Odontogenic sinusitis is an inflammation of the maxillary sinuses that develops from infected teeth of the upper jaw. The penetration of infection is also facilitated by dental manipulations in the area of the maxillary sinuses - treatment and extraction of teeth, implantation and sinus lifting. Without identifying and eliminating the cause, standard treatment by an ENT doctor in a clinic does not bring results. Treatment of odontogenic infections must be comprehensive!
Doctor Levin Center has been specializing in the treatment of patients with combined ENT and dental pathologies for more than 20 years. Comprehensive rehabilitation programs are carried out by maxillofacial surgeons with otolaryngological training.
Causes of odontogenic sinusitis
The maxillary sinuses (maxillary sinuses) are separated from the oral cavity by a thin layer of bone in which the roots of the upper chewing teeth are located. Such close proximity poses a threat of sinus infection. In 15% of cases, the apices of the roots are anatomically located under the mucous membrane of the sinus, without a bone layer, which further increases the risk of developing odontogenic sinusitis.
Conventionally, the reasons can be divided into 2 categories:
Delayed dental treatment
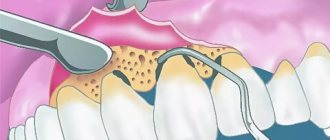
With pulpitis and periodontitis, infection from the dental canals slowly but surely spreads to the surrounding bone tissue. Without treatment, foci of infection grow, melt the bone septum, opening the “gate” for the penetration of pathogenic microflora. In advanced situations, cysts form on the roots of teeth, and when the bone barrier is destroyed, they grow into the sinus.
Medical errors
As a result of dentist errors, mechanical damage to the sinus floor is possible (perforated form of the disease). The result is the formation of a communication with the sinus, the penetration of foreign bodies with the body’s response in the form of odontogenic sinusitis.
The most common treatment errors after which patients turn to our Center:
- Unsuccessful endodontic treatment The therapist did not calculate the effort during mechanical cleaning and filling of dental canals. There was a fracture and pushing of the instrument and/or removal of the filling material beyond the root apex into the lumen of the sinus.
- Traumatic tooth extraction The surgeon, without preliminary diagnosis, having no idea about the location of the roots, damaged the bone septum. Perforation of the sinus floor occurred, often with the tooth or its fragments falling into the sinus cavity.
- Implantation without sinus lift Experimental implantation protocols without prior bone grafting result in damage to the sinus floor by the implant. If the perforation goes unnoticed during surgery, the implant flies into the sinus.
- Sinus lift without diagnostics The surgeon did not calculate the bone tissue parameters and did not assess the condition of the mucous membrane. During the preparation of the bone septum, its perforation and rupture of the membrane occurred. Bone material ended up in the sinus cavity.
Odontogenic maxillary sinusitis - symptoms and treatment
Often, treatment of odontogenic maxillary sinusitis is carried out using a combination of conservative and surgical methods. The method of treatment and its volume depends on the causative factor and the course of the disease.
For odontogenic sinusitis caused by acute or aggravated periodontitis, treatment often consists of eliminating the causative factor and prescribing drug therapy. To eliminate the cause of inflammation, endodontic treatment of the root canals of a diseased tooth is performed, followed by filling.
In case of extensive destruction of the coronal part of the tooth, its strong mobility, as well as the patient’s refusal to preserve the causative tooth, its extraction (removal) is carried out. If by the time of treatment the patient has developed a purulent form of sinusitis, a puncture of the maxillary sinus is performed with evacuation of purulent contents and daily washing of the sinus with antiseptic solutions. Drug therapy is prescribed. In the catarrhal form of acute maxillary sinusitis, sinus puncture is not required; drug therapy and lavage through the natural anastomosis are prescribed.
Treatment of odontogenic maxillary sinusitis is usually an interdisciplinary problem: the disease is jointly treated by dental therapists, dental surgeons, maxillofacial surgeons and otolaryngologists. The number of specialists depends on the severity of the disease.
For odontogenic cysts of the maxillary sinus, the presence of filling material and other foreign bodies in the lumen of the maxillary sinus without oroantral communication (pathological communication between the sinus cavity and the oral cavity), surgical treatment is indicated. There are several types of operations on the maxillary sinus.
