According to antiplagiat.ru, the uniqueness of the text as of October 16, 2018 is 99.9%.
Key words, tags: X-rays, tooth extraction, orthopantomogram, periodontitis
A dental cyst belongs to the group of jaw cysts. Jaw cyst is a general concept that unites many pathologies. The formation of a cystic cavity in the jaw can be caused by an inflammatory process, or in rare cases, by a growing tumor. It can be in a “dormant” state and not manifest itself in any way, or, on the contrary, be in an active, acute phase, get sick, affect neighboring healthy tissues, and cause various diseases. In any case, the presence of cysts in the jaw and, in particular, the presence of a dental cyst, requires attention and serious consideration.
Tooth cyst: historical background
The word “cyst” is of Greek origin (“kystis”) and literally means “bubble.” A dental cyst is a cavity-like tumor-like formation. Previously, when X-rays were not taken, it was extremely difficult to see such formations and, as a rule, dentists encountered them during the extraction of teeth from patients. Thanks to the advent of X-ray diagnostics at the end of the 19th century (1895), it became possible to plan the treatment of dental cysts. And today, if a patient regularly visits the dentist’s office, we can successfully diagnose and eliminate dental cysts at those stages when they do not pose a danger.
Contraindications
Cystectomy is contraindicated in cases of intolerance to anesthesia and severe concomitant diseases of the heart, liver, kidneys, lungs, blood, diabetes mellitus, exhaustion, and systemic infections. In addition, partial cystectomy is not performed if a reduction in the working volume of the bladder is unacceptable for stage 0 cancer, as well as in cases where the tumor is located near the junction of the ureters and urethra with the bladder (there is no technical ability to ensure urinary function).
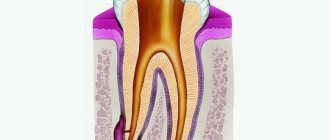
Tooth cyst: anatomy
A dental cyst is a benign cavity tumor-like formation that has a membrane and an internal epithelial lining, the cells of which produce fluid. Modern medicine still cannot accurately answer the question of how and where an incipient cyst takes epithelial tissue from. However, most scientists are inclined to believe that it comes from the remnants of the dental epithelium, the so-called islands of Malasse-Astakhov. And it develops as a result of chronic odontogenic inflammation, when microbes enter the jaw bone through the tooth canal. Further development of the process can go in two directions, the result of which are pathologies: an extensive destructive process that does not have a shell - a non-shell formation (such a process is not a cyst), or a dental cyst itself - a shell-like formation.
Robot-assisted RC in women
The position of the patient on the operating table, the localization of trocars and the technique of pelvic lymph node dissection are identical as in men. In women, two modifications of the operation are possible - with removal of the uterus and ovaries (anterior exenteration) or with their preservation.
Posterior dissection. The technique of posterior dissection in women depends on whether organ-conserving surgery is planned or not. With anterior exenteration, a transverse incision of the peritoneum is performed under the junction of the uterus and the posterior wall of the vagina, which expands bilaterally over the common iliac vessels. The uterus is retracted anteriorly using a 4 robotic arm. The ligaments along the ovarian stalk are identified and clipped with Hem-o-lock clips or divided using LigaSure. Next, the uterine arteries are isolated, clipped and divided. The uterus is retracted proximally, which improves identification of the area between the vagina and the uterus. This step is facilitated by manipulation of a vaginal tampon. After incision of the posterior vaginal fornix, its anterior wall is mobilized along with the uterus to the cervix of the vagina. The incision in the anterior vaginal wall continues distally to the level of the bladder neck. Thus, part of the anterior vaginal wall is removed en bloc along with the bladder. Careful closure and reconstruction of the vagina is essential to prevent pelvic organ prolapse and the development of a genitourinary fistula. To achieve good functional results, it is necessary to preserve the autonomic nerves along the lateral wall of the vagina, which are responsible for sexual function.
