Pharyngitis is an inflammatory process that forms on the back wall of the larynx and affects the mucous membrane, as well as deeper layers, tissues of the soft palate and lymph nodes. The acute form of pharyngitis can develop into chronic if the patient does not seek help from a doctor and self-medicates.
Since the pathological process in the larynx is caused by the spread of pathogenic bacteria, the risk of developing pharyngitis increases in people with a weak immune system and in those who suffer from ENT diseases or are predisposed to them.
How dangerous is pharyngitis and how does it manifest itself? Which doctor should I contact and how to treat the disease? We will answer these and other questions in this article.
Reasons for the development of pharyngitis
Experts believe that the peak development of pathology occurs at the end of winter and the beginning of spring, since at this time the human immune system is especially susceptible to colds. Often in the spring season, a lack of vitamins and microelements in the human body leads to the appearance of vitamin deficiency, the body weakens and creates an excellent environment for the development of pathogenic bacteria. Inflammatory processes are also possible: both separately and against the background of the underlying disease.
The first signs of pharyngitis and its further treatment may differ depending on the stage of the pathology, gender, age and general health of the patient.
We include the following as the main reasons for the development of pharyngolaryngitis:
- hypothermia, eating too cold foods;
- deformation of the nasal septum;
- strains of microorganisms that cause the development of chlamydia, candidiasis, whooping cough, scarlet fever, measles;
- adenovirus, influenza virus;
- streptococci, staphylococci, pneumococci;
- sinusitis, tonsillitis, caries, rhinitis;
- difficulty breathing through the nose;
- pathologies of the gastrointestinal tract: reflux, heartburn, hernia;
- abuse of bad habits;
- regular high loads on the vocal cords;
- polluted, toxic air;
- hormonal disorders and endocrine pathologies (diabetes mellitus, obesity, hypothyroidism, etc.);
- tonsillectomy, which was performed on the patient previously;
- infectious diseases in chronic form;
- weakened immunity.
Preventive measures to prevent stomatitis in children
To minimize the risk of developing stomatitis you need to:
- wash the child’s toys, bottles and other things regularly, and do not forget to thoroughly wash the baby’s hands;
- strengthen the child’s immunity;
- do not let your child bite his nails;
- create a balanced menu containing all the necessary minerals and vitamins. The diet should be followed;
- promptly treat diseases such as tonsillitis, gastritis and other gastrointestinal diseases. If you extinguish the outbreak in time, this will prevent stomatitis from developing;
- At least once a year, and preferably twice, visit the dentist for a detailed examination of the oral cavity.
All these simple recommendations will help avoid the occurrence of stomatitis, because any disease is much easier and cheaper to prevent than to treat it later. If it was not possible to avoid the disease, at the first signs of it, you must consult a doctor to prescribe effective treatment. If stomatitis appears again and again, a thorough immunological examination is required. The child should be examined by a pediatrician and an immunologist; it is also advisable to contact an endocrinologist and gastroenterologist (perhaps they will identify a chronic disease leading to relapse of the disease).
It is equally important to teach your child proper oral hygiene. If the teeth are affected by caries and covered with plaque, and there are fistulas on the gums, the fight against stomatitis will not be successful. A child must be taught how to properly brush his teeth and gums by buying him a brush and toothpaste appropriate for his age.
Symptoms of pharyngitis
The first signs of the disease may differ depending on the type of pharyngitis. They are both local and general in nature. But there are common signs that are characteristic of any type of pharyngitis: sore throat, bad breath, stuffy ears and difficulty swallowing. With an active inflammatory process, an increase in body temperature above 38° can be observed - this is how the body fights a foreign infection. General signs: sweating, poor appetite, weakness, dizziness, fatigue, fever, chills. Some complain of pain and noise in the ears, and discomfort when exposed to loud sounds.
- During acute catarrhal pharyngitis, swelling and redness of the mucous membranes of the larynx appears. Also, red follicles may form on the back wall of the throat, and clear and slightly cloudy mucus may accumulate. There is swelling and redness of the tongue.
- In the purulent form of acute pharyngitis, ulcers with an accumulation of purulent masses appear on the surface of the posterior pharyngeal wall.