Radical maxillary sinusotomy according to Caldwell-Luc. Under general anesthesia, the mucous membrane and periosteum in the vestibule of the oral cavity are dissected from the canine to the second molar. A raspatory is used to skeletonize (expose) the bone tissue, after which the anterior wall of the maxillary sinus is trepanned (created access). The burr hole is expanded to 1.5*1.0 cm, the mucous membrane of the anterior wall of the sinus is excised and all pathological tissues and fluids are removed from the sinus: pus, polyps, foreign bodies, cyst membrane, blood clots, etc. This type of operation requires extremely careful execution, because it is necessary to remove all pathological tissue in the least traumatic way, without affecting the healthy mucous membrane of the sinus. Also, during the operation, an additional communication is created between the sinus cavity and the nasal cavity, into which tubes are subsequently installed for subsequent rinsing with antiseptic solutions. Afterwards, the postoperative wound is sutured and drug therapy is prescribed. The material obtained during the operation is sent for pathohistological and bacteriological examination. According to the literature, this surgical method has complications in the postoperative period in 80% of cases [18]:
- replacement of ciliated epithelium with scar tissue;
- fusion of the natural anastomosis with the nasal cavity;
- impaired sensitivity of teeth and adjacent soft tissues;
- trauma to the nasolacrimal duct;
- lacrimation;
- osteomyelitis of the upper jaw and zygomatic bone.
With a gentle micromaxillary sinus, an incision of about 8 mm is made in the area of the canine fossa, the anterior wall of the maxillary sinus is trepanned, the hole is widened for the introduction of an endoscope and endoscopic surgical instrument. The maxillary sinus is sanitized (cleansed), foreign bodies and pathological tissues are removed under endoscopic control. This method makes it possible to achieve adequate sanitation of the sinus cavity with minimal trauma.
A more modern surgical intervention is trocar sinusotomy, in which a puncture of the mucous membrane in the area of the canine fossa is performed, followed by trepanation of the anterior wall of the maxillary sinus and insertion of a trocar (an instrument designed to penetrate into the body cavity through the integument) into the resulting hole, through which an endoscope and endoscopic instruments are inserted. instruments for surgical sanitation of the sinus. With micromaxillary sinusotomy and trocar sinusotomy, an additional anastomosis is not applied.
Methods for sanitation of the sinus through the natural anastomosis without punctures and incisions are possible; such treatment methods are carried out by otolaryngologists.
Special attention should be paid to the treatment of perforated forms of maxillary sinusitis, as one of the most common forms. At the moment, there are many ways to close perforation of the floor of the maxillary sinus, many of which only slightly differ from each other in the methodology. All techniques pursue the following goals:
- reliable closure of the perforation hole;
- relapse prevention;
- prevention of the formation of persistent oroantral anastomosis.
The most commonly used are various variations of defect replacement with a cheek flap. The point is the same:
- sampling of the mucous membrane of the alveolar process of the upper jaw;
- formation of a mucoperiosteal flap, its mobilization (creation of mobility) and movement to the palatal surface, followed by suturing.
The obvious disadvantage of this method is that it provides only soft tissue regeneration in the area of the perforation hole [19]. Also, the disadvantages of this method include the loss of attached keratinized gum (an immovable cuff, a barrier that protects the tooth and the bone around it from the traumatic effects of food bolus, penetration of microbes and other factors). In addition, the operation can lead to a decrease in the depth of the vestibule of the oral cavity (the space of soft tissue between the lip or cheeks and the elements of the dentofacial row), which threatens the development of gingivitis, periodontitis, the formation of malocclusion, loosening of teeth and other pathologies.
To preserve the attached keratinized gum and the depth of the vestibule of the oral cavity, a palatal flap on a pedicle began to be used. The disadvantages of this method include extensive trauma and a large wound surface of the hard palate. In this regard, splitting of the palatal mucoperiosteal flap is currently widely used. However, these methods also do not allow restoration of lost bone tissue volume. To restore the bone tissue of the alveolar process in the area of the perforation hole, various synthetic and natural bone replacement materials are used.