Robotic organ-sparing cystectomy in women. In the absence of tumor invasion closer to the uterus, an operation is planned to preserve it and the vagina, as well as the supporting ligaments and vessels of the ovaries. The peritoneum between the uterus and the bladder is opened transversely, the wall of the bladder is separated anteriorly from the cervix, and the anterior vaginal fornix is identified. Next, closer to the cervix, the anterior wall of the vagina is opened, part of it is removed along with the bladder. Mobilization is carried out until the neck of the bladder and urethra are separated from the vagina.
Lateral dissection of the bladder. After posterior dissection of the MP lateral to the umbilical ligaments, the MP is mobilized on both sides, which makes it possible to identify the vascular pedicles. The MP is carefully retracted using the fourth hand, allowing the MP vessels to be stretched, isolated, clipped or divided using LigaSure. First, the superior cystic artery is stopped, then the inferior one.
Anterior mobilization of the bladder and urethral dissection. Lateral dissection continues inferiorly to the perirectal space and further along the pubic bone. The endopelvic fascia is opened and the bladder is then separated from the anterior abdominal wall as described above. The urethra is identified and the dorsal venous complex is ligated. When planning orthotopic cystoplasty, the urethra is divided below the neck of the bladder to preserve the mechanism of urinary continence.
Types of dental cysts
It is customary to distinguish between 2 types of dental cysts - follicular and radicular. Follicular cysts are less common than radicular cysts. In the presence of certain factors, it grows from the dental follicle - the membrane around the growing tooth. When it is large in size and involves adjacent teeth, it is called a follicular dentigerous cyst.
Radicular (odontogenic inflammatory) cysts form on the roots of teeth as a result of pathological processes spreading beyond the root apex. By location, radicular cysts can be apical (root), lateral (lateral), apicolateral and interradicular.
The mechanism of formation and growth of a dental cyst
The cystic cavity, located in the jaw, has external resistance from the surrounding jaw bone. But the epithelial cells of the lining begin to produce fluid, which gradually fills the cavity, creating excess pressure.
This pressure acts on the surrounding bone tissue, causing its gradual peripheral resorption, giving the cyst the opportunity to grow even larger, increase fluid secretion, and therefore put even more pressure on the walls. This is why cysts can grow to very large sizes, sometimes asymptomatically, if not accompanied by periodic inflammation. This may be due to the patient’s good immune status, low pathogenicity of the microflora in the lesion and other factors.
Rehabilitation period and possible complications
Immediately after surgery, the patient can go home, as the procedure is performed under local anesthesia. After the anesthetics wear off, pain appears, which can be relieved with analgesics. You can relieve swelling with a cold compress.
In the first week, you need to eat liquid or soft food at a comfortable temperature. Spicy and sour foods and rough foods are prohibited. You cannot go to the bathhouse, the beach, take a hot bath, play sports or other increased physical activity, otherwise the wound may open and bleeding may begin.
Smoking is not recommended, as nicotine constricts blood vessels. Hygiene procedures should be done carefully, brushing your teeth with a soft-bristle toothbrush. It is useful to rinse your mouth with decoctions of chamomile, oak bark, sage, or just soda, salted water.
The most common complication is wound infection and associated consequences. Possible suture divergence, relapse of the disease, bleeding, damage to the nerve, roots of adjacent dental units.
Possible complications of a dental cyst
As the cyst grows, it can “push aside” nearby anatomical formations, such as the canal of the inferior alveolar nerve, and can disrupt the external contours of the jaw bones (plastic toy syndrome), thereby changing the contours of the face, that is, causing facial asymmetry. It may also involve other neighboring tissues in the pathological process. So, often, retrograde periodontitis develops in the teeth located next to the cyst. And if the cyst grows into the maxillary sinuses, chronic odontogenic sinusitis is formed, which can be asymptomatic for a long time, but, nevertheless, have a detrimental effect on health.
