Quick transition Treatment of epiglottitis
Epiglottitis is an acute inflammatory disease of the epiglottis and adjacent structures that can lead to life-threatening airway obstruction.
In the case of the infectious nature of the disease, inflammation occurs as a result of bacteremia and/or direct invasion of the microorganism into the mucous membrane of the epiglottis.
As a result of swelling and accumulation of inflammatory cells between the epithelial layer and the cartilage of the epiglottis, the latter increases in size. The swelling progresses rapidly and covers the entire vestibule of the larynx (the area of the larynx below the vocal folds is usually not affected), the airways narrow down to complete obstruction, leading to cardiac arrest and death.
Effective rinsing solutions
• Water with salt, soda.
Dilute 1 teaspoon of salt and soda in a glass of water. You can add a little iodine there, which will have a disinfecting effect. • A solution of chlorhexedine, which has antiviral and antimicrobial activity. It fights well against pharyngitis, streptococcal, and staphylococcal infections.
• Chlorophyllipt is a green alcohol solution for getting rid of staphylococcal and viral infections. They are also good for treating laryngitis, pharyngitis, and sore throat.
• Propolis – helps in case of bacterial sore throat. Drops of propolis tincture are dissolved in 100 ml of water (you can buy it at the pharmacy).
• Medicinal herbs that have bactericidal and anti-inflammatory effects. These include: St. John's wort, calendula, chamomile, eucalyptus, oregano, raspberry leaves, sage. You can use these herbs individually or as a whole collection.
Remember, dear friends. Self-medication for such diseases is unacceptable. Every pimple on the mucous membrane of the throat requires treatment by a professional who can accurately determine the cause of its appearance and prescribe the correct therapy. Be healthy!
Children get sick often, and this is largely due to imperfect personal hygiene, close contact with other children or adults who are sources of infection, as well as the immaturity of the immune system, as a result of which the body becomes susceptible to viruses and bacteria. Redness of the mucous membrane of the pharynx and tonsils is a persistent sign by which a person examining the throat of a sick child can judge the presence and severity of the inflammatory process. Often, parents and practicing pediatricians are faced with cases of classic pharyngitis and tonsillitis, but if the pimples in the child’s throat have a reddish tint, the approach to diagnosis will be different.
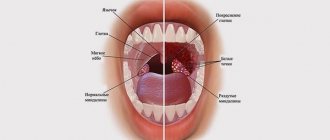
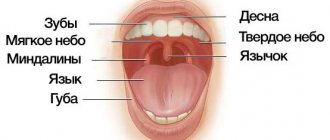
Throat diseases are a broad concept, since it includes a whole group of heterogeneous pathologies that can be caused by both viruses and bacteria, and pathogenic fungi (mycoses). The “throat” in the generally accepted sense includes the pharynx, lymphoid formations - the tonsils, and sometimes the larynx, located next to the pharynx. Since during a visual examination without special devices one can see mainly the back wall of the pharynx and the palatine tonsils, complaints about rashes are usually explained by damage to these anatomical areas.
A rash in the throat in children is a symptom that can only be called relatively specific. Rashes such as spots, nodules or blisters (vesicles) are not characteristic of the typical form of pharyngitis or tonsillitis (sore throat), and these diseases are the most common. Damage to the mucous membrane, accompanied by the appearance of vesicles, is observed during infection with herpes group viruses, enteroviruses that cause:
- herpangina;
- chicken pox;
- herpetic stomatitis.
Pimples in the throat are usually explained by an infectious process.
However, at the same time, other changes that are present in banal (simple, classical) forms of inflammatory processes can be mistaken for a rash. The diseases named in the list are characterized by a blistering rash, often with clear or cloudy exudate, rather than elements resembling pimples or pimples. Therefore, diagnosis should be carried out by a specialist familiar with the features of changes in the mucous membrane of the oropharynx in various pathologies.
It is also necessary to distinguish between infectious and inflammatory pathologies that occur acutely or chronically, provoked by viral or microbial agents. For example, white bumps in the throat may indicate a bacterial throat infection called bacterial pharyngitis. The etiology of the disease during the infectious process determines the choice of treatment, so timely and high-quality diagnosis is necessary for successful recovery.
Why might red formations resembling pimples appear in a child’s throat? This occurs as a result of the development:
- Acute infectious pharyngitis.
- Chronic hypertrophic pharyngitis.
These diseases are caused by an inflammatory process within the boundaries of the pharynx and are most often caused by respiratory viruses or bacteria (streptococci, staphylococci). We cannot exclude the possibility of simultaneous damage to the tonsils (tonsillopharyngitis), which is often observed in children, especially in the younger age group.
Red back of the throat: causes and treatment
Many people are accustomed to considering redness in the throat as the first symptom of a cold, is this true? What to do if the back of the throat is red, it becomes difficult to swallow and there is a tickle when speaking? Can use traditional methods or give preference to drug therapy.
Reasons for violation
Banal hypothermia and cold air can cause the appearance of a red throat. Also eating excessively cold, hot or spicy foods. Allergic reactions to external irritants.
A dry microclimate in the room, swallowing snow in winter (applies to children), and eating solid foods that can scratch the mucous membrane and provoke an inflammatory process can cause tickling and coughing.
The following may contribute to the development of such symptoms:
- viruses that cause pharyngitis in 70% of cases, this will indicate the initial stage of development of the disease;
- bacteria, when streptococci, Haemophilus influenzae, mycoplasma penetrate the body, while the microflora in the nasopharynx, where pathogenic microorganisms live, is disrupted;
- Candida fungus, cause a chronic stage of the disease in children with weakened immune systems.
Why does a child's throat turn red?
A red back wall of a child’s throat indicates an inflammatory process, especially if the baby has difficulty swallowing and has a sore throat. In this case, you need to approach the healing of the body fully, using antiviral, antibacterial, and immunomodulatory agents.
If there are also red pimples on the back of the throat, this indicates that the inflammation is of a bacterial nature, a rash is formed, white or brown pustules.
Colds and runny nose
Red spots on the back of the throat may indicate the occurrence of mucus, which flows into the throat and causes an inflammatory process. Additionally, the child develops a hoarse voice, cough, and sputum leaving the body.
To stop this process, it is necessary to thoroughly rinse the nasopharynx with a water-salt solution, take cough softeners, followed by expectoration of sputum.
In case of a bacterial runny nose, you need to carry out antibacterial rinsing with Miramistin, inhalation with Decasan or mineral water. With the right approach, this symptom can be completely eliminated in a few days (in the absence of high fever).
An article on the topic - how to rinse with saline solution.
Infections
If your throat hurts and the back wall of your throat is red, then you can safely talk about an infection. It is the mucous membrane of the throat that takes the “blows” of a viral or bacterial attack.
If the infection is viral, then pathogenic bacteria destroy the outer epithelium, creating a favorable environment for microbes to penetrate deep into the tissue, and the integrity of the membrane is compromised.
In this case, the following symptoms are observed:
- the back of the throat turns red and hurts;
- the voice begins to wheeze and “sit down”;
- sudden attacks of dry cough;
- general weakness appears in the body;
- the temperature rises.
Treating viral infections with antibiotics is ineffective; antiviral agents and drugs are needed to maintain the body's immune flora, for example, Interferon. But if pus forms on the back wall of the throat, it is necessary to use antibiotics and perform antimicrobial irrigation with chlorophyllipt.