How to avoid
There are only two ways to prevent the development of odontogenic sinusitis:
- Treat your teeth in a timely manner, prevent infection of the dental canals and spread of inflammation beyond the apex of the tooth root.
- Contact proven clinics with experienced doctors, the opportunity to conduct a thorough diagnosis and provide for an emergency situation.
In our Center, not a single dental procedure, especially at the border with the maxillary sinuses, is performed without a thorough X-ray examination using a computed tomograph.
The study is carried out using
a high-precision Sirona device with the Galileos diagnostic software package.
Based on the results of computed tomography, we determine the location of the roots and the size of the bone septum. This makes it possible to plan treatment in such a way as to avoid risks.
Tooth extraction operations and other interventions in the area of the maxillary sinuses in our Center are performed only by maxillofacial surgeons with ENT training . Deep knowledge of the anatomy of the maxillary region allows you to avoid mistakes that a regular dentist might make. But each case is individual, and even if something goes wrong, our doctors are always ready for any turn of events and correct the situation.
Diagnosis of maxillary sinusitis
The diagnosis is made by an otolaryngologist based on the patient’s complaints, examination (rhinoscopy), and also based on the results of:
- X-rays, linear, computer or magnetic resonance imaging, and orthopantomograms (panoramic images) of teeth.
- General blood test.
- Diagnostic puncture. In the laboratory, the obtained material is examined, identifying the infectious causative agent of the disease.
- Video endoscopic examination. An endoscope is inserted through the puncture, with which the doctor looks at what is happening inside.
Symptoms of odontogenic sinusitis
Inflammation from infected teeth develops gradually and in the initial stages is most often asymptomatic. If dental treatment has been carried out, symptoms may also not appear immediately - it all depends on the body’s immune system and reaction to foreign bodies. There are cases that sinusitis does not make itself felt for several years.
But sooner or later the infection will make itself known. The symptoms of odontogenic sinusitis are practically no different from rhinogenic sinusitis (when the infection enters through the nose as a result of a cold, flu or acute respiratory viral infection):
- pain and swelling in the sinus area
- nasal congestion and difficulty breathing
- purulent or mucopurulent discharge
- headaches, especially when bending forward
- decreased sense of smell
- temperature up to 39o
An unsuspecting patient first turns to an ENT specialist, but he needs to see a dentist. However, there are points that indicate the odontogenic origin of sinus inflammation:
- pain in the chewing teeth of the upper jaw, especially when chewing
- there was treatment or removal of teeth at the border with the sinuses
- implants or sinus lift were installed
The most important distinguishing feature is that only one sinus is bothering you , which is associated with bad teeth or dental treatment. In this case, first of all, you need to solve dental problems. As a rule, the symptoms of sinusitis disappear within two weeks after eliminating the source of inflammation.
Navigation
In ENT practice, there are cases when a patient comes to an otolaryngologist with complaints of severe nasal congestion and suppuration from the nasal cavity. At the same time, the patient has an elevated body temperature and headaches. But the ENT doctor, having examined the patient, sends him to see a dentist. “Why?”, you will be surprised. Because in this case we are dealing with odontogenic sinusitis.Sinusitis is a type of sinusitis. The development of sinusitis of odontogenic nature is not associated with colds or acute respiratory viral infections. The main cause of the disease is bad teeth. First, the development of inflammatory tooth disease occurs, after which the inflammatory process from the upper jaw extends beyond the oral cavity and is localized in the maxillary sinus.
Such a state cannot be tolerated. Timely detection of symptoms and diagnosis carried out by a competent ENT doctor will allow timely diagnosis of dental sinusitis and avoid serious complications.
What are the maxillary sinuses
The maxillary sinuses (also called the maxillary sinuses) are special cavities on both sides of the nose that are filled with air.
