiotics are not needed, the treatment is completely different - antiviral drugs and even hormones in severe cases.
Adenoviral infection. The only ARVI infection that can be accompanied by plaque on the tonsils, which means what is the immediate diagnosis? That's right, sore throat. The reason is a virus, as the name suggests. In addition to the tonsils, there is damage to the eyes and lymph nodes, liver, and respiratory tract. Often rashes, as with mononucleosis. And these rashes do not alarm clinicians at all: a sore throat with a rash is an allergy! This is where the diagnostic search ends. There may be pneumonia, which will never happen with a sore throat, as well as a cough or runny nose. A cough or runny nose is no longer a sore throat!
More about “allergic sore throats”, i.e. rash. Scarlet fever, measles and other numerous childhood exanthemas (these are the same rashes in a clever way), if accompanied by damage to the tonsils. Acutely contagious diseases, in which, unlike sore throats, it is imperative to take into account the epidemiological environment and the possibility of developing epidemics, the danger of “missing” them, especially at the beginning, in the first isolated cases. Here we are talking about the health of not just one person, but many - a greater responsibility. And I don’t advise my colleagues to make mistakes. Sanitation station fines are the least evil (although I don’t know if there is anyone to fine now, or if the country is in complete order: no SES - no problems). In addition, the complications of these infections are quite formidable and specific: from damage to the heart and kidneys in scarlet fever to meningoencephalitis in measles. And if you are treating a sore throat, do you think about possible encephalitis? And you miss it. And if I remember about the Landry-Guillain-Barre ascending paralysis... Brrr!
By the way, it is interesting that both sore throat and scarlet fever are of streptococcal etiology. It would seem that scarlet fever should be classified as a sore throat - it’s the same pathogen. But we agreed that the main criterion for this classification is damage to other organs and systems, in addition to the tonsils. And the clinical picture of scarlet fever is very specific: complications are more frequent, faster and more severe. Why is this so if there is only one pathogen? Or erysipelas is also a streptococcal infection, but the skin is affected... And scarlet fever does not recur, but erysipelas and sore throat - as much as you like. This is a topic for a separate conversation, very exciting and interesting. Another time somewhere in the future somehow another time sometime later…
Fungal infection of the tonsils. It also has its own nuances for a specialist: a characteristic coating in the form of scattered semolina, combined damage to other mucous membranes - the oral cavity and not only. If “not only” (esophagus, gynecology - thrush, onychomycosis - nail damage), and even if it recurs, then we remember immunodeficiency. Sometimes HIV infection debuts with such “sore throats”. Important? If you take the risk of missing out, you’ll end up taking the prophylactic course of ART yourself. Antibiotic therapy in this case aggravates the process rather than cures it. Moreover, these tonsillitis often develop after previous antibiotic therapy.
Who has heard of “Duguet’s sore throat” ? Well, of course, infectious disease specialists know. For other specialists, this eponym has been completely erased by the daily routine, although in the institute course on infectious diseases you were told about specific tonsillitis in typhoid fever, caused by the typhoid bacillus, because it generally affects lymphoid tissue, which includes the tonsils. Well, how do you feel about the prospect of not recognizing typhoid fever? Okay, it’s contagious and also epidemic. Antibiotics for S. typhi are specific - they do not treat a common sore throat, and without them there are complications... Intestinal bleeding and perforation (a hole, in other words) - peritonitis and death.
Another eponym, but more recognizable. Angina Simanovsky-Plaut-Vincent . Here, if you don’t diagnose, nothing really bad will happen. By and large, it can be classified as tonsillitis, and not tonsillitis - only the tonsils are affected by a specific pathogen - a spirochete. But! Very often this is a one-sided ulcerative process (only one tonsil is affected), and this is already interesting, it can be confused. At the beginning of the differential diagnostic list are paratonsillitis and paratonsillar abscess . Here LORiki are at their best, and the GP doctor must not miss it and refer to them in time - the abscess must be opened, otherwise... Well, at the end of the list... well, for example, syphilis . One-sided, beautiful, neat primary chancre on the tonsil, similar to Vincent’s ulcer. Are there still retarded people who consider cunnilingus a perversion? That prose of life! And we treat, we treat... What, it doesn’t go away? And some kind of pale rash appeared - like a starry sky... Ah-ah-ah, this is already the third course of antibiotics! Allergy! Right now, let's add L-cet - just one tablet a day. ...Why is that nose sunken in?..
