- Tooth extraction
- Removal of a tooth cyst
- Bone tissue augmentation
- Resection of the apex of the tooth root
- Installation of a dental implant
- Installation of a mini-implant
Patients have more chronic dental diseases than acute ones. Advanced caries, pulpitis, periodontitis lead to the fact that after a few months or years the patient is faced with a neoplasm on the root of the tooth or its acute inflammation. In this case, resection helps to save the tooth.
When should tooth resection not be performed?
- The main condition for successful root resection is the presence of sufficient jaw bone volume in the patient - at least 5 mm, otherwise there is a risk of jaw fracture.
- A tooth root resection operation will be ineffective if the patient has chronic periodontitis and/or periodontitis, as well as mobility of the diseased tooth.
Tooth root resection is contraindicated if:
- Large cysts or granulomas, when they reach the size of a third of the tooth root or more.
- A completely destroyed dental crown, if the tooth cannot be replaced with prosthetics.
- Close proximity of the roots of healthy teeth.
- Severe mobility of the diseased tooth.
- Some common diseases, such as diabetes, blood diseases, heart diseases, immunodeficiency conditions.
Preparing for surgery
Before agreeing on the operation, the dentist will prescribe a number of additional tests and examinations. The goal is to ensure that the patient has no absolute contraindications and to pre-develop a strategy for the procedure. You will definitely have to do:
- cardiogram. Resection of the root apex is strictly contraindicated in cases of cardiac arrhythmias, so no sane dental surgeon will undertake the operation without confidence that the patient is able to tolerate it normally;
- blood clotting test. The operation requires a fairly deep and long-term intervention. Of course, any qualified surgeon is able to cope with bleeding in the process, but there is no need to improvise without reason;
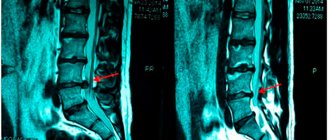
- radiography. The photo is needed for three reasons. Firstly, for absolute certainty that the patient has periodontitis and surgical intervention is justified. Secondly, to determine the exact location of the cyst or granuloma and make the incision in the gum and the hole in the bone tissue minimal. Thirdly, to understand how close the maxillary sinuses are to the apex of the root (their damage during the operation is extremely undesirable);
- examinations by specialized specialists (cardiologist, hematologist, otolaryngologist), other tests at the discretion of the attending physician, depending on the individual characteristics of the patient.
If periodontitis is not the only problem, before resection of the apex of the tooth begins, it is necessary to treat all other organs of the oral cavity. In particular, the following may be carried out:
- hygienic cleaning (if there is plaque or stone deposits on the enamel);
- canal filling;
- installing crowns on other teeth;
- any other dental procedures if relevant defects are identified.
Do I need to do a resection or still remove the tooth?
Tooth root resection is a tooth-preserving operation. The dentist will recommend it to you when there is at least the slightest opportunity to save the tooth. If the dentist does not see this possibility, then the conversation will immediately focus on removal.
When will the tooth have to be removed?
- You have a large cyst that affects more than a third of the tooth or several teeth.
- The root of the tooth is destroyed.
- There is severe inflammation of the tissues adjacent to the diseased tooth.
- The tooth is movable.
- Subsequent prosthetic replacement of a diseased, destroyed tooth with a crown is impossible.
Features of postoperative rehabilitation
After such surgery, the patient should refrain from any physical activity for 24 hours. Eating food is allowed only after 3 hours. Subsequently, care must be taken to ensure that the oral cavity is not exposed to thermal irritants, to limit the consumption of spicy and salty foods, as well as the use of overly aggressive means for rinsing and brushing teeth.
Swelling may persist for 1-2 days and moderate pain may be felt. To prevent the development of a purulent and inflammatory process, antibacterial agents and antiseptic solutions are prescribed, which must be used to thoroughly rinse the mouth. After 6 months you should undergo an x-ray examination.
How is tooth root apex resection performed?
For the patient, resection of the apex of the tooth root is a simple operation and the procedure is tolerated quite easily.
First, the doctor makes an incision in the gum and bone tissue of the jaw to create access to the tumor. After which the tumor itself is removed along with the affected part of the tooth root. The entire cavity is thoroughly cleaned so that not even a small amount of infected tissue remains and is treated with an antiseptic.
