Glossitis is a disease that affects the tongue and appears in the form of spots, inflammation and swelling, and severe itching. The reasons are an inadequate diet, irritating external factors, such as smoking, alcohol, certain toothpastes, or the habit of constantly sucking lollipops.
The disease takes such forms as:
- median rhomboid;
- folded;
- interstitial;
- black hairy;
- Gunter's;
- desquamative.
Based on duration and severity, acute and chronic forms are distinguished. In the first case, swelling, inflammation of the surface, changes in the color and structure of the tongue are observed. With chronic glossitis, papillomas, fungal growths, and severe pain can develop.
Causes
Factors that provoke the development of inflammatory processes include:
- Diarrhea and food poisoning - harmful substances released during bowel movements negatively affect the papillae;
- An inactive lifestyle - this contributes to the appearance of stagnant processes in the pelvis;
- Constipation, in which the papillae are injured during bowel movements;
- Abuse of enemas - with frequent procedures, the mucous membrane of the anal canal is damaged;
- Drinking alcoholic beverages;
- Allergy to personal hygiene products, underwear material;
- Proctological diseases: critpitis, proctitis.
Symptoms
The main signs of the disease are:
- the appearance of uneven plaque with pronounced white spots;
- ulcers form along the entire surface, gradually spreading to the rest of the oral cavity;
- tongue mobility is limited, sharp pain appears when talking or eating;
- color changes, local spots of different shades are visible;
- swelling, there are tooth marks on the side areas;
- impaired salivation;
- there is an unpleasant odor from the mouth.
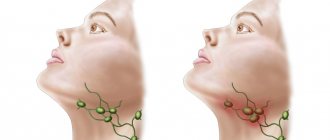
In some cases, the sense of taste changes or disappears, and a burning or itching sensation is felt at the slightest movement. As it progresses, body temperature rises, cervical and submandibular lymph nodes enlarge.
Diagnostics
If papillitis is suspected, the proctologist performs:
- Visual inspection;
- Palpation;
- Anamnesis collection.
If the nodules are located inside the anus, the patient will have to strain to get them out.
To obtain information about the condition of the rectum, the patient is referred to:
- Anoscopy - an anoscope is used for examination, which allows you to examine a section of the rectum 10-12 cm long from the anus and diagnose various proctological pathologies: polyps, bleeding, etc.
- Sigmoidoscopy - allows you not only to examine the rectum at a distance of up to 25 cm, but also to take samples for histology and to excise detected tumors.
Mandatory diagnostic measures include laboratory tests: stool, blood and smear analysis, flora culture, etc.
The need for differential diagnosis is due to the fact that the symptoms of papillitis are similar to some other proctological diseases. Therefore, in order to accurately establish a diagnosis, it is important to exclude the development of other pathologies. Hypertrophied papillae develop a stalk, so they resemble a polyp in many ways. Sometimes you need to make sure that these are not sentinel tubercles formed by fissures in the anus.
Treatment
If the papillae are in normal condition and do not bother a person, then they do not require medical intervention. Therapy is needed in case of development of inflammatory processes. The following can be used to treat papillitis:
- Conservative techniques;
- Operational methods.
But initially the cause of the disease must be eliminated. Without this, only temporary results can be achieved. If you undergo a course of medication or surgical treatment, but do not eliminate the root cause of the formation of the papillae, then after some time they will become inflamed again.
Conservative treatment
In this case, the doctor prescribes medications with anti-inflammatory, analgesic, antimicrobial and immunomodulatory effects. If the patient suffers from constipation, then the treatment regimen includes laxatives, and for diarrhea, medications to normalize stool. Colloidal solutions may also be prescribed to facilitate bowel movements.
Nutrition is of no small importance. The diet for papillitis should include light foods aimed at improving intestinal activity. Therefore, it is recommended to consume more vegetables, fruits, and dairy products. Sweets, fried, spicy and salty foods should be excluded from the diet. The consumption of alcoholic beverages is strictly prohibited. The patient must also stop smoking.