You can also remember about tuberculosis - also more often a one-sided process. Yes, the damage to the tonsils is exclusive to him. But we are entering the era of multidrug-resistant tbc, i.e. in fact, its forms that were abundantly encountered in the pre-antibiotic era and which we have completely forgotten about. Previously, this form of tuberculosis was described, and quite often, usually against the background of a developed process in the lungs.
Speaking about unilateral lesions, we must remember about tonsil cancer . Rarely, yes. But aptly - late diagnosis, metastases and... “What fool treated you? It’s so elementary!” Yes, the last doctor is the smartest. And the smartest of all is the pathologist. In my memory there were three cases, and I will say that at first glance... that's right, tonsillitis. There are, of course, nuances: it’s been a long time, it doesn’t hurt too much (that’s why they don’t go to the doctor for a long time), there is no temperature, the blood is uncharacteristic... But you know, this damn symptom is plaque on the tonsil! — outweighs everything. They don’t undress, they don’t examine... Sore throat! All!
Lesions of the tonsils in other non-infectious processes. It’s not a sore throat at all, but you can’t tell the difference by looking at it. Unless they usually write “ulcerative-necrotic”. That’s when “ulcerative” also needs to be differentiated from Vincent’s sore throat. What could we be talking about?
Agranulocytosis . Often manifests itself as a sore throat. The disease is more likely hematological. A condition of a sharp, sometimes critical, incompatible with life decrease in the number of neutrophils - nuclear leukocytes - in the blood. For various, not always clear reasons, most often due to the toxic effects of medications. Mostly dangerous are the group of non-steroidal anti-inflammatory drugs (be careful with swallowing paracetamol, ibuprofen and aspirin!), but antibiotics are also not uncommon. Important? After all, we see a sore throat and... that’s right, let’s add more antibiotics and increase the toxic effect. Moreover, the sore throat is severe, necrotic, and accordingly we prescribe powerful, reserve antibiotics, intramuscularly, or better yet, intravenously. My grandmother, about 20 years ago, died within two hours of being in the hospital, I remember it for the rest of my life.
By the way, grandparents very rarely get tonsillitis. Why? An interesting question, the topic of the next conversation. If you see a sore throat in an elderly person, doubt it and then remember about non-infectious options: cancer, agranulocytosis, leukemia, systemic diseases, as well as fungus, immunodeficiency against the background of some other pathological processes, including oncology of a different localization...
Acute leukemia also often debuts with tonsillitis. Diagnosis, like agranulocytosis, is by a simple clinical blood test. But we must appoint him! You can even get a “C”, but in our clinic the rule is only full grade. At the same time, we’ll look at atypical mononuclear cells (ATM), characteristic of mononucleosis, then we won’t miss it. And never put off this test until the morning (remember your grandmother? We immediately gave her a test, the diagnosis was correct, hormones were administered, but...).
Leukemia is white blood cells 30 and above, not to be confused with leukocytosis in sore throats (almost this high never happens, well, 12–15) and leukemoid reactions (specific formula). Agranulocytosis is the opposite: leukocytes are zero to one point ten, and they are all due to lymphocytes, there are no rod segments. Urgently - hydrocortisone in combination with dexamethasone into a vein (the first is faster, the second is more powerful) and no antibiotics! And urgently a hematologist. Maybe you'll have time. We also had successes, not just deaths.
I’ll also say about thermal, chemical and mechanical damage to the tonsils . More often it occurs in children who are unlucky with overly loving and active mothers and grannies - they aggressively force them to breathe with their mouths open over a vat of boiling potatoes, cover them with a blanket on top (steam burn), give them boiling water with a magic green pharmacy (official medicine is the machinations of the pharmaceutical mafia, weed - that’s salvation!) or mercilessly rub the tonsils with a finger (spatula, spoon) wrapped in gauze dipped in Lugol’s solution (alcohol, soda, salt, antibiotic, tincture of Kalanchoe, aloe, some other “E” - underline as necessary) ) - combined chemical-mechanical injury. Among adults, it is found in strong “men” who use one remedy for all diseases - tsedvaashpyatyoash in different forms. Most often in my practice I have encountered moonshine, and they prefer strong, at least 70 degrees - this certainly helped. There was also pure alcohol - an excellent disinfectant!