Tonsils
The tonsils are located in the upper part of the larynx, and antibodies are released through their pores into the pharyngeal mucosa. Inflamed almonds are called adenomas; when they enlarge, nasal breathing becomes more difficult, pimples may appear on the back wall of the throat, and a lingering runny nose appears.
It is recommended to rinse the nasal passages with medicinal decoctions or saline solution; for this purpose, you can use an oil- or water-based inhaler.
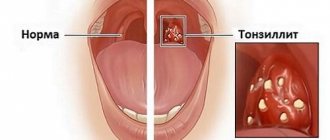
Pharyngitis
If the back wall of the throat is constantly red, then we can talk about pharyngitis - severe inflammation of the mucous membrane, the throat begins to hurt very much, the voice becomes hoarse. In children, this form of the disease occurs as a complication after nasopharyngeal disorders.
Article on the topic - nasopharyngitis in children: treatment.
Teeth cutting
During teething, a slight fever, cough, and runny nose may appear, causing the throat to become redder and salivation to increase. During this period, it is important to prevent the addition of a secondary infection, and therefore you need to actively gargle and rinse your nose with saline solutions.
Allergy
Redness of the throat may be associated with an allergic reaction; to treat this symptom, you need to establish the cause of the deterioration of the baby’s condition, and only then use antihistamines to relieve the symptoms of the disease.
Constantly red throat - how to treat.
How to examine a child's throat for diagnosis
Red back of the throat - how to treat
You can use medications and traditional methods of healing the body. Features of treatment for a child are as follows:
- regular irrigation of the oral and nasal cavities (sprays, rinses), such procedures relieve swelling and reduce inflammation;
- antihistamines are used to reduce swelling in the throat and nasopharynx;
- if the back wall of the throat is red, then treatment can be carried out with iodine-containing agents to disinfect and warm the surface (Lugol);
- choose preparations based on sea salt as an antiseptic;
- various lozenges and lollipops can significantly alleviate the condition and destroy germs, this method is well suited for children, there are different flavors that young patients like;
- high temperature (38 and above) can be brought down with the help of antipyretic medications (Nurofen);
- Additionally, ozonation of the sore throat (UV ray treatment) may be required.
Traditional therapy
If there are red pimples on the back of the throat and the inflammatory process continues, it is important to adjust the baby’s diet, exclude serving hot and cold foods and liquids, and add more plant foods high in vitamins and microelements.
Drinking plenty of fluids is required, the air in the room should be humid, and the temperature should not exceed 24 degrees. Warm baths for hands and feet, mustard plasters on the feet or calves (if there is no fever) will give a good therapeutic effect.
For inhalations, you can use decoctions of eucalyptus, sage, calendula, and chamomile leaves, breathe for several minutes, and perform about 5 such procedures per day.
To irrigate the throat, you can use the following means:
- herbal decoctions based on chamomile, sage, calendula, St. John's wort, eucalyptus;
- honey compotes with dried fruits;
- warm teas with raspberry and currant jam;
- infusion of oak bark, linden flowers, rose hips.
You can make a warm compress on the throat - fold gauze in several layers and soak it in a 40% alcohol solution, apply a bandage to the neck, wrap it with a warm scarf, and leave it overnight.
Only an experienced doctor can choose the right treatment regimen, and self-medication will not lead to good results. Only a rational combination of folk remedies and medications can lead to the desired effect.
Improvement of the nasopharynx
If red bumps appear on the back of the throat, then we may be talking about inflammation of the nasopharynx. Drug therapy for this disorder is aimed at eliminating the pathogen and alleviating the symptoms of the disease.
For proper treatment, it will be necessary to undergo the necessary tests in order to determine the nature of the disease - viral, bacterial, allergic or vasomotor. In most cases, such symptoms indicate the presence of viral nasopharyngitis.
What medications to use
- Antiviral drugs - Ingavirin, Kagocel, Rimantadine.
- For bacterial infections of the nasopharynx - Amoxicillin, Cifran and others.
- For allergic disorders of the mucous membrane of the throat - Diazolin, Suprastin.
- To relieve fever - Rinza, Theraflu, Ibuprofen.
- To rinse the nose and reduce the flow of mucus - Nazivin, Pinosol.
The patient requires bed rest, plenty of fluids, and regular ventilation of the room.
If your nose is stuffy, you need to rinse your nose with saline solution, or put a few drops in each nostril until the result improves.
Attention: you should not blow your nose too much, because mucus can get into the ear canal or maxillary sinuses, which can lead to subsequent complications.
You can treat red bumps on the back of the throat by regularly gargling with herbal decoctions of sage, calendula, eucalyptus, chamomile, cooking in a water bath, and performing the procedure 6-8 times a day.
How not to harm a child with pharyngitis?
If the back wall of the throat is red and a high temperature is observed, then various thermal procedures are prohibited; a small patient should not be given too many pathogenic teas and infusions, so as not to provoke dehydration of the body.
It is also not recommended to use vinegar and alcohol rubdowns, which may cause vascular spasms. In case of acute or chronic pharyngitis, a child should not consume hot, spicy, sour, cold and spicy foods; dishes and drinks should be at room temperature.
Hospitalization may be required in the following cases:
- red bumps on the back of the throat;
- purulent inflammation of the throat and nasopharynx;
- prolonged maintenance of temperature, difficulty in controlling the course of the disease;
- the occurrence of scarlet fever, diphtheria as a secondary infection.
Treatment of the chronic form in case of mucosal atrophy
To treat the inflamed mucous membrane of the throat and nasopharynx, inhalation with essential oils is indicated; they help prevent the membrane from drying out. To improve the patient’s health, you can use various oils (sea buckthorn, olive, peach), add a few drops to a glass of boiling water and breathe for 5-7 minutes.
You can do soda inhalations, pour one spoonful with a glass of boiling water and carry out the procedure several times a day. Steam inhalation of potatoes and onion infusion is effective.
It is useful to prepare a composition from raspberry leaves, St. John's wort, mint, nettle, add propolis alcohol tincture to the finished composition, take 2 spoons several times a day before meals.
Infusions of blueberries, currants, and raspberries will help you cope with pharyngitis; gargle or add to warm tea, drink 3-4 times a day. Additionally, take medications prescribed by your doctor.
How to treat pharyngitis
Red throat in infants - treatment with folk remedies
The following folk methods for sore throat in infants have proven their effectiveness:
- Apply compresses from decoctions of chamomile, eucalyptus and calendula for a maximum of 30-40 minutes.
- Compress with low-fat cottage cheese, place the warm mass on the neck, hold for several hours, repeat the procedure.
- Give chamomile tea only after consulting a doctor; you can add a weak decoction of medicinal plants to the feeding mixture.
- You can lubricate the pacifier with a solution of oil chlorophyllipt.
- Bathe your baby in a bath with the addition of eucalyptus decoction (has bactericidal and immunomodulatory properties).
- Place peeled garlic cloves or onion slices in the child’s bedroom and carefully monitor the humidity in the room.
To irrigate the throat, you can prepare the following composition: take aloe leaves, rinse in boiled water, chop, grind in a meat grinder, mix the resulting juice with water. Rinse your throat with this product; use a pipette or an inhaler spray for irrigation. You can lubricate the nipple before feeding.
Article on the topic - how to use aloe juice for treatment.