Each cavity is connected to the nasal passage by small openings called anastomoses. The cavities are covered with mucous membrane. The function of mucus is to trap bacteria and harmful particles in it, and then remove them from the body through those same anastomoses. When edema occurs, the excretory opening becomes very narrow, as a result of which mucus, along with harmful particles and bacteria, cannot come out and stagnates. At this time, the patient begins to experience bursting pain in the cheek area - this is how inflammation of the maxillary sinus begins. Treatment of the maxillary sinus should not be neglected, since inaction can provoke serious consequences, including sepsis and meningitis. Classic sinusitis can be bilateral, when both sinuses are affected. In the odontogenic form, the inflammatory process starts in the sinus on which side the diseased tooth is located.
Types of odontogenic inflammation
The disease begins with a serous form.
It is characterized by swelling of the mucous membrane, nasal congestion, dilation of capillaries, and increased secretion production. Swelling of the tissues leads to a narrowing of the anastomosis, the mucous masses do not find a way out and mucus with pathogenic contents accumulates in the sinus. This is how serous inflammation turns into purulent inflammation. There are also acute and chronic forms of the disease. Chronic odontogenic sinusitis occurs due to improper treatment of acute sinusitis. Chronic odontogenic sinusitis lasts for years, worsening during a decrease in immunity or when infected.
Odontogenic sinusitis is diagnosed by an otorhinolaryngologist, and treatment is carried out by two specialists: a dentist and an otorhinolaryngologist.
Causes of odontogenic sinusitis
It is very easy to understand why acute odontogenic sinusitis occurs - just look at the anatomy. If you look at the structure of the skull, you can see: the 5th, 6th and 7th teeth of the upper jaw are located very close to the maxillary sinus. There are cases that these teeth even go into her cavity. An infection in a tooth easily thins the already small distance between the tooth and the wall of the sinus and easily penetrates inside, thus starting the inflammatory process.
Development in acute form occurs due to the following reasons:
• Improper oral hygiene. The most common cause of the disease is neglect of basic rules of oral care: improper and irregular brushing of teeth, delaying a visit to the dentist when there are problems with the teeth. At particular risk are those patients who have been diagnosed with an advanced form of caries with developing necrosis of the dental nerve. • After tooth extraction. Infection after tooth extraction is associated with the formation of a fistula - a small channel through which the infection enters the maxillary sinus. This occurs when the roots of a diseased tooth enter the maxillary cavity. • Incorrectly installed seal. Unfortunately, there are cases when the development of inflammation is facilitated by the inept actions of insufficiently qualified dentists. Part of the filling can get into the sinus, and it will immediately be perceived by the body as a foreign particle, and the inflammatory process will start. If after visiting the dentist you have a runny nose, you need to consult an otolaryngologist. • Oral diseases. Caries, gum disease, periodontal disease, the presence of cysts are all diseases in which there is a source of infection on the oral mucosa. • Reduced immunity. Decreased immunity leads to the activity of bacteria that are constantly in the oral cavity.
Symptoms of the disease
The symptoms of the disease are similar to classic inflammation of the maxillary sinuses. Only a highly qualified otolaryngologist will be able to distinguish odontogenic sinusitis from ordinary sinusitis.
Signs of odontogenic sinusitis are:
• constant nasal congestion;
• purulent nasal discharge with a characteristic odor; • the appearance of odor from the patient’s mouth; • pain in the cheek area under the eyes; • acute toothache in the upper jaw; • increased body temperature. Symptoms also include a general deterioration in well-being, a persistent feeling of fatigue, and problems sleeping. Specific symptoms of purulent odontogenic sinusitis are pain when lightly pressing on one of the cheeks or when lightly tapping on the teeth located in the area of the inflamed sinus.
Chronic odontogenic sinusitis is manifested by discomfort in the affected sinus area. In general, the patient feels satisfactory until a period of exacerbation occurs.
Diagnosis and treatment
Treatment of an inflamed maxillary sinus, like any other disease, begins with diagnosis and determination of the causes that led to the inflammatory process.