Acute pharyngitis
Acute pharyngitis can occur independently, and can also be accompanied by acute inflammation affecting the upper respiratory tract: rhinitis or inflammation of the mucous membranes of the nasopharynx.
Depending on the cause of development, acute pharyngitis occurs:
- Viral – most often caused by rhinovirus;
- Bacterial – caused by streptococci, staphylococci and pneumococci;
- Fungal – source of the inflammatory process – Candida;
- Traumatic - caused by damage to the pharynx and larynx: the throat was scratched by a sharp bone or burned by boiling water, severe stress on the ligaments;
- Allergic – occurs when inhaling allergens or irritants, such as tobacco, exhaust fumes or dusty air.
Causes of pathology
The infection is caused by group A streptococcus. A person can be either a carrier of the pathogen or an active source of infection. The greatest contagiousness is observed in the first 1-4 days of the acute period. 3 weeks after the onset of the disease, the likelihood of the infection spreading is reduced to zero. Up to 20% of the adult population are asymptomatic carriers of streptococcus. There is a seasonal dependence: the largest number of infections is recorded in the autumn-winter period against the background of acute respiratory viral infections, tonsillitis, and pneumonia.
Chronic pharyngitis
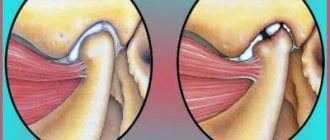
According to the depth of damage to the pharyngeal mucosa, chronic pharyngitis is divided into: catarrhal, hypertrophic and atrophic forms.
- Chronic catarrhal pharyngitis - there is slight swelling of the tissue layers of the pharyngeal mucosa. Individual areas are sometimes covered with clear or slightly cloudy mucus. It develops as a result of acidic gastric contents entering the throat, for example, in the case of a hiatal hernia. Therefore, catarrhal chronic pharyngitis is a consequence of the development of diseases of the gastrointestinal tract.
- Chronic hypertrophic pharyngitis is a significant severity of swelling of the mucous membrane. Additionally, thickening of the uvula and swelling of the soft palate are observed.
- Chronic atrophic pharyngitis is characterized by some thinning of the lining of the pharynx. They are usually pale pink, sometimes shiny varnished. Some of their areas become covered with crusts, viscous mucus and pus.
Any type of chronic pharyngitis develops due to the fact that the acute form of the disease was not cured in time and developed into a more serious form. Chronic pharyngitis also appears as a consequence of rhinitis, sinusitis, deviated nasal septum, nasal polyps - that is, when nasal breathing is difficult for a long time. In addition, long-term use of vasoconstrictor drops also leads to the appearance of chronic pharyngitis.
Reasons for the appearance of pimples
Pimples on a child's tongue appear due to exposure to irritating factors - in some parts of the tongue, the surface of the mucous membrane becomes stratified, under which fluid accumulates. This could be blood, serous exudate, pus, or microbial waste products. Therefore, the appearance of the pimples varies. They are red, transparent, white, yellowish.
In general, pimples on the tongue may appear due to the following reasons:
- injuries, burns, contact with very cold things: for example, a scratch from an uncut nail, too hot porridge or milk, or it could be touching metal with your tongue in the cold,
- stomatitis of various origins: most often the “culprits” of the rashes are the Candida fungus and the herpes simplex virus. Additionally, the surfaces of the gums, palate,
- inflammation of the tongue (glossitis): inflammation begins due to the harmful effects of bacteria and viruses, as well as metabolic disorders,
- general diseases of the body: rashes often appear with chickenpox, scarlet fever, diphtheria, sore throat, with pathologies of the digestive or hormonal systems,
- allergies: sometimes manifests itself to new foods, hygiene products, washing powders, toothpaste, cosmetics.
How does pharyngitis manifest and progress in children?
Children suffer from pharyngitis more severely than adults. This especially applies to babies under one year old. Swelling of the mucous membrane can cause signs of suffocation; the pain that accompanies the disease reduces the child’s appetite. Often, a baby’s body temperature can reach 40°. The most difficult thing in this situation is that a small child cannot say what hurts.