Preventive actions
To avoid redness of the throat and accompanying symptoms of a child’s well-being, it is necessary to correctly carry out prevention:
- hardening the body in order to adapt the body to sudden changes in temperature; you can begin to carry out such procedures from early childhood;
- regular house cleaning, moderate humidity, clean air;
- sanitary and hygienic standards, after each visit to the street, wash your hands with soap and wash, clearing the nasopharynx of bacteria;
- in the cold season, you need to keep your feet warm, wear woolen socks, and choose shoes from natural materials, to prevent hypothermia of your extremities;
- regular recreation in nature, in the forest, in order to saturate the lungs with clean air;
- good nutrition;
- morning exercises;
- consuming vitamins and minerals to strengthen the immune system;
- You can get a flu shot to protect yourself from viral diseases by 80%.
Now you know what to do if the back of the throat is red and the child’s condition requires immediate recovery. It is important to follow preventive measures and not to start the disease.
Attention, TODAY only!
Source: //LOR-explorer.com/lechenie-gorla/krasnaya-zadnyaya-stenka-gorla-prichiny-i-lechenie
Scarlet fever
The causative agent of this infectious disease is hemolytic streptococcus, which causes inflammation of the oral mucosa. Infection occurs 2–3 days after contact with a patient with tonsillitis, pharyngitis, or a carrier of the bacteria.
The first signs of scarlet fever are fever and sore throat. The next day, a rash appears on the cheeks, folds of the arms and legs, and sides of the body. A feature of the skin lesion is a white nasolabial triangle, untouched by the rash.
A characteristic sign of infection is the appearance of pimples on the back of the throat in the form of a red, pinpoint rash.
Note! On the second or fourth day of illness, the patient’s tongue becomes “crimson.” Its papillae enlarge and become bright red, giving the tongue a grainy appearance.
The tonsils are inflamed, covered with purulent plaque, and painful when swallowing.
The main treatment for scarlet fever is antibiotics - Amoxiclav, Phenoxymethylpenicillin, Ampicillin for 7-10 days. The infection is usually mild. But rapid improvement is not a reason to discontinue the drug.
Streptococcus is destroyed in the body only with a full course of treatment. Otherwise, the patient will be its carrier, posing a danger to the family. Additionally, B vitamins and ascorbic acid are prescribed.
The most common cause of candidiasis is decreased immunity. Therefore, thrush often occurs in the mouth of infants. Thrush is characterized by pimples in the throat, covered with a white cheesy coating. The spots are localized on the tongue, behind the arches, tonsils and soft palate.
Important symptom! After removing the top layer, small erosions are visible, from which droplets of blood are released. The rashes cause discomfort to patients.
- pain and dryness in the throat;
- itching and burning;
- tonsil hypertrophy;
- redness of the throat;
- elevated temperature is observed mainly in children;
- decreased appetite.
Untreated thrush becomes more complicated. Ulcers appear in the mouth and fester. The infection spreads to the larynx. Yeast-like fungi Candida are able to penetrate the digestive system.
With the bloodstream they can spread throughout the body, leading a person to sepsis with a fatal outcome.
During treatment, systemic antifungal drugs are prescribed - Fluconazole, Mycostatin, Fucis, Itraconazole. Medicines are prescribed in courses. The doctor selects medications based on the results of the smear, taking into account the severity of the infection.
Gargles with boric acid and oak infusion are prescribed. The oral cavity is lubricated with Lugol's solution, Fukortsin, sea buckthorn oil and antifungal creams. Ultraviolet and laser rays are used in complex treatment.
The causative agent of stomatitis is the herpes virus, which often infects children under 3 years of age. Inflammation of the mucous membrane occurs with sore throat while eating. Signs of stomatitis;
- hyperemia of the pharyngeal walls;
- spots that differ in color and shape, covered with a yellowish coating;
- ulcers appear on the inner walls of the cheeks, gums and back wall of the larynx, surrounded by a halo;
- formation of “jammed” cracks in the corners of the mouth.
Antiviral drugs are used to treat stomatitis. Both special agents and herbal preparations are used as immunostimulants - Chinese lemongrass, Echinacea.
Sebidin, Septolete, Faringosept relieve throat pain. For oral candidiasis, an effective Candida solution is widely used.
In addition to special therapy prescribed by a doctor for each disease, traditional methods of treatment are used.
The following products are recommended for mouth rinsing for candidiasis:
- juice of aloe or related Kalanchoe, diluted with water;
- soda or saline solution in a proportion of 1 tsp. for 200 ml of boiled water;
- infusion of a mixture of dried herbs - chamomile, mint and eucalyptus. To prepare the solution in a water bath, take 1 tbsp. l. dry collection in a glass of boiled water, infuse for 15 minutes;
- After rinsing, doctors advise dissolving a spoonful of honey in your mouth.
To strengthen the local immunity of the oral mucosa, herbal teas with lemon, honey, linden, and raspberries are useful. It is useful to take a drink made from rose hips.
For sore throat, beet juice relieves sore throat. Propolis helps, which is usually chewed several times a day. Gargling with infusions of chamomile, eucalyptus, and sage is widely used.
Pimples in the throat - which may indicate diseases
It is not uncommon for the first, inconspicuous symptoms to appear before the onset of the disease itself. The body warns and makes it clear that a new problem has arisen. The body's natural signals should not be ignored. It would be best to undergo a thorough examination to eliminate anxiety. Preventive measures to maintain health will not hurt.
Briefly about pimples in the throat
The occurrence of inflammation on any part of the body signals the appearance and presence of a disease. Pimples in the throat were no exception, as were pimples on the gums.
Occurs with various types of infectious diseases. The disease may not manifest itself. The first signals may be formations that appear in the oral cavity, in the larynx, and on the tonsils.
People often warn about diseases associated with inflammation of the throat.
It is worth paying attention to the inflammatory processes occurring in the middle. You need to go see a doctor and take the necessary tests. It is possible to prevent the disease before the onset of characteristic symptoms.
Recovery will take place before the onset of illness. A person will not experience unpleasant symptoms that bring discomfort, pain, or complete exhaustion of the body.
A disease noticed in time is half the recovery.
Emerging diseases
Pimples in the throat can be the first sign of the occurrence of such diseases:
- tonsillitis;
- scarlet fever;
- bacterial pharyngitis;
- candidiasis;
- stomatitis.
The above diseases pose a serious threat to the human body. Incorrect treatment and lack of medication lead to death. You need to immediately pay attention to education.
Angina
Sore throat (acute tonsillitis) is determined when plaque appears on the tonsils. Characterized by fever, acute pain in the tonsils. The appearance of plaque is a distinctive feature of the disease.
There are different types of sore throat. The complexity of treatment depends on the type. Inflammation that occurs in the tonsils prevents you from breathing, drinking, or eating calmly.
Acute pain that occurs upon any contact with food or water brings painful sensations.
Most often, catarrhal tonsillitis develops. The patient complains of pain in the tonsils, severe burning, dry mouth, and fever. The plaque on the tonsils is not very large. Treatment is carried out for two weeks with antibiotics, sometimes a drip is prescribed in case of elevated temperature.
Follicular tonsillitis may appear, characterized by an increase in body temperature to thirty-nine degrees Celsius. The pain when swallowing becomes more acute. It often goes into the ear. Due to an infectious inflammatory process, partial hearing loss begins. Lymph nodes double in size. Fever causes body aches.
The lacunar type has similar symptoms to the follicular type. It comes with complications. White pimples turn yellow due to the large amount of pus.
The fibrinous type is characterized by the elimination of acne and the flow of pus. An inflammatory process occurs. A yellow plaque settles in the tonsils, exposing the body to infection. My throat starts to hurt. Plaque gives rise to a strong inflammatory process. Fever is an integral feature of the disease.