Robot-assisted RC in men
Position of the patient and localization of trocars. The patient is placed in the dorsal lithotomy position, the arms are placed along the body, the lower limbs are spread to the sides so that it is possible to bring the robot. The patient is adequately fixed to the table and placed in the Trendelenburg position at 30-450 (Fig. 1).
Figure 1. Position of the patient on the operating table
After induction of general anesthesia, the surgical field is prepared, a nasogastric tube and a sterile Foley catheter are installed. Correct placement of trocars is very important for the success of the operation. We used a 6-trocar technique with the camera port located 5 cm above the umbilicus in the midline. After insufflation of the abdominal cavity to 10-12 mm Hg. Art. under visual control, two robotic trocars were installed along the navel line on the right and left lateral to the rectus abdominis muscles. The left port is set 8 cm and the right port 10-11 cm from the midline, which provides more space for the assistant's trocar. The third of them is installed 7-10 cm lateral from the left port and 5-7 cm above the iliac crest. When performing intracorporeal urine diversion, this port is replaced with a 15 cm trocar for the stapler, which provides a better angle for resection of the small intestine and the formation of an interintestinal anastomosis. Two assistant ports are located on either side of the right robotic port. The location of the trocars is shown in Fig. 2.
Figure 2. Trocar position
Posterior dissection. Initially, both ureters are mobilized along the lower third from the area of intersection with the iliac vessels to the urinary tract. Closer to the juxtavesical portion of the ureter, two Hem-o-lock clips are applied, between them it is intersected and part of it is sent for pathomorphological examination (Fig. 3).
Figure 3. The left ureter is mobilized along the lower third and clipped
A ligature is applied to the proximal clip, which facilitates further manipulation when anastomosing the ureter with the reservoir. The vas deferens and seminal vesicles are then identified, the wall of the bladder behind the vesicles is mobilized to the Denonvilliers fascia, which is opened, and further dissection is performed between it and the rectum (Fig. 4).
Figure 4. Posterior MP dissection. A) Seminal vesicles. B) Rectum.
Retroprostatic dissection should be performed anterior to the prerectal fat to avoid rectal trauma. If the neurovascular bundles are not preserved, the seminal vesicles are left unchanged on the MP. In the case of nerve-sparing RC, they are allocated closer to the prostate, thereby avoiding damage to the neurovascular bundles, which are located laterally and close to the vesicles.
Mobilization of the bladder and prostate on both sides. After separation of the bladder from the rectum, the bladder is mobilized on both sides. The medial umbilical ligaments are identified closer to the abdominal inguinal ring. The peritoneum is divided laterally to the ligaments extending into the medial portions of the external iliac artery and into the space of Retzii. Using a combination of sharp and blunt dissection, the space between the lateral surface of the bladder and the lateral pelvic wall is widened until the pelvic fascia is reached (Fig. 5).
Figure 5. Excretion of the bladder along the lateral surface to the prostate
In this case, the urachus and umbilical ligaments should not be crossed so that the MP does not fall into the surgical field. The endopelvic fascia is then opened and the lateral surface of the prostate is exposed.
Clipping and intersection of MP vessels. The vas deferens is divided to provide access medial to the external iliac vessels, and lateral dissection is continued. Using the fourth arm, the MP is retracted cranially. With sufficient retraction, the lateral crura can be well identified for division with LigaSure or clipping with Hem-o-lock clips. First, the superior cystic artery is isolated and clipped (Fig. 6).
Figure 6. Clipping of cystic vessels
Next, the inferior cystic and vesicoprostatic arteries are mobilized. Isolation of the pedicles of the bladder ends on the superolateral portion of the prostate near the seminal vesicles while preserving the neurovascular bundles. They are located in the posterolateral part of the prostate and are easily distinguished all the way to the apex of the prostate. Nerve-sparing dissection for RC can be performed using a similar technique as for robot-assisted prostatectomy. The incision is performed in the periprostatic fascia and continues distally to the apex of the prostate. In this case, thermal injury or excessive traction of the neurovascular bundles should be avoided. Next, the vascular pedicles of the prostate are isolated and dissected between Hem-o-lock clips. This technique effectively preserves the lateral periprostatic fascia. We performed infrafascial dissection in patients with low prostate-specific antigen levels, and they did not have prostate cancer in our RC series.