Incorrect treatment can lead to irreparable consequences for a small, fragile organism. Therefore, at the first signs of pharyngitis, consult a doctor immediately.
Causes of bubbles on a child’s tongue
In order to help the child as quickly as possible and prescribe appropriate treatment, it is necessary to determine the causes of the formation of bubbles on the child’s tongue. The very first reason why the mucous surface of a child’s tongue becomes covered with pimples is thrush. Often, this disease affects young children whose immunity is severely weakened. Small white bubbles form not only on the surface of the tongue, but throughout the entire oral cavity.
Treatment consists of frequent wiping of the mouth with a tetraborate solution, which contains glycerin. Sometimes doctors prescribe glycerin-based borax. All these drugs are easily available and are available even without a doctor's prescription. Therapy is carried out as follows. Take a piece of clean bandage and wrap it around your index finger, then moisten it generously in the liquid and gently wipe your tongue, and then your entire mouth. Try not to press on the tongue as this may trigger the baby's gag reflex. A similar treatment of the oral cavity should be carried out after each meal.
Sore throat and pharyngitis: what is the difference?
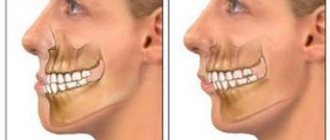
The general condition of the patient with acute tonsillitis or tonsillitis can be confused with the symptoms of pharyngitis. If the disease is diagnosed incorrectly, then treatment of pharyngitis in adults will not have any effect. And the acute form of the pathology can develop into a chronic one.
Unfortunately, many patients self-medicate and start using medications without a doctor’s specific prescription. This is extremely contraindicated! It is better to take care of your health in time and seek help from an experienced otolaryngologist.
It is important to remember that during pharyngitis, the larynx becomes inflamed, and during tonsillitis, the tonsils become inflamed. During a sore throat, it is always painful to swallow, and the pain intensifies even more when eating food. With pharyngitis, the opposite happens - while eating warm food or warm drinks, the sore throat decreases.
During the development of a sore throat, there is no cough or sore throat, only a sore throat and sometimes the formation of a white coating. With pharyngitis, there is a sore throat, as well as noise, pain, or congestion in the ears. The difficulty in distinguishing between these two diseases is further complicated by the fact that one patient can simultaneously develop both pathologies, since they are caused by the same pathogen.
Principles of treatment
The disease does not require hospitalization. All events are held at home.
Scarlet fever in children: how to treat a contagious disease:
- antibiotics (penicillin group) for a course of 10 days;
- antitoxic serum;
- gargling with a solution of furatsilin, a decoction of chamomile, calendula, eucalyptus;
- in case of dehydration - intravenous infusion of saline preparations;
- symptomatic therapy – antipyretics, non-steroidal anti-inflammatory drugs;
- gentle diet, bed rest.
The modern approach to the treatment of streptococcal infections guarantees a favorable outcome without serious consequences. Re-infection is diagnosed in 1-3% of patients.
Diagnosis of pharyngitis
Detection of all types of pharyngitis begins with a visual examination of the larynx using a special device and taking an anamnesis. A throat swab is also taken for examination to test for diphtheria.
Other types of diagnostics:
- Cultural examination - inoculation of taken materials on a nutrient medium.
- Rapid diagnosis - identification of streptococcal antigen in throat swabs.
- Immunoserological diagnosis - the method is used in case of streptococcal infection.
Laboratory research:
- Complete blood count – exclusion of blood diseases, infectious mononucleosis;
- A general urine test helps rule out kidney disease (glomerulonephritis).
Depending on the symptoms of the disease, as well as the condition of the larynx, the presence or absence of cough, fever, plaque on the tonsils and soreness and increased size of the lymph nodes, additional consultations with other specialists may be necessary: an endocrinologist, a cardiologist, an allergist.
Ulcers caused by trauma
The main reason for the appearance of ulcers when the mucous membrane is injured is infection in the wound. Most often, white rashes occur due to the habit of biting nails or the tip of a pencil or pen.
Fans of seeds and hard toothbrushes may also be at risk. Many people believe that hard bristles remove plaque better. Actually this is not true. If you carefully brush your teeth with such a brush, you can damage the enamel, gums and cause inflammation.