Operational methods
Surgical treatment consists of excision of the tumor. For this purpose the following is used:
- Radio wave technique - removal of papillae using the Surgitron device, the action of which is based on the generation of high-frequency radio waves into thermal energy. Heat, acting on cells, stimulates their evaporation;
- Ligation with latex rings - the essence of the technique is to throw a ring onto the pedicle of the hypertrophied papilla in order to compress the vessels that feed the neoplasm cells. After this, the papilla shrinks and as a result it disappears.
Prevention of papillitis
To avoid inflammation of the anal papillae, it is recommended:
- Observe hygiene procedures: rinse the anus after each act of bowel movement;
- If gastrointestinal diseases are detected, undergo timely treatment;
- Move more to eliminate congestion in the pelvic area;
- Get rid of bad habits (smoking, drinking alcohol);
- Avoid “heavy” foods;
- In case of constipation, use laxatives.
Hypertrophied anal papillae. Treatment of inflammation of the anal papillae
Inflamed anal papillae, papillitis, fibroanal polyps are an acute or chronic proctological disease characterized by pain, intense itching in the anus, sensation of a foreign object, discomfort and difficulty during defecation, sphincter spasm. The cause of inflammation is hypertrophied anal papillae (papillae) - anatomical nodular intraluminal formations at the level of the anorectal line, normally not exceeding 1 cm and having a pale pink color. Under normal conditions, a proctologist can detect them next to the Morganian crypts during palpation of the anorectal area.
Papillae are classified into two types based on their shape:
- cone-shaped with a wide base;
- spherical on a narrow stalk.
Cause and symptoms of papillitis
Problems begin when the formations become inflamed, multiply in size, and acquire a red-purple hue. At the initial stage of the disease, discomfort occurs only during bowel movements. When the disease progresses for a long time, the inflamed anal papillae may even protrude from the rectum, which significantly aggravates the problem. Also, when they grow up to 3 cm, they may be pinched by the sphincter muscles, which is accompanied by acute pain spreading to the coccyx area.
The initiation of the inflammatory process occurs at the time of frequent mechanical injury to the papillae from feces and penetration of infection into the tissue, which is typical for chronic constipation. Another way is possible, when the papillae are irritated under the influence of toxins eliminated by the body after poisoning.
Patients report the following symptoms:
- “foreign body” in the anus;
- pain that gets worse with bowel movements;
- burning and swelling at the base of the anus;
- formation of erosions;
- traces of blood;
- the appearance of mucus from the anus due to weakening of the sphincter function.
Provoking factors for inflammation of the anal papilla include:
- inactive lifestyle and poor circulation in the pelvis, including obesity and pregnancy;
- regular constipation and trauma to the rectal mucosa;
- food poisoning;
- abuse of cleansing enemas;
- allergies to the composition of linen, personal hygiene products;
- excessive alcohol consumption;
- proctological diseases (cryptitis, hemorrhoids, proctitis).
Diagnostic features
Hypertrophy of the anal papillae and the development of the inflammatory process are easily detected by a proctologist when examining the rectal area. The nature of the patient’s complaints is of great importance, since papillitis can manifest itself against the background of other problems. The peculiarity of the diagnosis is that enlarged anal papillae are similar in shape to tumor-like growths in rectal polyposis. They can also be confused with the so-called sentinel tubercle (a sign of chronic anal fissure) or hemorrhoidal node. In this regard, to make an accurate diagnosis, a detailed examination with mirrors can be performed, and anoscopy can also be prescribed.
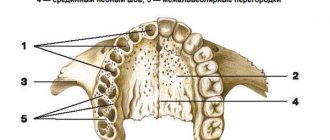
Differences between hypertrophied anal papillae (papillitis) and polyposis:
- the papillae are externally pale, covered with multilayered squamous epithelial tissue;
- polyps in one layer are covered with columnar epithelium to match the color of the mucous membrane;
- papillae are located approximately at the level of the anorectal line;
- Rectal polyps are always localized above the anorectal level.
