Causes of pain
After pulpitis, a tooth hurts for several reasons - damage to the tissues surrounding the tooth root (periodontal) or an inflammatory process.
Tissue damage can be caused by the following circumstances:
- formation of a wound surface during removal of the neurovascular bundle of a tooth;
- treatment of root canals with antiseptic agents if the antiseptic leaves the canal.
Can a tooth hurt after pulpitis due to the dentist’s dishonest work? The inflammatory process can occur due to poor quality work by the doctor. Signs of poor treatment of pulpitis on an x-ray are:
- incomplete filling of root canals, when there is still free space left to the apex;
- excessive filling of root canals, when the filling material extends beyond the apex of the root canal;
- extra holes in the root canals.
Pulpitis
A common symptom for all types of pulpitis is severe pain, especially with changes in temperature and continuous or intermittent toothache at night.
Acute focal pulpitis
characterized by paroxysmal pain, with clear localization and long intervals of intermission. Attacks of pain in acute focal pulpitis are mostly short-term, pain occurs from exposure to temperature stimuli. The pain intensifies at night, which is a characteristic symptom of all pulpitis. The examination reveals a deep carious cavity, the bottom of the cavity is painful during probing. The electrical excitability of the pulp is reduced on the side in which focal pulpitis is localized.
For acute diffuse pulpitis
attacks of pain are longer, light intervals are insignificant. Diffuse pulpitis differs from focal pulpitis in more intense pain at night. The pain intensifies in a lying position, the pain can radiate to different areas, depending on the location of the diseased tooth. On examination, the carious cavity is deep with pain along the entire bottom during probing. The response to temperature stimuli in acute diffuse pulpitis is sharply painful, but in some cases cold reduces pain. Percussion of a tooth affected by pulpitis is generally painless. The electrical excitability of the pulp is reduced in all areas, including at the bottom of the carious cavity. It is these electrical excitability data that help to accurately determine the type of acute pulpitis.
Chronic pulpitis has less pronounced symptoms and a blurred clinical picture. So with chronic
In fibrous pulpitis, attacks of pain from various irritants are insignificant and short-lived. During a survey of the patient, it turns out that the tooth had pain before, and the symptoms of pain corresponded to acute pulpitis. With chronic pulpitis, spontaneous pain is rare, mainly due to impaired outflow of exudate. The reaction to cold is slow, and pain is sometimes observed with a sharp change in ambient temperature.
Probing the bottom of the carious cavity confirms the presence of communication between the carious cavity and the tooth cavity. The electrical excitability of a tooth with chronic fibrous pulpitis is reduced, and an x-ray image confirms the rarefaction of bone tissue at the root apex.
Chronic gangrenous pulpitis
clinically manifested by pain in the tooth while eating hot food or when exposed to other temperature stimuli. Patients with gangrenous pulpitis complain of rare spontaneous pain and an unpleasant putrid odor from the mouth. In the anamnesis there are complaints of acute pain of a paroxysmal nature with irradiation along the trigeminal nerve. During examination of a tooth with chronic gangrenous pulpitis, it is discovered that the carious cavity widely communicates with the tooth cavity. Probing a carious cavity is painful throughout the entire depth of both the coronal and root pulp. The depth of the lesion is determined by the degree of prevalence of gangrenous pulpitis and the deeper the lesions with gangrenous pulpitis, the lower the degree of electrical excitability of the pulp. In half of the cases with gangrenous pulpitis, X-ray images reveal destructive changes in the periapical tissue; the severity of the destruction depends on the depth of the pulpitis.
For chronic hypertrophic pulpitis
subjective sensations are practically absent. Patients complain of bleeding from the overgrown pulp tissue and minor pain while eating. There is a history of complaints of acute paroxysmal pain, which is characteristic of focal or diffuse pulpitis. When examining a tooth affected by hypertrophic pulpitis, it is clearly visible that the crown of the tooth is destroyed, and a hypertrophically altered pulp protrudes from the carious cavity. Superficial probing is almost painless, but with deep probing the pain intensifies. The periapical fissure on the X-ray image is unchanged.
During exacerbations of chronic pulpitis, spontaneous paroxysmal pain occurs. Often, during a relapse, patients complain of prolonged intense pain from various external stimuli. The pain radiates along the trigeminal nerve; at rest, the pain is usually aching in nature, which intensifies when biting with an antagonist tooth. The patient's medical history includes manifestations of acute and chronic pulpitis. During the examination, it becomes clear that the carious cavity and the tooth cavity form a single whole, the cavity is open, and probing the pulp is sharply painful. With exacerbation of chronic pulpitis, the electrical excitability of the pulp is reduced, and on the radiograph the expansion of the periodontal fissure is clearly visible. Bone loss in the periapical zone is a characteristic manifestation of chronic recurrent pulpitis.
Untreated pulpitis can lead to pulp necrosis, spread of the inflammatory process to the peri-apical tissues and the development of periodontitis.