Mobilization of the anterior wall of the bladder and urethra. The urachus and medial umbilical ligaments are coagulated with a bipolar dissector and divided. The anterior wall of the bladder and prostate are distinguished. The dorsal venous complex is ligated and divided, and apical dissection of the prostate and urethra is performed along the length (Fig. 7).
Figure 7. Mobilization of the prostate and urethra
Next, the Foley catheter is removed and a Hem-o-lock clip is placed on the urethra closer to the prostate to prevent urine or tumor cells from entering. Alternatively, a similar clip can be applied to the Foley catheter after tightening its balloon, which assists in traction of the bladder with the prostate (Fig. 8).
Figure 8. After cutting off the urethra, a clip is applied to the Foley catheter.
The released drug is placed in an endobag. The pelvis is washed with an antiseptic solution and hemostasis is performed by coagulation or suturing of bleeding vessels. After drainage is established, the drug is removed through the widened wound of one of the ports.
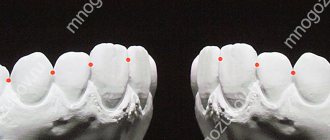
Diagnosis of a dental cyst
The choice of treatment method for a dental cyst is based on a multifaceted diagnosis, which may include:
— examination of the patient; - “targeted” x-ray of the tooth, which the patient indicates as the causative tooth; - orthopantomogram (panoramic image of the jaw bones), which allows you to see pathologies and the most likely places of their development in the upper and lower jaws, in the maxillary sinuses, in the canals of the nerve trunks; - in some cases - a computed tomogram, which allows you to see the facial skeleton and skull bones, joints, maxillary sinuses in three projections (frontal, sagittal and horizontal) and in a three-dimensional volumetric image.
Cystotomy and cystectomy in dentistry - what is it and what is the difference
Both operations are used for surgical treatment of cysts. The differences lie in the method of surgery and the final result of the procedure.
Features of the methods:
- During cystectomy, the tumor is radically removed, that is, completely removed. At the last stage, the wound is sutured.
- Cystotomy involves partial removal of the cystic wall and bone. The remaining capsule communicates with the oral cavity. After the procedure, the pressure inside the formation decreases, it flattens, and then gradually resolves.
The choice of method depends on the clinical case. A preliminary X-ray or computed tomography is performed to rule out contraindications.
Advantages and disadvantages of cystotomy:
- advantages - the procedure is easy to perform, low-traumatic, there is no risk of damage to nearby tissues and nerves;
- disadvantages - the duration of postoperative care, as additional cavities are formed, deformations, and jaw defects impair the cleansing of the mouth from microorganisms.
Advantages and disadvantages of cystectomy:
- advantages - complete removal of the capsule, suturing the wound, reparative bone regeneration;
- disadvantages - high trauma, risk of damage to adjacent teeth, nerves, blood vessels, maxillary sinus, accidental removal of a malignant tumor, autolysis of a blood clot in bone tissue cannot be ruled out.
Removal of a dental cyst. Historically significant and modern methods of surgery for removing dental cysts
Initially, the most common method of treating cysts was their removal. For this purpose, 2 fundamentally different methods were used: cystotomy and cystectomy.
Cystotomy (or the PARCH-I method) has historical significance in the development and establishment of medicine. Today this method is practically not used, but previously it was indispensable for removing large cysts. To avoid complications and its severe consequences, a wide channel was created between the cyst cavity and the vestibule of the oral cavity by suturing the edges of the cyst shell with the oral mucosa.