What's happening? The integrity of the mucous membrane and in particular the capillaries is compromised. Through the holes in them, fibrinogen comes out along with the blood plasma, which instantly turns into fibrin outside the vessel and forms the same fibrinous deposits as in diphtheria - the mechanism is identical, except that damage to the capillaries in diphtheria is caused by an exotoxin, not injury. These plaques are difficult to remove, when removed they bleed and reappear, often spreading beyond the tonsils (after all, it is not the tonsils alone that are subject to burn-trauma, but also the surrounding mucous membranes), which makes us seriously worried about diphtheria (how many such cases were there in the 1990s !). So the simple question “what was the treatment?” with additional detail (rarely does anyone remember about moonshine of their own free will, as well as about executions of children - it’s somehow inconvenient) it’s not even superfluous - the most beautiful differential diagnosis is obtained, the students are “just in capture.”
If you try hard, you can remember a dozen more nosologies, but I think that the main idea is clear. Hearing a patient complain of a sore throat and seeing plaque on the tonsils, it is too early to diagnose a sore throat. How often is this exactly what happens in a crowd under the outpatient clinic, 12 minutes per patient, a busy schedule of operational activities (I’m talking about ENT specialists), complaints and hassle, paperwork, parallel solutions to economic problems imposed by the head physician, “inconceivable everyday life”...
But there are other reasons that are less excusable. This is laziness of the mind, forgetfulness, reluctance or inability to think, ignoring symptoms that do not fit into a convenient and quick scheme, the apparent simplicity of the diagnosis and the presence of one single symptom - plaque on the tonsils.
The patient needs to undress, examine the skin in search of a rash (it may not be abundant and invisible, in hard-to-reach places the patient may not notice it and, accordingly, does not complain), palpate the liver, spleen, lymph nodes of other groups, listen to the lungs, and most importantly - ask smart , focused questions. Not for show, but logically flowing from your living medical pulsating thoughts and one from the other, strung together, like the rings of a child’s pyramid, onto the core of a completed diagnosis. Graceful and correct. And then there will be no medical error, an annoying oversight, for which you are first of all ashamed of yourself... Believe me, I am not lecturing, I am far from boring edification. I just went through it. I was ashamed and hurt. And I want both you and I to have fewer such cases.
And for this, I propose to use the scheme I proposed, or, if you like, classification, which is very practical and helps to understand the difference between tonsillitis and tonsillitis.
Sore throat is a separate, complete diagnosis; tonsillitis is just one of the symptoms that requires speculation. And it is possible to say that a patient has tonsillitis only by excluding all diseases in which it could be tonsillitis (see above + a dozen more). Nothing! So it’s long and difficult! Did you think it was easy to be a doctor? Easy... This, guys, is just an “apparent appearance.”
You could probably call them something else, but, in my opinion, this is a rational option. On the same site they called it this way: “anginas are divided into primary (ordinary, simple) and secondary - sore throats due to diphtheria, mononucleosis, scarlet fever...”.
Well, that's nonsense!
What is this secondary sore throat with diphtheria?!
I hope you agree now that this is not a scholastic question, but a very practical one, closely influencing the choice of treatment tactics, allowing you to avoid unnecessary mistakes, complications and even deaths. Including thought and alertness.
A request to colleagues - respond, let's discuss. Maybe I’m wrong about something, I’m ready to listen to your points of view.
And a request to the crossing communities. The topic raised is quite difficult and specific. Perhaps understandable only to doctors, although I have tried to replace and interpret complex medical terms. It seems to me that the main thing you should take away from this story is that sore throat is not such a simple disease for which there is no point in going to the doctor. Everything is supposedly easy: you have a sore throat, the pharmacist at the pharmacy will recommend an antibiotic, let’s drink it, and everything will go away. And look how many diagnoses with unpronounceable names are found under its mask, sometimes even fatal if not recognized and treated incorrectly. Antibiotics do not always help, it’s good if they are simply useless, and sometimes they are critically harmful .