Scarlet fever
Scarlet fever is an infectious disease. They warn about the occurrence of pimples on the throat. When they occur, a white coating appears on the tongue. Scarlet fever can be contracted from someone with tonsillitis. A person is dangerous in the first days of illness. It is worth limiting contact with a healthy person who has recovered from the disease.
Can be a carrier for a month. You can get infected from a healthy person. A certain percentage of people have scarlet fever. The disease develops without symptoms and does not cause discomfort to the carrier. Bacteria can be released when you sneeze or cough.
It is worth regularly (twice a year) to take a culture test for the presence of streptococcus bacteria.
pimples around the mouth
Bacterial pharyngitis
Occurs at the end of winter, beginning of autumn. The period is characterized by a weakening of the immune system. The body is exposed to a variety of viruses. Pharyngitis is characterized by inflammation of the mucous membrane of the throat, enlargement of the lymph nodes, causing pain. Pimples on the throat can signal the appearance.
The cause may be polluted, hot air inhaled daily. Irritation of the mucous membrane occurs. The result is pharyngitis. The nasopharynx is often affected. The disease is accompanied by a runny nose, which does not go away for a long time, transforming into rhinitis, sinusitis. Disease of the tonsils, ears, nose are interconnected. Problems arise for one, and another begins to get sick. Logical pattern.
Candidiasis
Candidiasis is a fungal infection that affects not only the larynx, but the body as a whole (detailed material). Affects the oral cavity. A characteristic feature is a white tongue. It can manifest itself for a variety of reasons.
Common – abuse of antiseptics, lack of vitamins, overdose of antibiotics. These products kill beneficial bacteria in the body. Provoke fungus to grow.
Contains the necessary enzymes for the development of fungal disease.
At the initial stage, symptoms are not noticeable. Sometimes dry mouth appears and the temperature rises slightly. Weakness and malaise occur. Less often - sore mouth.
The symptoms are similar to normal respiratory inflammation. Almost no one goes to the doctor with such a diagnosis, considering it a trifle. Symptoms can be aggravated by eating sour, hot foods.
The mucous membrane of the throat becomes more irritated. A real illness is emerging.
The advanced form has pronounced purulent discharge. Pimples on the back of the throat are characteristic manifestations of candidiasis. The disease may appear in the form of grains.
The formations will stand out clearly, having a bright red color. It can be seen especially clearly when coughing or observing the throat under a light. By visiting a doctor quickly, without preliminary tests, you can find out the result of the examination.
After passing the necessary tests, confirm the result.
Stomatitis
Affects the oral mucosa. It appears as white wounds. On contact it causes pain and burning. Occurs due to mechanical damage and dysfunction of the body. It can be a burn caused by eating sour or hot foods. Signals about health problems.
Most often occurs due to swelling of the lymph nodes. Characterized by bad breath, bleeding gums, and a pimple in the throat. In advanced cases, plaque can form on the tongue. Manifestation of stomach problems.
Ulcerative formations appear on the inside of the cheeks and lips. Contact with salty, sour foods causes severe pain. The formation is covered with a white, protective film.
It goes away after eliminating the problem with nutrition and putting the natural metabolism in order.
Troubleshooting
A white pimple that appears on the tonsil requires immediate diagnosis and clarification of the cause of its appearance. Do not ignore the problem that has arisen. You need to go to the doctor and get the necessary tests. Diseases that prevent rashes fit into the classification of unpleasant and difficult to treat.
Each type is treated differently. They have a common feature of elimination - do not drink hot drinks, do not breathe dusty air, do not take hot or cold baths. Hot water and tea provoke the rapid development of the inflammatory process.
Burning water creates burns on the damaged shell. The pain gets worse. Purulent discharge is profuse. It is recommended to take drinks and a bath at room temperature. Eliminate sour, salty, and sweet foods from your diet.
The strong taste irritates the mucous membranes, leading to complications.
Treatment occurs in stages. First you need to remove the source of pain and inflammation. In addition to preventive methods, mouth rinsing can be used. Dilute a tablespoon of soda and two drops of iodine with warm water. Gargle three times a day.
Do not swallow the prepared solution under any circumstances. Damage the digestive passage, stomach. Burns may occur, causing ulcers. After three days of active rinsing, the purulent plaque will gradually decrease, and the pain in the tonsil area will become barely noticeable.
After eliminating pain, you should begin drug treatment. Will consist of antibiotics. Penicillin antibiotics are often prescribed. People who have an allergic reaction to a type of drug should not use the product.
The doctor is obliged to prescribe a medicine that is not harmful to health. When eliminating a white pimple, remember that treatment must be comprehensive and support the components of the body. In addition to drug treatment, you should take a course of vitamins.
The body will be saturated with useful substances, the immune system will become stronger, and recovery will proceed at a rapid pace.
If you notice a pimple on the tonsil, do not try to get it out or remove it yourself. It can lead to infection of the body and the onset of illness. First, a doctor must examine you, render his verdict, and prescribe medications. With the help of medications and rinses, you can get rid of formations in the oral cavity.
Many people, seeing formations in the tonsil area, naturally ask: what is it? The undisguised interest can be explained by concern for health. A trip to the doctor, a well-written article on the Internet can explain what it is and suggest a solution to the problem.
Doctors warn! Shocking statistics - it has been established that more than 74% of skin diseases are a sign of parasite infection (Accarida, Giardia, Toxocara).
Worms cause enormous harm to the body, and the first to suffer is our immune system, which should protect the body from various diseases.
The head of the Institute of Parasitology shared the secret of how to quickly get rid of them and cleanse your skin, it turns out that it’s enough... Read more...
(1 5,00 of 5) Loading...
Source: //boleznikogi.com/pryshhiki-v-gorle-kakie-mogut-signalizirovat-zabolevaniya
Treatment
The method of treatment is chosen by the doctor individually, depending on the disease:
- Sore throat that occurs without fever and chronic tonsillitis require treatment with drugs aimed at combating streptococcus - these are broad-spectrum antibiotics. In parallel with this, it is necessary to rinse the tonsils from plaque and plugs with pus. The procedure is performed in medical institutions. You can do without it, but the recovery process in this case will be delayed.
- Rinsing is an excellent remedy for plaque, purulent formations and inflammation, relieving pain and discomfort. The procedure can be carried out with soda and salt, or with antiseptic drugs (miramistin, furatsilin). If the child is still too small and does not know how to gargle, then the procedure can be replaced by irrigation with the same compounds. Rinsing should take at least 5 minutes, otherwise it will have no effect. It is better to irrigate the oral cavity 6-7 times a day, after which you should not eat food for 30-40 minutes.
- In case of thrush, plaque is removed with a soda solution, but antifungal drugs are more often prescribed. It is not easy for children to cope with thrush - a fragile immune system is not able to quickly overcome fungi, so serious systematic treatment is required and compliance with all doctor’s recommendations.
In addition to drug therapy and procedures, it is important to adhere to a number of rules in order to get rid of an unpleasant disease as soon as possible:
- give up solid and irritating foods, giving preference to soft cereals, jelly, lean broths, purees, etc.;
- Likewise, you should refrain from eating cold and hot food;
- do not apply warm compresses to the throat - heat promotes the growth of bacteria;
- Drinking plenty of fluids will help quickly remove the infection from the body and improve the condition of the tonsils.