Odontogenic sinusitis is an insidious disease that must be treated under the supervision of an otolaryngologist. He will identify the exact cause of the disease and tell you how to treat the disease. Diagnosis begins with examination of the sinuses. To identify and treat a diseased tooth that has caused inflammation, the patient is sent for an X-ray examination, and in especially severe cases, a computed tomography scan. Effective treatment consists of several stages. Traditionally, the first stage of treatment is to eliminate the cause of suppuration. If the root cause of the disease is a problematic tooth, then at the initial stage the disease is treated by tooth extraction. Extraction is carried out in dentistry - before removing a tooth, you need to approach the choice of clinic with all responsibility, since an inexperienced doctor can only aggravate the situation.
If we are dealing with perforation of the maxillary sinus and penetration into it, for example, of part of the material for filling a tooth, then surgical treatment is indicated. The operation is performed to remove a foreign body from the sinus and subsequently eliminate the defect site.
If sinusitis without perforation, in order to release the purulent mass from the sinus, a puncture (puncture) of the maxillary sinus is performed.
Elimination of symptoms involves taking antibacterial drugs, rinsing the nasal cavity, using vasoconstrictor drops, and also performing physical procedures.
A highly qualified ENT doctor, modern equipment and a flexible pricing policy are the three components of the success of our clinic.
If you are faced with the problem of sinusitis, do not delay visiting the doctor!
Be healthy!
What is the danger of the disease
Without proper treatment, a chronic inflammatory process with pathogenic microflora develops in the sinus, destroying the sinus mucosa and surrounding bone tissue. Since the maxillary sinuses are located close to anatomically important structures, severe complications can arise:
- Orbital The upper wall of the sinus is in contact with the lower wall of the eye orbit. The infection spreads into the orbit with the formation of an abscess and phlegmon. As a result, optic nerve neuritis develops, deterioration or complete loss of vision.
- Intracranial The most dangerous complications associated with the penetration and impact of infection on the brain. Meningitis, encephalitis, and abscess develop. If detected and treated untimely, irreversible consequences, including death, can occur.
Foci of infection provoked by the presence of a foreign body can cause a precancerous condition.
Treatment
The treatment of odontogenic sinusitis requires an integrated approach. As a rule, treatment requires the simultaneous participation of an otolaryngologist and a dentist. Isolated antibacterial and conservative therapy lead only to temporary relief of the condition and removal of the severity of the process.
For a complete recovery, it is necessary to eliminate the source of infection - remove or treat the causative tooth while simultaneously sanitizing the inflamed sinus.
In case of foreign inclusions in the sinus (filling material, sinus lifting material, fungal bodies), their complete removal is necessary. For this, endoscopic techniques are used. They allow you to remove these formations through the nasal cavity. If there is a connection between the sinus and the oral cavity (oroantral fistula), it must be closed using special bioinert collagen-based membranes and mucosal flaps.
Why you should entrust treatment to the ENT department of dentistry
ENT dentistry is a symbiosis of two medical areas, a multidisciplinary approach to the treatment of inflammation of the maxillary sinuses of odontogenic origin. Only an experienced maxillofacial surgeon with ENT training can make an accurate diagnosis and create a sound rehabilitation plan.
As a rule, odontogenic causes of sinusitis are simply ignored during routine examination by an otolaryngologist. Treatment in a city clinic without high-quality diagnostics or in the absence of it at all turns into a multi-part series with monthly visits to an ENT doctor, dragging on for many years, causing inconvenience and worsening the quality of life.
Unified drug therapy or traumatic sinus punctures are prescribed, which, if they bring relief, are for a short time. Inflammation from the acute stage becomes chronic with periodic exacerbations. A person runs from one doctor to another to no avail, but without identifying and eliminating the cause, odontogenic sinusitis cannot be cured !
Can a dentist diagnose sinusitis?
In case of pulpitis, the patient finally comes to the dentist. The doctor fills the canals, removes the nerve, but part of the infection still remains in the apical delta - after all, it has penetrated there a long time ago!
The apical delta is a branching at the tips of the roots that can never be adequately sterilized. And if a tooth has many roots, then, naturally, the entire system of root canals is one, like the root of one tree.
Therefore, if an infection gets into a tooth, it is already inside.