If during a routine examination the proctologist discovered papillae in you, you should not panic - this is normal if their appearance and location do not go beyond the norm. If they give you anxiety, have signs of inflammation or fall out of the rectum, then the need to remove the hypertrophied anal papillae is obvious. This must be done so that one trouble is not joined by others, more serious and potentially dangerous. In some situations, a histological examination may be required, when a piece of tissue is sent to the laboratory to be analyzed for malignant degeneration.
Treatment of inflammation and hypertrophy of anal papillae
Modern proctology uses two types of treatment: medication and surgery. When choosing a tactic, the attending physician does not rely on the fact of the presence of hypertrophied papillae, but on the cause of their inflammation. So, if the formations are inflamed against the background of hemorrhoids, then it should be treated first, and if they are accompanied by proctitis, then the treatment of proctitis is paramount. As clinical practice shows, when diagnosing a chronic anal fissure (fissure), removal of the anal papillae is considered a strict necessity.
Drug treatment
For isolated inflammation of the anal papillae, treatment with medications is successful. As part of therapy, the following are prescribed:
- special diet;
- warm baths, enemas with antiseptic, astringent, bacteriostatic effects;
- anti-inflammatory suppositories;
- antibacterial therapy.
Surgery to excise hypertrophied anal papillae is indicated in rare cases. Removal is recommended if drug treatment does not bring results, the papillae are large in size, the anal papillae constantly fall out of the anus, their surface is covered with ulcers. Surgery is also necessary when the development of papillitis occurs against the background of another disease of the anorectal mucosa.
Surgical treatment regimen for hypertrophied anal papillae
Two modern methods of surgical intervention are considered the most successful:
- surgery using the Gabriel method - the surgeon excises the anal papilla along with the adjacent crypt;
- cryodestruction of inflamed papillae is a minimally invasive operation using liquid nitrogen to remove the anal papilla.
The surgical intervention is performed on an outpatient basis in a specialized proctology setting, under local or intravenous anesthesia.
Forecast
In the majority of patients, after drug treatment of anal papillae, complete regression of symptoms is recorded, so the prognosis of the disease is favorable. Enlargement and inflammation of papillae in themselves do not threaten human life. But it should be understood that with this diagnosis, neither acute nor chronic inflammation of the anal canal structures occurs independently. With complicated papillitis, the prognosis worsens. To prevent the development of paraproctitis, pectenosis and other serious ailments, you need to be examined, determine the nature of the phenomenon and take the necessary measures.
Prevention of papillitis
To prevent relapses that will lead to a new need for surgical treatment of the anal papillae, the patient should:
- carefully care for the perianal area;
- give up “wrong” nutrition, fight constipation;
- promptly identify and treat gastrointestinal diseases;
- give up bad habits and unconventional sex;
- be moderately active, avoid stagnant processes in the pelvis.
After excision of hypertrophied anal papillae and in the absence of pathological neoplasms in the rectum, the patient should undergo an annual follow-up examination.
How to treat anal papillae if they are inflamed
At the initial stage, the disease is asymptomatic or with minimal symptoms. Therefore, in this case, the appearance of regular discomfort indicates that the disease is in full swing. If you suspect that your anal papillae are inflamed, do not engage in amateur activities. This can be fraught with serious health consequences and interfere with further quality of life. If you experience any discomfort, and even more so with pain in the rectum and anal canal, do not hesitate to make an appointment with a doctor. The sooner the diagnosis is made, the easier it is to restore health!
Many are afraid of surgical intervention for complicated hypertrophied anal papillae, having heard enough horror stories. In fact, high-precision, minimally invasive surgical methods are now used, so the risks are minimal compared to the prospects of refusing treatment. If it is important for you that the operation is performed by a male proctologist surgeon, contact the best private proctology in Rostov on the street. 2nd Five-Year Plan, 29/5. Dr. Tolokhyan has more than 20 years of experience in practical medicine, 16 years of experience in proctology/surgery and hundreds of grateful patients.