Acne therapy
Pharyngitis caused by bacteria and other pathogens responds well to treatment with antibacterial drugs. Granular chronic pharyngitis, manifested by pimples in the throat, requires an integrated approach to treatment:
- antibacterial drugs;
- immunostimulants;
- physiotherapy.
For abscesses, surgical intervention is used. After removal of the abscess, the patient is prescribed detoxification agents and antibiotics.
If candidiasis bacteria are detected, treatment is carried out with antifungal drugs. The Candide solution has proven itself well, with which you need to wipe your tongue by dipping a cotton swab into it. During the treatment period, the patient is advised to remain in bed, drink more warm liquids and adhere to a balanced diet.
In addition to taking medications, doctors also prescribe gargling with iodine, sea salt or soda. To achieve maximum effect and relieve inflammation, you should gargle at least 10 times a day. When the inflammation begins to subside, you need to use calendula flowers for rinsing.
A solution of furatsilin and streptocide have also proven themselves well. Thanks to their antiseptic effect, these drugs will quickly relieve inflammation and relieve other symptoms of the disease. However, you should not stop rinsing after a slight improvement; doctors strongly recommend rinsing until all symptoms of the disease completely disappear.
Aids
To cleanse the throat mucosa, doctors prescribe the drug Lugol. However, it contains iodine, so it is better for allergy sufferers to refrain from using it.
White pimples in the throat, which are caused by sore throat or tonsillitis, require complex treatment. In this case, patients are prescribed hyposensitizing and anti-inflammatory drugs, as well as a complex of vitamins.
Physiotherapeutic procedures, as well as ultraviolet and laser treatments have found wide application in the fight against viral and colds. In case of acne recurrence, surgical intervention is indicated. Today's medicine performs such operations using laser surgery.
To eliminate pimples in the throat that are caused by a viral infection, antiviral drugs, such as Acyclovir, are prescribed, as well as vitamins and minerals to stimulate the immune system.
Pimples in the throat are a temporary phenomenon, but they can significantly worsen a person’s general condition. Therefore, it is extremely undesirable to ignore this symptom, especially if it is accompanied by other signs of a cold. Self-medication is also unsafe. Only visiting a doctor and following all his prescriptions will help you quickly get rid of the unpleasant symptom.
Treatment methods for white pimples in the throat in children
Child examination
The doctor will determine the cause of the appearance of white bubbles or pimples in the child’s throat through tests, throat swabs and visual examination of the throat. Treatment is prescribed on an individual basis and depends on the cause of the pathology.
Treatment of candidal stomatitis
For candidal stomatitis, a soda solution helps a lot. Gauze is wrapped around the finger, moistened in a soda solution (preparation instructions: 1 teaspoon of soda per glass of boiled water) and the mucous membranes of the oropharynx affected by white pimples are carefully treated.
Preparation of soda solution
Infants should be put to the breast more often, and babies who are already receiving complementary foods should be given boiled water to drink after each meal. In case of severe damage and severe course of candidal stomatitis, the doctor selects an antifungal agent for the child in its age-appropriate dosage.
Children who eat from a common table must limit fast carbohydrates in their diet:
- White bread;
- candies;
- chocolate;
- cocoa;
- baked goods;
- cookie;
- sugar.
Treatment of sore throat
White pimples in the throat with a sore throat most often indicate damage to the mucous membranes by staphylococci. Treatment in this case is necessarily comprehensive.
Depending on the age and characteristics of the child’s body, the doctor prescribes:
- antibiotics to which the pathogen is sensitive (this is determined in the laboratory after inoculating smears from the oropharynx on a nutrient medium);
- aerosols and sprays with local analgesic and anti-inflammatory effects;
- rinsing solutions (you can prepare them yourself at home or purchase ready-made ones at the pharmacy);
- dissolving tablets with antiseptics.
For small children under 4-5 years old, the doctor selects antibiotics in the form of a suspension. The drugs in this dosage form come with a syringe or measuring spoon, with which you can easily measure a single dose of the medicine.
Abscess treatment
A pimple in the throat of a child, which rapidly progresses in growth and is accompanied by signs of intoxication of the body, in most cases is a retropharyngeal abscess. The lesion most often occurs on one side of the pharynx (right or left) and develops against the background of untreated pharyngitis, tonsillitis, or tonsillitis.
Treatment of a child's throat
In pediatric practice, a retropharyngeal abscess is treated surgically; doctors do not wait until the abscess opens on its own, as this entails additional complications in the form of inflammation of the digestive tract, lymphadenitis, and sepsis.
After surgical opening of the abscess, the child must be prescribed conservative treatment, which includes:
- antibiotics;
- gargling with antiseptic solutions, for example Furacilin (the price of tablets in the pharmacy is lower than the cost of the finished solution);
- treatment of the pharynx with aerosols and sprays that contain an antiseptic or antibiotic.
The video in this article explains where pimples in the throat come from, what causes the growths, and what measures should be taken to prevent the development of the pathological process. Please remember that this video is for informational purposes only and cannot replace the advice of a qualified specialist.
Pimples that appear suddenly in the throat often cause severe discomfort.
Small red sores or purulent rashes interfere with the enjoyment of food, cause pain, and sometimes bleed.
According to medical professionals, a rash on the tongue, inside the cheeks and on the back of the throat is always a symptom of an infectious disease.
- All information on the site is for informational purposes only and is NOT a guide to action!
- Only a DOCTOR can give you an ACCURATE DIAGNOSIS!
- We kindly ask you NOT to self-medicate, but to make an appointment with a specialist!
- Health to you and your loved ones!
The disease can be viral, bacterial or fungal in nature.
But mechanical damage to the mucous membrane is also possible.
It’s a good idea to learn to understand the signs of the most common infections yourself.
This will help avoid unnecessary worries in non-dangerous cases or unforeseen complications in a serious illness.
Traditional methods of treatment
Traditional medicine recipes have always been and remain an effective method of combating viral and colds, including pimples in the throat.
At the first signs of illness, you can prepare a solution for gargling at home. To do this you will need a teaspoon of butter, ½ teaspoon of soda and the same amount of ginger powder. Mix all ingredients with boiled milk (100 ml). Rinse your throat well and then eat a tablespoon of honey. At the same time, you should not immediately swallow honey; you need to keep it in your mouth for as long as possible.
Lemon
Lemon is a good remedy for strengthening the immune system, which is actively used for colds. The simplest and most effective remedy is lemon tea. But not everyone knows that the vitamin C contained in lemon is destroyed under the influence of high temperatures, so it is important to throw the lemon into warm, not hot water.
It is also useful to pour warm (not hot) boiled water over the raspberries and let them brew for a while. Such teas and infusions can be drunk in any quantity; they remove toxins from the body well.
Tea mushroom
Kombucha is a good remedy for relieving pain due to inflammatory processes. You should gargle with the kombucha solution throughout the day. After rinsing, a noticeable improvement occurs already on the 3rd day. The only drawback of this method is the unavailability of kombucha. In this case, it can be replaced with slightly acidified beet juice.
Inhalations
For colds and viral diseases, inhalations of medicinal mint and chamomile help well. 1 tablespoon of herbs is poured with boiled water. To obtain the maximum effect, inhalations must be carried out at least 5 times a day, lasting 20 minutes. For complete recovery, inhalations of the throat and nose are indicated. It is also recommended to use additional treatment methods:
- mustard plasters;
- holding your feet above the steam;
- foot baths.
It must be remembered that the use of all these procedures must be agreed with a doctor; starting treatment on your own is dangerous, because at a temperature, for example, it is strictly forbidden to carry out inhalations and steam your feet.