Other causes of mucosal injury:
- uncomfortable dentures;
- braces or other orthodontic structures;
- habit of unconsciously biting your cheek or tongue;
- exposure to mucous membranes with drugs or acids.
How to treat?
It is enough to remove the irritating factor and wait 1 - 2 weeks. Usually the ulcers go away on their own. If this does not happen, it is recommended to consult a doctor.
Treatment methods for pharyngitis
Treatment must be comprehensive. The patient is prescribed medications that will relieve pain and reduce inflammation. It is also important to adhere to a special diet and exclude from the diet foods that irritate the mucous membrane of the throat and bring even more discomfort: alcoholic beverages, spicy and salty foods, sour foods, carbonated drinks.
Drug therapy
Depending on the clinical picture and general condition of the patient, the doctor may prescribe antihistamines, antitussives and antiviral medications. Lozenges/lozenges are used to relieve pain.
In some cases, they resort to the use of antibiotics. They can only be taken as directed by a doctor.
Local impact
Rinsing with special solutions also has a good effect on the inflammatory process and redness of the larynx. They have a gentle effect, relieve pain and improve the general condition of the patient.
To diagnose and identify the disease, you need to consult an otolaryngologist. At the city clinic, you can contact your primary care physician, who will issue a referral to an ENT specialist. However, this takes time. You often have to wait 2 weeks for an appointment with a doctor. In some cases, this is simply impossible, since it is necessary to quickly conduct an examination and prescribe treatment before the situation becomes critical.
Therefore, we recommend contacting the Medunion medical clinic. We employ practicing otolaryngologists, and you don’t have to wait several weeks for appointments. Sign up today for a time convenient for you, and get tested tomorrow.
Patients choose us because we provide the service of a specialist coming to your home if you cannot come to the clinic on your own. You can also take samples directly at home.
The cost of an initial consultation with an otolaryngologist in Krasnoyarsk at the Medunion clinic starts from 1,300 rubles. You can sign up on the website or by calling 201-03-03.
Aphthous stomatitis in children
Manifests itself in the form of small individual ulcers on the lips and oral mucosa. Its appearance is provoked by:
- allergic reactions of various types (to food, medications, etc.);
- staphylococci (there are many of these bacteria in carious formations and dental plaque);
- immunity disorders;
- liver diseases.
Aphthous stomatitis in children: symptoms and treatment
Exacerbation occurs mainly in autumn and spring. Ulcerations most often form on the lips, tongue and inside the cheeks (in these places the mucous membrane comes into contact with food and can be injured by the teeth).
Sometimes weakness in the body and fever appear, but often the general condition of the body remains normal.
The size of the ulcers (ulcers) is 5-10 mm. They are covered with a grayish coating and are surrounded by a red, inflamed rim of mucous membrane. There is pain when touching them. It happens that only 1 ulcer forms.
Aphthous stomatitis in children: treatment
The causes of stomatitis in children will influence the nature of treatment. Immediately after the first symptoms appear, it is necessary to adjust the child’s menu, completely eliminating the main allergens (chocolate, honey, berries, citrus fruits, etc.). During illness, you should also not eat spicy foods with added spices.
Often, aphthous stomatitis becomes a reaction of the body to medications, so if a child is taking medications, it would be a good idea to consult a doctor.
Treatment methods:
- Antiallergic drugs. The most frequently prescribed are Suprastin, Diazolin and many others like them.
- Treatment of ulcerations. At the initial stage of the disease, “Miramistin” (they are recommended to spray the aphras using a special sprayer that comes with the drug) and “Cholisal” (ulcers are treated with gel at least 3 times a day) perform well. When the acute symptoms of the disease pass, you can use Solcoseryl, a gel that accelerates the healing of mucosal defects and has an analgesic effect.
- Exposure to UV rays in a physiotherapy room.
- Use of immunomodulators. Firstly, it is worth purchasing a special toothpaste based on lactoferrin, and secondly, you can take a course of Imudon.
- Sanitation of the oral cavity. Since one of the causes of stomatitis is microorganisms, all carious formations must be cured and plaque removed.