You need to be able to understand these problems. I didn’t write all this so that you could take a short course in infectious diseases and not worry us. Quite the opposite - so that you understand how difficult it is, and do not shoulder a heavy burden of responsibility for yourself and your loved ones. Leave it to us, we studied for it. Do not engage in self-diagnosis and self-medication, do not seek help from neighbors, friends and medical charlatans.
Source
published 06/30/2019 19:30 updated 07/02/2019 — Tests and examinations, Diseases, doctors, treatment and medicines, Infectious diseases, Respiratory diseases, Infectious diseases
Treatment of viral sore throat
Before treatment, it is necessary to diagnose and identify the pathogen. If the viral nature of the occurrence is confirmed, then, as a rule, the treatment regimen is as follows:
- Taking antiviral drugs. They speed up the fight against viruses and reduce recovery time. Basically, the ENT doctor prescribes tablet forms of drugs, but in severe cases injections are used.
- Taking antihistamines. They reduce the severity of intoxication and reduce swelling of the throat.
- Use of painkillers, anti-inflammatory non-steroidal drugs.
- Taking antipyretics based on ibuprofen or paracetamol. Recommended only when the temperature rises above 38°C.
- Taking immunostimulants. To strengthen and restore the patient's immune system, immunostimulating agents are prescribed. In addition, they enhance the effect of antiviral drugs. Children are prescribed in the form of drops or suspensions.
- Gargling. Gargling with herbs, antiseptics, and ready-made preparations reduces pain in the throat and eliminates inflammation.
The otorhinolaryngologist recommends drinking as much water, fruit drinks, warm tea, juices, and herbal infusions as possible, since the disease causes dehydration. The liquid removes toxins and viruses from the body.
Throughout the illness, you should stick to bed rest and not have a sore throat on your legs. If you follow bed rest for 2-3 days, the recovery time is significantly reduced, and improvement in well-being occurs on the second day.
The air must be humidified and the room ventilated. It is imperative to adjust your diet, namely to exclude smoked foods, spicy foods, too hot or cold foods, which will irritate the inflamed tonsils.
Usually the disease goes away completely within 6-7 days.
Causes of viral sore throat
As a rule, the virus enters the body when the body’s protective functions are reduced. Immunity may decrease after recently suffering from influenza, acute respiratory viral infections, as well as nutritional disorders (exhaustion). The following factors reduce the body's resistance to viruses:
- Poor nutrition and ignoring vegetables and fruits.
- Staying in an unventilated area. It is for this reason that preschoolers get sick.
- Stress.
The virus can enter by airborne droplets, contact, household and waterborne routes. Children often become infected with viral sore throat when visiting a swimming pool, kindergarten, or school. In close contact with a sick person, the likelihood of getting sick doubles.
Bacterial or viral?
In addition to viral origin, the disease can be caused by bacteria: streptococci and staphylococci are normally present in the microflora of the oral cavity and begin to multiply uncontrollably during the inflammatory process. The latter may be caused by caries or periodontitis (read more about the disease in the article).
How to distinguish viral stomatitis from bacterial one? It is extremely difficult to do this at home, so it is better to consult a doctor. The main differential feature is the localization of the rash. With viral herpetic stomatitis, vesicles with transparent contents first appear on the tongue (its tip, along the side surfaces and under it), and then can even spread to the pharynx and tonsils.
For bacterial stomatitis, the location of the rash on the gums and those areas where the skin borders the mucous membrane (for example, on the red border of the lips) is more common. Also, with a disease caused by streptococci, “jams” are often observed - pustules on the corners of the mouth, which quickly begin to bleed, become covered with a crust, crack and cause constant discomfort while eating and talking.
Types of diagnostics
An experienced doctor can identify herpetic stomatitis in adults during an initial examination, relying on only two methods.
- Clinical picture.
Based on the totality of the patient’s specific complaints and distinctive external signs, the dentist will not only assess the severity of the disease, but also differentiate it from ordinary stomatitis, candidiasis, etc. - Immunofluorescence.
Express microscopy method, the most accurate for diagnosing acute herpetic stomatitis.