Yoga
This method of treatment will not be understandable to everyone, but those who have encountered yoga in their lives should know about a healing remedy for colds, which is called “lion pose.” This exercise helps blood flow to the throat, causing inflammation and pain to disappear. Bubbles in the throat, if any, will also disappear quickly.
This exercise is done like this:
- the patient should sit comfortably;
- lean your elbows on the back of a chair;
- open your mouth wide;
- try to stick your tongue out as far as possible.
At the same time, the neck muscles are maximally tense. To do this correctly, you need to imagine a lion that spreads its fingers, bends its paws at the elbows and opens its eyes wide. Here it is important to portray the same aggression, as a result of which the patient will feel an incredible surge of strength. It is recommended to stay in this position longer; for maximum results, it must be performed at least 7 times a day. Moreover, it does not require excessive effort.
Treatment
Before starting therapy, it is imperative to exclude the bacterial origin of the plaque.
The fact is that viral infections that can give such a symptom do not require special treatment. It is enough to give the child more to drink, gargle with saline solution, and drop the same solution into the nose more often (ideally every 15-20 minutes).
For medications, if you really want to buy something at the pharmacy, you can take vitamins and saline solution to rinse the nasopharynx. Antiviral agents, immunomodulators and immunostimulants have no proven effectiveness.
Antibiotics are contraindicated because they increase the risk of a secondary infection, which will also be resistant to antibacterial drugs.
In case of bacterial infection (staphylococcal tonsillitis, for example), it is important to show the child to the doctor in time to prescribe antibiotics. Rinsing will not bring much benefit, but if you really want to, you can use a furatsilin solution
In rare cases, when the infection is very severe, the white plaque is removed mechanically. But you shouldn’t do this at home; usually such manipulation takes place in a hospital or clinic.
Separately, it is worth mentioning such products as Lugol’s solution, alcohol, etc.
The mucous membranes will be able to recover faster if they are sufficiently hydrated.
Alcohol solutions, which some recommend using in combination with water for rinsing, can lead to only one result - additional drying, which means that the likelihood of complications will increase and recovery will slow down significantly.
Lugol's solution is an iodine-based preparation. Not recommended for children due to easy absorption of iodine. The fact is that, when it gets on the mucous membranes, especially damaged ones, iodine is quickly absorbed, accumulates in the body and causes an overdose in the child, which in itself is quite dangerous.
You should not inhale if there is a white coating in the throat, because heating only accelerates the rate of reproduction of microbes and fungal pathogens. Warm compresses on the throat are also contraindicated.
Viral diseases
What can cause the formation of red spots in the oropharynx? Theoretically, the cause of the pathological symptom can be any respiratory disease in which the infection is localized in the throat. Viral diseases are extremely rarely limited to damage to the laryngopharynx mucosa, so patients often complain of inflammation of the nasal mucosa and rhinitis.
| Disease | Typical manifestations |
| flu | high fever, chills, headaches, dry mouth, erythematous rash on the walls of the throat, difficulty nasal breathing, muscle weakness |
| herpangina | febrile fever, vesicular rash in the oropharynx, abdominal pain, difficulty swallowing, hypersalivation, fibrous film on the throat mucosa |
| herpetic stomatitis | red throat, pinpoint rashes on the mucous membrane, burning and sore throat, aphthous formations in the mouth, swollen lymph nodes, painful swallowing |
| measles | high fever, hoarseness of voice, large red spots on the soft and hard palate, redness of the conjunctiva of the eyes, sneezing and photophobia |
| rubella | macular rash on the body, headaches, inflammation of the throat mucosa, red dots on the palatine arches and the back of the pharynx, cervical adenopathy |
| Infectious mononucleosis | fever, inflammation of the pharynx, swollen lymph nodes, pain when swallowing, red rashes in the oropharynx, weakness, migraine, high fever |
| viral pharyngitis | soreness in the laryngopharynx, dry cough, low-grade fever, difficulty breathing, small vesicles on the palatine arches and the back of the pharynx |
It is possible to reliably determine the cause of the appearance of an erythematous rash only after submitting a swab from the throat for virological and microbiological analysis.
Acute pharyngitis
An acute inflammatory process in the mucous membrane of the pharynx is often combined with rhinitis, laryngitis or, as mentioned before, tonsillitis or tonsillitis. However, there are also isolated forms that are associated with infection and exposure to harmful factors (hypothermia, dust, unfavorable living conditions). Acute pharyngitis in children is most often observed as a manifestation of ARVI (acute respiratory viral infection). It is also considered as one of the syndromes associated with scarlet fever or measles.
Children, unlike adults, suffer from acute pharyngitis quite difficult. The disease is characterized by a pronounced intoxication syndrome, severe sore throat and is accompanied by a high risk of infection spreading into the auditory tube (tubo-otitis, eustachitis) and the middle ear (otitis media). Although in more than 70% of cases acute pharyngitis is provoked by viruses that also cause ARVI, one should be wary of infection with beta-hemolytic streptococcus.
Patient complaints
Children who can already formulate complaints usually describe pain when swallowing as the dominant symptom. Pain syndrome is present in all forms of acute pharyngitis, regardless of the type of pathogen. Patients are also concerned about:
- dryness and rawness in the throat;
- stuffy ears, hearing loss;
- weakness, headache.
With concomitant rhinitis, nasal breathing is impaired, causing the mucous membrane of the pharynx to dry out even more, since the child has to breathe through the mouth. Pimples in the throat are usually clearly visible. There may also be coughing, an obsessive cough - dry or with a scanty amount of mucopurulent discharge. Increased body temperature in children usually reaches 38 °C or more.
Objective signs
Pimples on the surface of the mucous membrane of the posterior pharyngeal wall during an acute process:
- red;
- edematous;
- increased in size;
- stand out clearly;
- slightly raised.
They are located randomly, in groups or at great distances from each other, but without obvious limitation to a specific area. The mucous membrane also turns red, swells, and is covered with mucopurulent discharge.
University
Currently, methods for rapid diagnosis of streptococcal antigen in smears from the surface of the tonsils and/or posterior pharyngeal wall (Streptatest, STREP-A-CHECK-1, Binax-Strep A) have become widespread, which allow obtaining results within 15–20 minutes . However, despite their high specificity (95–100%), they are characterized by lower sensitivity (60–80%) than culture tests.
However, neither cultural examination nor rapid tests make it possible to differentiate patients with ATP of streptococcal etiology from asymptomatic carriers of GABHS with intercurrent viral infection.
According to the 2012 ESCMID (European Society for Clinical Microbiology and Infectious Diseases) guidelines, smear culture for GABHS is not recommended routinely in all patients with acute sore throat. If there is a high probability of GABHS based on the assessment on clinical scales, rapid diagnostics should be carried out whenever possible; in the case of a negative result of the rapid test, bacteriological examination is not performed.
The IDSA (Infectious Diseases Society of America) recommends increased use of the rapid test and/or culture of the posterior pharyngeal swab because clinical symptoms are not considered reliable in differentiating ATF caused by viruses from GABHS unless severe symptoms of a viral infection (runny nose, cough, hoarseness and/or ulcerative lesions of the oral mucosa).
In children and adolescents, negative results of the rapid test should be confirmed by culture (in adults, this is not necessary due to the low prevalence of GABHS infection and the extremely low risk of developing rheumatic fever in the future). If the rapid test is positive, culture testing is not advisable. In children under 3 years of age, classic streptococcal ATP practically does not occur, and testing for GABHS in this age group is indicated only if it is diagnosed in a brother or sister.