Cystectomy (or PARCH-II method) involves complete excision/removal of the cyst. This surgical intervention is often simultaneously accompanied by the removal of the root apex, the source of the formation of the cyst containing infected apical deltas. Today this method is the most popular.
The main goal of cystectomy is complete sanitation of the cyst cavity, which is not possible without resection of the root apex. The fact is that the root pulp in its apical third has an apical delta with an unclear structure and very fine branching of the canals, even in single-rooted teeth. If such canals can be cleaned during tooth treatment, then during retreatment this is almost impossible, especially considering the narrowness of the lateral deltas. Removing the root apex, in addition, allows you to most effectively clean the cyst cavity behind the root. This is especially true for teeth 12 and 22, which have a more curved root system. The operation is carried out as follows: using a small incision on the gum, the surgeon very carefully reaches the surface of the bone located above the cystic cavity, removes the wall with a trephine or bur, making sure that the neighboring teeth are not damaged, and then removes the cyst shell and performs a resection of the root apex . Next, sanitation of the cystic cavity is carried out and its subsequent revision for residual cyst particles. After this, in some cases, retrograde filling is performed. The final step in the operation to remove cystic formations is filling the resulting cavity with osteoplastic material and suturing the wound.
In the case of the formation of a large cyst, amputation of the apex of the tooth root can be performed, or half of the tooth and damaged root can be removed (hemessection), and in the case of an interradicular cyst, this can be done by corono-radicular separation.
How is the cystectomy procedure performed?
- Examination by a doctor of the damaged area, x-ray diagnostics.
- Conducting anesthesia. The operation is performed under conduction and infiltration anesthesia.
- Carrying out the operation. As a rule, with this intervention the tooth is completely removed.
- The dentist removes the cyst through the resulting hole.
- After curettage, the cyst needs to be filled. A special bone-forming drug is poured into the resulting cavity, aimed at accelerating the healing process. Also suitable for successful healing are xenografts or materials made from bone chips and the patient’s own blood.
- Applying a suture to the wound
- At the end of the cystotomy procedure, complex anti-inflammatory and antibacterial therapy is prescribed, as well as follow-up examinations (images are taken once a month to track the dynamics of bone restoration in the area of the removed tissue).
The cystectomy procedure has no age restrictions. However, each clinical case requires an individual approach and treatment. Your attending physician will tell you in more detail about how the operation is performed, what treatment is needed during the rehabilitation period and other nuances during your consultation.
On a note. For several days after the cystectomy operation, pain (from nagging to moderately acute) and slight swelling of the tissue may be observed in the intervention area. Don't be afraid of this. If swelling and pain are accompanied by an increase in body temperature for 3 or more days, you should consult a doctor.
Quality criteria for dental cyst removal
Despite the fact that cystectomy is a surgical intervention, the main indicator of the quality of treatment will be the sanitation of the root canals, including retrograde filling. Currently, in addition to eliminating the cyst shell itself, the unspoken rule has become the filling of its cavity with one or another osteoplastic materials, because this completely eliminates the possibility of blood clot suppuration, promotes rapid healing of the bone defect and improves the mechanical stability of the tooth.
More about the operation
Cystectomy is an organ-saving operation that involves complete excision of an ovarian cyst without damaging healthy tissue.
Despite its benign nature, even a small cystic formation can lead to the development of serious complications - dysfunction of the ovaries and menstrual cycle, adhesive disease, infertility. The intervention can be performed as planned or emergency. The second option is used in the development of emergency conditions - rupture of the cyst, torsion of its stem and some other indications. Cystectomy of the cyst is performed laparoscopically, through several micropunctures in the abdominal cavity. The main advantage of this approach is minimal blood loss, low risk of complications and rapid recovery after surgery.