Synthetic bone replacement materials are placed into the resulting space, which will take root over time and completely restore the patient’s bone.
Next, the wound is closed with a special self-absorbing membrane and the gum is sutured.
In order to protect the injured area, a bandage may be applied to the gum for up to 1 week.
After surgery, the patient may experience swelling of the gums and pain when chewing, which normally should subside within a few days.
Healing of the mucosa usually occurs in 7-10 days, the bone is restored in approximately 3-4 months.
Why should you agree to resection?
Before the development of a technique for eliminating inflammation in the deep layers of bone tissue by cutting off the root tip, there were no alternatives to tooth extraction. Despite the flourishing of dental prosthetics and implantation, an artificial organ will never become a complete replacement for a natural one.
Therefore, if, after an examination, a specialist says that resection of the apex of the tooth is necessary, rest assured: this is so. Refusal to undergo surgery will certainly result in irreversible loss of the affected organ.
What to do after tooth root resection?
Root resection is well tolerated by patients and does not cause major problems even in the postoperative period, but it is necessary to follow a number of rules that will alleviate the condition and speed up recovery.
Typically, after surgery, patients are prescribed antibiotics and vitamin supplements. They must be taken strictly as prescribed by the doctor.
It is necessary to maintain gentle but regular oral hygiene and use antiseptic rinses.
You can't overwork your body. During the healing period, it is better to limit physical and emotional stress.
Do not eat hot or hard food, it should be warm and soft.
Advantages of ultrasonic root resection PIEZOSURGERY:
- Vessels and nerves are not damaged, since the ultrasound system acts only on the bone and does not injure soft tissues.
- Bone tissue is not rejected, since it is completely synthetic and not cadaveric or animal.
- There is no allergy to the implanted synthetic bone.
- There is no burn or injury to bone tissue, since the bone is not cut out using a cutter or drill.
- There is no unpleasant smell of burnt bone during surgery.
- Ultrasound will completely remove infected, altered tissue from the root apex and will not leave an infection.
- There are no relapses - the cyst is removed forever with a 100% guarantee.
- Laser bone sterilization is the key to complete cleansing of bacteria.
Methods and stages of removing teeth or their roots
Most often in modern dentistry, only two methods of removing teeth or their roots are practiced:
- removing a tooth from the gum using forceps;
- rocking of the tooth and its rotation around its axis by elevators.
In cases where the roots are deep, the gum tissue can be cut with a scalpel. In general, the process of removing teeth or their roots is divided into the following stages:
- separation of the round ligament from the neck of the tooth (ligamentotomy);
- applying (installing) forceps to the tooth;
- advancing the fixing elements of the forceps under the gum;
- final fixation of the forceps;
- rotation (rotation) or luxation (swaying) of the tooth;
- extracting a tooth or its roots from the socket.
Many patients are frightened by the phrase “gastric resection”. How justified are these fears?
Longitudinal gastrectomy is not at all the same resection that is performed for cancer or peptic ulcer disease. With PRG, the lateral part of the stomach is removed, while the important physiological valves of the stomach (cardiac sphincter and pylorus) are preserved, and thus the stomach after PRG remains physiologically quite functional. From a voluminous sac, the stomach turns into a narrow tube, where food does not stay long and quickly passes into the intestinal tract. The secretory activity of the stomach, of course, decreases, but this also plays into the hands of the goal of weight loss.
What is the difference between PRJ and more complex operations?
Cholecystectomy
- Cost: 100,000 - 160,000 rubles.
- Duration: 25-30 minutes
- Hospitalization: 3 days in hospital
More details
A patient who has undergone pancreatic cancer usually does not require lifelong doses of vitamin and mineral supplements that are absolutely necessary after gastric bypass or biliopancreatic bypass. The likelihood of metabolic side effects (protein, vitamin and calcium deficiency) is also less here. PGC does not require removal of the gallbladder, although if gallstones form in the gallbladder during weight loss, this may be necessary later. At the same time, if we talk about the stability of weight loss, biliopancreatic bypass undoubtedly leads here. Due to the fact that the operation of prostate cancer is relatively young, no one can yet say how stable its results are after 5-10 or more years. Therefore, we warn all patients who are considering the option of longitudinal gastrectomy that if over time the result of PRG turns out to be insufficient, a second stage of treatment may be required - gastric bypass or biliopancreatic bypass. In this case, the second stage will be easier to complete, since the “gastric” stage of biliopancreatic bypass has actually already been completed.