Laboratory data also do not always allow one to distinguish a bacterial infection from a viral one. Markers of bacterial infection can be considered leukocytosis more than 15 x 109/l, neutrophilia more than 10 x 109/l and/or band forms more than 10% or more than 1.5 x 109/l, CRP more than 70 mg/l. Lower numbers or a significant increase in only one of these indicators are often found with viral infections. Thus, in 1/3 of children with tonsillitis caused by adenoviruses and the Epstein-Barr virus, leukocytosis exceeds 15 x 109/l, and CRP exceeds 60 mg/l. On the other hand, low marker numbers do not necessarily rule out a bacterial infection. Thus, laboratory markers of inflammation do not always help in the diagnosis of streptococcal infection, their diagnostic value is lower than that of catarrhal symptoms, and routine biochemical blood tests are not recommended for ATP.
Serological diagnosis of GABHS infection has become widespread. Most often in general clinical laboratories it is limited to determining the titer of antibodies to streptolysin O (ASL-O). True GABHS infections always cause a specific immune response—an increase in ASL-O titer. The determination of ASL-O in venous blood is a highly sensitive and specific (about 80%) reaction; the determination of ASL-O in capillary blood is much less reliable.
The synthesis of antibodies in general and ASL-O in particular depends on the individual characteristics of the immune response: in some it is pronounced and long-lasting, in others it is slow. Antibody synthesis starts 1–2 weeks after the onset of streptococcal infection, but even 8 weeks after GABHS tonsillopharyngitis, the ASL-O titer may not reach its maximum. ASL-O can remain at very high levels for up to a year.
The value of ASL-O in the acute period does not give any indication of the risk of developing immune complications and does not depend on the severity of the disease. On the other hand, if the patient has an increased ASL-O already in the first three days from the onset of tonsillopharyngitis, this excludes an acute streptococcal infection and indicates that the patient suffered from it within a period of 2 weeks to 6-12 months before the examination or suffers from chronic tonsillitis . Immune complications (glomerulonephritis, ARF) develop 3–8 weeks after GABHS infection; if they did not arise within these periods, then it is hardly possible to assume their development in the future (even despite the increased level of ASL-O).
It is necessary to clearly understand that ASL-O are antibodies of antigen recognition, and not of its elimination, and not treat the patient with antibiotics in order to normalize this indicator. The immune process has a certain stage, which develops despite the death of the pathogen. It is the infection that needs to be treated, not the elevated ASL-O level! Determination of the ASL-O titer is recommended only in cardiorheumatology and nephrology to prove the streptococcal etiology of heart and kidney damage.
To diagnose the streptococcal etiology of ATF, determination of the level of antibodies is not used; the diagnosis is verified by cultural methods. This test can be used to differentiate active infection from a carrier state. (The meaning of the definition of ASL-O was described in sufficient detail by Alexander Lavrinovich in “MV” dated January 5, 2022).
There are early and late (immune) complications of GABHS infection.
Early complications are represented by cervical lymphadenitis, paratonsillitis, parapharyngitis, retropharyngeal and peritonsillar abscesses. The etiology of these complications is associated with a combined flora (GABHS and anaerobes) penetrating into the peritonsillar tissue and lymph nodes from the depths of the lacunae in severe tonsillitis or as a result of injury, for example, during processing or shading of the tonsils. In this case, the patient, despite the treatment, continues to have fever, pain when swallowing, turning the head, and opening the mouth. Upon examination, asymmetry of the pharynx and bulging of the pharyngeal wall are revealed.
Immune complications of GABHS infection, which include post-streptococcal acute glomerulonephritis and acute rheumatic fever, are well known to clinicians. The latter disease develops in 0.3% of patients with untreated GABHS tonsillitis, of which 40% develop chronic rheumatic heart disease. Adequate ABT reduces the risk of developing acute rheumatic fever (ARF) by 80% and peritonsillar abscess by 85%.
The so-called rheumatogenous GABHS strains have a number of specific properties. Of particular importance is M-protein, a type-specific antigen located in the outer layer of the cell wall. Antibodies to M-protein cross-react with various tissues of the host body according to the principle of molecular mimicry as the main pathogenetic mechanism for the development of immune complications of GABHS infection. In addition, protein M has the properties of a superantigen, causing polyclonal activation of lymphocytes and the formation of low-affinity antibodies, which can lead to impaired tolerance to self-tissue antigens and the development of autoaggression, especially in genetically predisposed patients. These properties were noted in serotypes M-3, M-5 and M-18.
Immunopathological complications of GABHS infection develop in the convalescence stage. Acute glomerulonephritis manifests itself on the 7th–10th day of illness, and adequate therapy for angina does not reduce the risk of its development. The clinical manifestations of ARF appear 2–3 weeks after the symptoms of ARF are relieved, and fever occurs in no more than 30% of patients. However, even in the acute period of ATF, disorders of the internal organs are detected. Changes in the cardiovascular system are characterized by tachycardia, muffled or weakened heart sounds.
When body temperature normalizes, tachycardia gives way to bradycardia, and the dullness of heart sounds becomes even more pronounced. In 1/3 of patients in the acute stage of the disease, microhematuria is detected, which disappears when the intoxication syndrome is relieved. These pathological changes are associated with the direct effect of streptococcal toxins (exotoxins, streptokinase, hyaluronidase, etc.) on organs, are not related to immunopathological reactions and do not require any anti-inflammatory or immunosuppressive therapy.
White pimples on the tongue closer to the throat: what are they?
Sometimes a person experiences the phenomenon of pimples on the tongue closer to the throat. This problem is common, but not everyone tries to find out the reasons and get rid of it. Why do pimples appear on the root of the tongue? The reasons for this pathology lie in damage to the mucosa during mechanical action or the influence of bacteria. Usually the pimples at the base of the tongue are small. But large defects often appear, which begin to hurt and cause discomfort when swallowing salivary fluid and food. This is often accompanied by plaque, which indicates the proliferation of pathogenic microbes and a weakened immune system.
If pimples appear on the tongue closer to the pharynx, there are various reasons. In many situations, this problem is caused by damage to the mucosa or tissue injuries. When tissue is damaged, small swelling or inflammatory processes appear. They are red and quickly disappear after proper treatment.
The appearance of white pimples closer to the larynx is more dangerous. They may indicate serious diseases, tissue damage from pathogens. One of the reasons is stomatitis. It is of bacterial origin, and the cause of this disease can be the consumption of unwashed fruits, failure to comply with personal hygiene rules, and a weakened immune system.
Features of the appearance of white pimples on the tonsil (tonsil) in the throat
To accurately determine the cause of this phenomenon, you need to take into account the location, size and corresponding symptoms. Based on their location, pimples on the tongue are divided into:
- tip of the organ;
- closer to the larynx;
- on the side of the bridle.
The color of the tubercle may also differ. They can be white, red or black (these are very rare). Often the tubercle that appears hurts, causes discomfort, and a burning or tingling sensation is felt. The reasons for this phenomenon may be different; the duration of therapy depends on the timeliness of their detection.
Please rate the article:
Prevention
To avoid the appearance of pimples in the throat caused by infections, you should follow the rules of prevention.
Photo: drinking plenty of fluids helps moisturize the oral mucosa and prevent the penetration of germs
Therefore, all measures should be aimed at strengthening it.