Indications for tooth extraction with a cyst
As a rule, conservative treatment carried out on time or surgery to remove the cyst allows you to save the tooth. But this is not always possible. A tooth must be removed in the following cases:
— the presence of severe pain symptoms when drug treatment is ineffective; - purulent inflammatory process when it is impossible to drain it; — fracture of the coronal part of the tooth, without the possibility of restoration with anchor pins and/or stump inlays; — obstruction of root canals; — the presence of multiple damage to the roots of the tooth or large damage; the tooth is almost completely destroyed and orthopedic restoration is impossible; - no need for dental treatment due to the presence of a prosthetic plan agreed upon between the doctor and the patient.
Carrying out laparoscopy
Access to the body cavity during laparoscopy is provided through several small holes in the peritoneum. The ovary or its ligament is grabbed with a soft clamp and rigidly fixed. Tissue coagulation is performed over the cyst. An incision is made along the perimeter of the formation, spreading the edges of the wound to the sides.
After enucleation, the doctor examines the place where the tumor was. Bleeding tissue is cauterized. Large cysts are usually opened during removal, so during laparoscopy special tools are used: needles and aspirators-irrigators. The resulting liquid is sent for cytology. Next, the ovary is freed from adhesions, and the edges of the incisions are precisely aligned. Sometimes there is a need for endosurgical sutures.
After the operation, the patient remains in the clinic for 4-5 days, the risk of complications is greatest in the first two days. At first there is pain in the pelvic area. After discharge, physical activity and sexual intercourse are not recommended for about a month, but mobility cannot be completely limited.
It takes about three months for a woman’s body to fully recover after removal of an ovarian cyst. If the rehabilitation period proceeds normally, the doctor allows pregnancy planning. The probability of a successful pregnancy after cystectomy is 85%.
Price
The cost of treatment or removal of a dental cyst consists, like many other surgical interventions, of a number of factors. The complex of diagnostic procedures performed, types and methods of treatment, conservative preparation of canals, preoperative preparation, the operation itself, the osteoplastic materials used, postoperative observation - all this affects the final cost of treatment in these clinical situations.
A dental cyst is a serious pathology. In all cases, even in cases of complete absence of any symptoms, it poses a health hazard. With regular visits to the dentist, you can be sure: a dental cyst, if there is one, will be detected in time, and subsequent treatment will allow it to be eliminated without leaving a trace, preserving the health of the tooth.
According to antiplagiat.ru, the uniqueness of the text as of October 16, 2018 is 99.9%.
Key words, tags: X-rays, tooth extraction, orthopantomogram, periodontitis
Introduction
Open radical cystectomy (RC) has long remained the mainstay of treatment for patients with muscle-invasive bladder cancer (BCC) 1 - 3. It is also indicated for recurrent superficial tumors with a high risk of progression, BCG-resistant carcinoma in situ, T1G3 1. The active development of medical technologies has led to the evolution
of minimally invasive operations in the treatment of bladder cancer. Over the past decades, laparoscopic and robot-assisted RC have been actively introduced. There are publications in the literature about their effectiveness and relative safety with superior results in terms of blood loss, early recovery of intestinal function, hospitalization and rehabilitation time 4 - 9.
Robot-assisted surgery has gained widespread development in urology, mainly due to the frequently performed radical prostatectomies. Over the past decade, robot-assisted access to RC has begun to be used. Until 2010, the number of centers performing this operation was limited. In recent years, the number of publications has increased, including large series, reflecting the growing acceptance of this approach for RC 7 - 8, 10 - 11. However, RC with urinary diversion remains one of the challenging operations in urology. It is associated with a high complication rate even in the hands of an experienced surgical team. As shown by some authors, their number decreases with experience, although they remain high even in specialized urological centers 5, 10 - 12. The operating time for robot-assisted RC, compared with open access, remains quite long. With the accumulation of experience, it is possible to reduce the duration of the intervention by optimizing the methodology for performing individual stages of RC, among which are cystprostatectomy with pelvic lymph node dissection (stage I) and intestinal diversion of urine (stage II). In this article, we present the stages of robot-assisted RC, additionally describing the technique of nerve-sparing RC in men and organ-sparing surgery in women.