When there is no need to see a doctor
Why does a tooth hurt after pulpitis? The appearance of pain is due to the increased trauma of the entire procedure, which consists of opening the tooth, removing pulp from the root canal and filling the empty space with artificial material - a filling.
How long does a tooth hurt after pulpitis in normal condition? Without pathologies, the pain persists for 5-10 days, and it gradually subsides. It is considered normal when:
- after pulpitis, the tooth hurts without increasing pain;
- there is no bleeding, swelling, swelling or redness, general weakness, or fever.
How is canal filling performed?
High-quality filling is the key to the absence of complications in the future. Before filling, the canals must be prepared: widen them slightly and ensure patency along the entire length.
Preparation consists of the following steps:
- elimination of tissues on which carious formations have appeared (removal of healthy tissue is allowed in order to gain access to the orifices);
- complete removal of the pulp;
- correct determination of the channel length (they are different in length);
- high-quality mechanical processing (includes expanding the diameter of the channel along the entire length);
- filling with gutta-percha.
The quality of the filling depends on:
- Correct determination of the channel length. In case of a dentist’s mistake, the canal may be either underfilled, which subsequently leads to the formation of cysts, or overfilled when the material extends beyond the boundaries of the root (consequences - pain, inflammation).
- High quality machining. The purpose of the procedure is to widen the canal so that it can be filled with filling material to its full length. Treatment can be carried out either using hand instruments, which the doctor rotates in the canal with his fingers, or using an endodontic tip (rotating in the canal, they remove a thin layer from the walls, gradually expanding it). This option is the most preferable, since the quality of processing increases and safety increases (the tip cannot break off due to automatic control of the load level).
- The chosen filling method and the doctor’s competence.
The patient can understand without the help of a doctor how well the canal was filled. To do this, you need to carefully look at the x-ray:
- The filling material will appear as a rich white color. This color should fill the channel throughout its entire length;
- in a properly sealed canal there should be no voids or gaps.
Reviews about our doctors
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020
Recovery period
Once treatment for pulpitis is completed, the patient will need some more time to fully recover - from one week to a month. During this period, physical therapy is indicated, for example laser therapy using a helium-neon apparatus. This is necessary to speed up the healing process and consolidate the therapeutic effect.
Since pulpitis is an inflammatory disease, after treatment in the clinic it is necessary to take a course of non-steroidal anti-inflammatory drugs at home, such as: Ibuprofen, Ketanov, Naproxen-Acri. However, it should be remembered that all anti-inflammatory and painkillers have their contraindications, so the choice of a specific medication must be agreed with your doctor.
Content:
- Abnormal factors causing the problem 1.1. Traumatic injury 1.2. Mistakes made during filling 1.3. Tool fragment 1.4. Wall perforation 1.5. Periodontitis
In certain cases, pain after pulpitis treatment may be normal.
Even if during the procedure the entire pulp was completely removed and there seems to be nothing left to hurt, discomfort may still occur. Why is this happening? It's all about getting the treated tissues used to the filling composition embedded in them. If the intervention was carried out efficiently and in compliance with all standards, the unpleasant sensations will soon go away on their own.
If the pain does not subside, but, on the contrary, becomes more severe, increases every day, the gums are swollen, and other dangerous accompanying symptoms appear - this is a reason to consult a dentist. It is quite possible that the inflammatory process is progressing in the tissues, which is important to stop as quickly as possible.
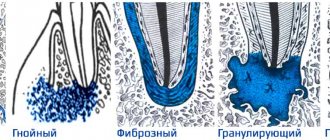
ETIOLOGY AND PATHOGENESIS
This disease is an advanced and most severe form of acute serous inflammation of the pulp. It can also develop as a result of caries: microorganisms contribute to the formation of pus in the carious cavity from the existing serous exudate: a purulent-inflammatory abscess develops.
To avoid such complications, it is important to identify and properly treat carious cavities in a timely manner. And for prevention, it is necessary to monitor dental hygiene to avoid the formation of plaque and tartar.
The infection can enter the pulp through the arteries entering the root canal. The cause of hematogenous infection of the pulp can be osteomyelitis, influenza complicated by capillary toxicosis, etc.
There are focal (partial damage to the pulp) and diffuse (complete damage to the pulp) purulent pulpitis. If measures are not taken, the destructive process may affect neighboring teeth.
What not to do?
If, after treatment, a tooth hurts when pressed or without mechanical action, you should under no circumstances resort to folk remedies such as heating, hot compresses, heating pads - if there is an inflammatory process, this can greatly worsen the condition. In case of allergic reactions, heat will also increase swelling.
It is also not recommended to use folk remedies for rinsing, which can cause a burn to the mucous membrane - iodine, tinctures of alcohol or vodka, liquids with the juice of “scorching” plants, etc. Even if there is no gum damage, such measures can worsen the situation.
It is also not worth taking various painkillers uncontrollably - firstly, you need to see a doctor in any case, and the effect of analgesics will not allow you to fully evaluate the clinical picture. Secondly, it can be dangerous to health.
It is important to visit a doctor at the first opportunity and perform all the necessary procedures to eliminate unpleasant consequences and improve the condition.