Are postoperative complications possible? What is their probability?
It is impossible to guarantee the absence of complications with any operation. In case of prostate cancer, a staple suture is placed along the entire stomach. Although these sutures are performed using high-quality staplers and are always reinforced, there is still a small risk of postoperative bleeding, as well as failure (cutting through) of some sutures, which in rare cases may require laparoscopic or surgical revision. To prevent suture insufficiency in the first two weeks after prostate cancer, nutrition should be in liquid form, without undue stress on the gastric sutures. Since the operation takes place in the area of the splenic hilum, we always warn that if significant bleeding occurs from the spleen, it may be removed. We also warn about this during other gastric surgeries performed due to obesity.
In what situations can longitudinal gastrectomy be the operation of choice?
Longitudinal gastrectomy can be considered as the operation of choice in patients with relatively moderate excess weight (with a body mass index of 35 to 45), in patients with severe concomitant diseases, as well as in other situations when performing more complex operations is risky for one reason or another reasons. PRG can be offered to patients regardless of age, including adolescents and the elderly. In our country, gastric banding has proven itself well in cases where gastric banding did not produce the desired results.
How much does tooth root removal cost in Moscow?
The cost of tooth root removal is determined individually, as it depends on how complex the case is. In the dental department of the multidisciplinary clinic CELT, it starts from 800 rubles for a simple removal and ends at 10,000 rubles for a complex removal of a 2nd degree dystopic tooth. You can view our basic prices in this section of our website. In order to find out the exact cost of tooth root removal in our clinic in Moscow, consult our specialist.
In the dentistry of the CELT clinic, you can get a consultation with a dental surgeon, undergo an examination and remove the roots of the teeth, if there are indications for this. We will eliminate any dental problems effectively and absolutely safely.
Removing the root of a decayed tooth
Cases where a root remains after tooth extraction are not uncommon. Its removal is a difficult and unpleasant procedure for the patient, even despite the effectiveness of modern anesthesia. Fortunately, the need to remove tooth roots does not always arise. If the root is healthy enough, it is treated and prosthetics are performed. However, removing a rotten tooth root is simply necessary, since its preservation will entail a number of problems:
- Halitosis (bad breath);
- A breeding ground for infection in the oral cavity, possible damage to neighboring teeth;
- The appearance of subgingival stone;
- Spread of infection to the maxillary sinuses, development of osteomyelitis;
- The appearance of cysts and granulomas at its apex ( removing a tooth with a cyst on the root
is a complex procedure); - A decrease in the body’s overall immunity due to the fact that it is forced to constantly fight the source of inflammation.
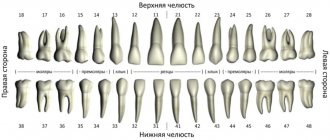
In order to properly plan the operation, our dentist performs an x-ray examination. The operation itself is performed using local anesthesia, dental forceps or an elevator. Removing the roots of the front teeth
is carried out using rotational movements, and lateral movements using rocking. The most complex cases may require additional manipulations, the use of burs and special microsurgical dental instruments. Removing the roots of the teeth of the lower and upper jaw is a more complex procedure than removing a whole tooth. It requires special training, which consists of examination, diagnosis and sanitation of the oral cavity. The treatment plan is drawn up based on diagnostic studies and the patient’s indications.
How likely is heartburn (reflux - esophagitis) to occur after prostate cancer? How to deal with this?
Firstly, the probability of reflux of stomach contents into the esophagus largely depends on the volume of resection, i.e. the larger part of the stomach is removed and the more the stomach looks like a narrow tube, the less the danger of reflux of gastric contents into the esophagus. Secondly, reflux esophagitis can be effectively treated and prevented with the help of antiulcer drugs (omez, quamatel, ranitidine, pariet, etc.) that inhibit gastric secretion. Such treatment can be prescribed for a period of 2 - 3 months after surgery, and then only if necessary. We are not proponents of additional “anti-reflux” interventions. They are justified only when it comes to large diaphragmatic hernias.