- Fresh and cool air helps to moisturize the mucous membranes and coat them with a natural secretion - saliva, which has an antibacterial effect.
- Drinking plenty of fluids prevents dehydration of the body and drying out of the mucous membranes.
- A balanced diet or taking complex vitamins will help strengthen the entire body as a whole and local immunity.
- You should not get carried away with antiseptics and antibiotics, as all microbes get used to them and stop responding to the drugs.
- Systematic hardening will gradually teach the body not to get sick. Ice cream, cool water from the refrigerator, a contrast shower, walks in the fresh air are the best helpers in this.
Causes of pimples in the throat
Among throat diseases, there are many that are characterized by various rashes on the mucous membrane of the tonsils and pharynx, which can be accompanied by pain of varying intensity. Lesions that resemble pimples may appear as a rash or inflamed follicles.
In any case, when a rash is detected in the throat, we have to talk about viral or bacterial inflammation, which develops in the following diseases:
- follicular tonsillitis;
- stomatitis;
- abscess;
- chronic pathologies of the respiratory tract;
- bacterial and viral infections.
The appearance of pimples in the throat can be caused by a decrease in the immune system, which occurs as a result of:
- hypothermia;
- lack of vitamins;
- poor nutrition;
- alcohol and tobacco abuse;
- recent use of antibiotics;
- presence of chronic diseases or oncology;
- ARVI;
- stress and fatigue;
- autoimmune diseases.
Only a specialist can determine the exact diagnosis and establish its cause, after the necessary examination. Only when the cause of the rash is established will the doctor be able to prescribe proper treatment.
Video: “Aphthous stomatitis”
Pimples in the throat are signs of diseases, usually of an infectious nature. The most common diseases that result in white rashes or appear as a white pimple in the throat are follicular tonsillitis, inflammation of the tonsils, which is chronic. Also, pimples on the mucous membrane occur as a result of stomatitis, but they are red in color, and the localization of the rashes is usually in the mouth and occasionally in the throat.
If a child has a white pimple in the throat, on the tip of the tongue or on the tonsil, which is accompanied by no fever, then the treatment will be the same as for an adult, unless of course it is a completely newborn.
Pimples in the throat are usually painful; the patient feels a sharp pain when swallowing. In addition, this disease is characterized by soreness, which causes severe discomfort to the person.
Typically, pimples are located on the tonsils (or tonsils), which perform a protective function in the body and recognize and trap pathogenic microorganisms that enter the human body through the oral cavity. If, as a result of stress or some other reason, the body’s immune status decreases, the tonsils are the first to be attacked, and as a result of the ingress of bacteria, a sore throat occurs, the manifestation of which is a rash in the form of blisters or pimples in the throat.
A white pimple in the throat is accompanied by other symptoms, which manifest themselves as pain in the ears, fever, enlarged lymph nodes, general weakness, headache, etc. If the rash in the throat is purulent in nature, then an unpleasant odor from the mouth will be noticeable.
What to do if a white pimple pops up in your throat
Pimples in the throat should be treated after consulting a doctor and finding out the cause of the disease. However, there are several folk methods that will help relieve inflammation and speed up the healing process. My patients took advantage of the doctor’s advice, thanks to which they can get rid of problems in 2 weeks without much effort.
To gargle, you can prepare an infusion of 1 tablespoon of eucalyptus mixed with linden and chamomile flowers. Pour boiling water over this mixture and leave for 30 minutes. It is recommended to gargle with this infusion 5 times a day.
Mixed aloe juice with water in a 1:1 ratio, which should be used to gargle a sore throat, will also help relieve inflammation. An infusion of willow bark will help speed up the healing of the affected mucosa. Gargle with this infusion 5 times a day.
In addition, you can prepare inhalations by boiling two tablespoons of a mixture of mint, sage and chamomile, then remove the decoction from the heat and breathe in the steam for 10-15 minutes. 10-minute inhalations of propolis will also be effective. To do this, place 1 tablespoon of propolis in a liter of boiling water.
As a rule, if you have acne in the throat, the doctor prescribes antibiotics appropriate to your condition, anti-inflammatory drugs, gargles, soft foods, and plenty of fluids. Also, if the condition requires it, then bed rest may be prescribed. To prevent the development of the disease, you should take care of your immunity. Take vitamins, stay cool and avoid stress.
Diseases that cause a rash in the throat
The color of pimples in the throat depends on the nature of the inflammation. If the causative agent of the disease is bacteria, then we are talking about a process, therefore, the pimples will be filled with white or yellowish color.
The inflammatory process, which is caused by a virus, is usually accompanied by red rashes.
The number of rashes also indicates the nature of the disease. For example, a small number of pimples (from 3 to 5) most likely indicates a mild viral illness, which is not accompanied by a number of symptoms that worsen the patient’s well-being.
Anginal rash
White rashes or spots in the throat are a symptom of herpetic and follicular tonsillitis. Its development is promoted by bacterial infection. In this case, the lymph nodes and follicles of the throat mucosa resemble pimples. Pimples are localized on the back of the throat. All of them are no larger than the size of a pinhead and are white in color.
In addition to blisters and ulcers, sore throat is characterized by other symptoms:
- heat;
- redness and enlargement of the tonsils;
- acute sore throat;
- intoxication;
- headache.
Follicular tonsillitis is characterized by a gradual increase in pimples, which often open on their own. In this case, minor bad impurities are observed in the patient’s saliva. The danger of a sore throat is that it can cause complications:
- rheumatism;
- cardiac dysfunction;
- renal colic.
Herpetic sore throat is characterized by the appearance of formations in the throat, which are called vesicles. Its development is caused by enteroviruses. Sore throat, which is provoked by streptococci and staphylococci, is characterized by the appearance of pimples in the throat.
Other diseases
The inflammatory process with the appearance of a rash can occur against the background of bronchial asthma and allergic reactions.
The appearance of bumps on the back of the throat can be caused by candidiasis. This disease is also called thrush; its appearance is caused by the proliferation of fungal microflora.
Blisters in the throat can be caused by stomatitis. However, they most often appear on the inside of the cheeks and gums. Rashes on the surface of the tonsils and throat appear extremely rarely.
Diseases may appear due to bacterial pharyngitis. This condition is typical for childhood. In addition to rashes on the mucous membrane of the throat, bacterial pharyngitis manifests itself:
- increased body temperature;
- swelling of the throat;
- sore throat;
- white pimples on the tonsils.
The presence of scarlet fever in the throat is accompanied by the formation of red pimples. The development of the disease is facilitated by infection with streptococci A. The disease most often affects children from 2 to 10 years old.
Folk remedies
A rash in the throat may be accompanied by severe pain. To eliminate unpleasant sensations, traditional medicine, in particular rinsing solutions, will come to the rescue. This procedure should be carried out after meals, at least 4-6 times a day.
Solutions and rinses will help relieve sore throat
- Recipe 1. Dilute 0.5 tsp in 100 ml of milk. soda, add a piece of butter and season with ginger.
- Recipe 2. Dilute 1 tsp in 500 ml of warm water. salt. Exactly the same proportions for preparing a soda solution.
- Recipe 3. Pour 200 ml of boiling water over 2 tbsp. l. mint, chamomile, eucalyptus. After rinsing, you can suck 1 tbsp. l. honey If there is no fever, you can do herbal inhalation or breathe over hot water in which propolis is diluted.
If pimples in a child’s throat are caused by thrush, the plaque should be removed in the following way: wrap a bandage around your finger, dip it in a soda solution and wipe the affected area.