And it’s normal that the body fights it, and the sinus mucosa begins to thicken. In the process, some people develop granulomas, others - cysts. But cysts are changes in the periodontium, and the mucous membrane itself begins to thicken and degenerate.
Sometimes it happens that polyps are formed - spherical thickenings on a stalk. Hypertrophy of the columnar epithelium may occur. That is, as a result of chronic inflammation, many, many layers are formed.
The dentist can conduct a computed tomography scan, but it can only identify changes in the mucous membrane in volume - simply establish the presence of this fact.
And only an otolaryngologist can say what exactly happened there. To do this, you need to conduct an endoscopic examination.
But in most cases, it is the dentist who is the first doctor to detect sinusitis on a CT scan.
When a person realizes from various symptoms that he has inflammation in the sinus, he also learns about this from the dentist.
Diagnostics
The odontogenic form of sinusitis often remains undetected by ENT specialists due to the lack of highly accurate diagnostics and banal ignorance of the “dental” cause of the disease. Such gaps lead to the fact that even after medical and surgical treatment the person continues to suffer.
Differential diagnosis is extremely important, which allows you to determine the form of sinusitis and select the appropriate treatment.
Only computed tomography provides informative 3D images for visualizing bone and adjacent soft tissues, the condition of the teeth, the presence of foreign bodies and neoplasms in the sinus.
In our Center, CT scans are performed on a Sirona Gallileos dental tomograph with ENT mode settings.
In some cases, it will be necessary to study the microbial composition of the sinus lining to rule out a malignant process.
Types of odontogenic inflammation
The disease begins with a serous form. It is characterized by swelling of the mucous membrane, nasal congestion, dilation of capillaries, and increased secretion production. Swelling of the tissues leads to a narrowing of the anastomosis, the mucous masses do not find a way out and mucus with pathogenic contents accumulates in the sinus. This is how serous inflammation turns into purulent inflammation.
There are also acute and chronic forms of the disease. Chronic odontogenic sinusitis occurs due to improper treatment of acute sinusitis. Chronic odontogenic sinusitis lasts for years, worsening during a decrease in immunity or when infected.
Odontogenic sinusitis is diagnosed by an otorhinolaryngologist, and treatment is carried out by two specialists: a dentist and an otorhinolaryngologist.
Stages of treatment
We strive to carry out all activities comprehensively in one day, so as not to delay the patient
- Sanitation of the oral cavity Preparation to maintain sterility during surgery to avoid secondary infection - retreatment of compromised teeth, hygienic cleaning.
- The operation is performed by a maxillofacial surgeon in a sterile operating room of the ENT department - “in your sleep”, according to the selected access protocol. A follow-up CT scan after surgery is required.
- Prosthetics If the protocol requires the removal of teeth, we install temporary orthopedic structures to close the aesthetic defect so as not to leave the patient without teeth.
Recovery after surgery
No hospitalization
A hospital stay for 2-3 days after surgery (as happens in city hospitals) is not required.
Gentle surgical protocols, the use of modern functional equipment and a microscope allow treatment to be carried out as delicately as possible .
All operations are performed in a controlled, drug-induced sleep - this is not general anesthesia ! Recovery from the state is easy, without dizziness, memory loss or clouding of consciousness. The drugs are absolutely safe for the body and are eliminated naturally 40 minutes after stopping the supply.
For patients with vascular and cardiac problems, a day hospital , where you can calmly recover and recover under the supervision of our anesthesiologist-resuscitator.
Accelerated rehabilitation
Recovery after the intervention occurs within a week. For those who want to speed up the process, our Center provides a set of procedures to reduce pain, resolve hematomas and swelling - carried out on the day of surgery.
Home care
Medications are prescribed - antibiotics, painkillers and decongestants. To prevent the patient from running to pharmacies in a postoperative state and to avoid purchasing counterfeit products “on the side,” the entire package of drugs is collected and given out free of charge .
The package contains all the necessary medications for taking and caring for the surgical area.
Please follow the recommendations and do not skip taking medications to avoid complications. The instructions are in the medicine package.
If you suspect a worsening condition, contact the clinic immediately. The telephone number for the 24-hour patient support service is listed in the memo.