Oral syphilis
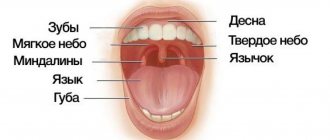
The diagnosis of “oral syphilis” is based on the patient’s complaints, medical history, clinical examination, and the results of additional research methods. With primary syphilis of the oral cavity, the dentist usually identifies one hard chancre. On palpation, the resulting ulcerative surface is painless, regular rounded, red in color with smooth, raised edges and an infiltrated sebaceous bottom. Lymph nodes are compacted, enlarged, painless, and not fused to the skin and surrounding tissues. With secondary syphilis of the oral cavity, residual syphilomas are found, as well as a roseolous-papular rash on the palate, arches, and tonsils. Scraping the papules leads to exposure of erosive surfaces. In case of relapse of secondary syphilis of the oral cavity, fewer rash elements are formed, papules and roseolas are pale in color, grouped, forming figures resembling garlands and lace.
With secondary syphilis of the oral cavity, polyadenitis is detected. Unlike catarrhal tonsillitis, pain when swallowing and high temperature reaction are not observed with syphilitic lesions. In tertiary syphilis of the oral cavity, a gummous infiltrate is detected, after the disintegration of which a deep crater-shaped ulcerative surface is formed. The integrity of the jaws and nasal bones is compromised. The affected areas become scarred, leading to permanent deformities. There is no enlargement of regional lymph nodes. The detection of treponema pallidum in scrapings or in the contents of lymph nodes confirms the diagnosis of oral syphilis. To identify syphilitic lesions, serological reactions are also used, which in patients become persistently positive, starting from 4 weeks from the moment of formation of chancre. The first 3 weeks of primary oral syphilis are a seronegative period, since at this time it is not possible to confirm the diagnosis using serological reactions.
Radiographically, in patients with tertiary syphilis of the oral cavity, zones of rarefaction of bone tissue in areas corresponding to gummous lesions, as well as sclerotic changes along the periphery, are diagnosed. There is destruction of the cortical bone layer and signs of periostitis ossificans. Oral syphilis is differentiated from a decubital ulcer, a malignant tumor, tuberculous and actinomycotic lesions, tonsillitis, chancriform pyoderma, Setton's aphthae, lichen planus, and leukoplakia. The patient is examined by a dentist or dental surgeon. If a specific syphilitic infection is suspected, the patient is referred for consultation to the dermatovenerological department.
Syphilis CLO. Clinic, diagnosis, treatment.
⇐ PreviousPage 31 of 38Next ⇒
Syphilis is a chronic infectious venereal disease that can affect all organs and tissues, including the maxillofacial area.
Etiology. The causative agent of syphilis, Treponema pallidum (spirochete), develops in the human body as a facultative anaerobe and is most often localized in the lymphatic system. Treponema pallidum can be spiral-shaped, encysted and L-shaped.
Clinical picture. The disease has several periods: incubation, primary, secondary and tertiary.
Manifestations of syphilis in the tissues of the face, jaws and oral cavity are observed in the primary, secondary and tertiary periods of the disease, and some changes are also observed in congenital syphilis.
The primary period of syphilis is characterized by the appearance of primary syphilomas or chancre on the mucous membrane, including in the oral cavity. In the secondary period of syphilis, the mucous membrane of the oral cavity is most often affected and pustular or roseolous elements are formed. These manifestations of syphilis are discussed in the course of therapeutic dentistry.
A rare manifestation of syphilis in the secondary period is damage to the periosteum. It covers a significant area of the periosteum of the jaw,
often lower. This specific lesion is characterized by a slow and sluggish course. The thickened periosteum acquires a doughy consistency, but a subperiosteal abscess does not form. Gradually, the affected areas of the periosteum become denser, and flat elevations appear.
The tertiary period of syphilis develops 3-6 years or more after the onset of the disease and is characterized by the formation of so-called gummas. Gummas can be localized in the mucous membrane, periosteum and bone tissue of the jaws. It should be borne in mind that manifestations of syphilis in the tertiary period do not always occur. In this regard, active or manifest syphilis and latent tertiary syphilis are distinguished.
When syphilitic gummas form, a dense, painless node first appears, which gradually opens with rejection of the gumma core. The resulting gummous ulcer has a crater-shaped shape and is painless on palpation. Its edges are smooth, dense, the bottom is covered with granulations.
When the periosteum of the alveolar process is damaged, teeth may be involved in the process, percussion becomes painful and mobility appears. The process from the periosteum can transfer to the bone.
The radiograph reveals foci of osteoporosis in areas of the bone corresponding to the location of the gumma in the periosteum, as well as loss of bone along the surface of the cortical layer in the form of a lesion. When teeth are involved in the process, the compact lamina of their alveoli is destroyed. The growth of the periosteum gives a wavy shadow along the edge of the jaw on the radiograph, as well as sometimes the phenomenon of ossifying periostitis.
Diagnostics. The clinical diagnosis of syphilis is supported by the Wasserman reaction and other serological reactions. Microbiological examination (detection of Treponema pallidum), as well as pathomorphological examination of the affected tissues, are important.
Treatment of syphilis is carried out in a specialized venereological hospital or dispensary.
Simultaneously with the general treatment of syphilis of the mouth and jaws, local therapy is prescribed - washing of syphilitic elements, ulcerations, fistulous tracts with various antiseptic solutions, most often with a 2% chloramine solution. Every 3 days, excess granulations are cauterized with a 10% solution of chromic acid. If syphilis affects the bone tissue of the jaws, it is advisable to periodically study the electrical excitability of the dental pulp; if indicated, trepanation of teeth with dead pulp and treatment according to the principles of therapy of chronic periodontitis. With the development of specific periodontitis, despite significant mobility of teeth, they should not be removed. According to indications, dental treatment is performed with root canal filling; After specific treatment, the teeth are strengthened quite well.
When a secondary pyogenic infection occurs, general and local use of medications that affect the microbial flora is indicated.
Active surgical treatment for damage to the periosteum and jaws with syphilis is not indicated even in the case of sequestration formation. They are removed after specific treatment against the background of subsidence and delimitation of the process.
Hygienic maintenance of the oral cavity is important. Tartar is removed, sharp edges of the teeth are removed, and the oral cavity is cleaned.
⇐ Previous31Next ⇒
Recommended pages:
Symptoms
The clinical course of syphilis is characterized by alternating periods of active manifestations and latent stages of the disease, a variety of clinical and morphological signs at different stages of the disease.
There are four periods of the clinical course of syphilis: incubation, primary, secondary and tertiary.
The incubation period (from the moment of introduction of Treponema pallidum until the appearance of the first clinical symptom of syphilis - chancre) lasts on average 3-4 weeks. This period may be longer in individuals taking small doses of antibiotics for the treatment of intercurrent illnesses; in the presence of severe concomitant pathology, as well as in elderly people.
Primary syphilis (syphilis primaria lues I) . The duration of primary syphilis is on average 6-7 weeks. It is characterized by the appearance at the site of introduction of Treponema pallidum of a painless inflammatory infiltrate - chancre (primary syphiloma). 5-7 days after the formation of hard chancre, the second obligatory symptom of the primary period appears - regional lymphadenitis (scleradenitis). It is expressed in an increase in regional lymph nodes. They grow to the size of a pea, plum or walnut, remaining painless. On palpation, the lymph nodes have a dense elastic consistency, are not fused to each other and surrounding tissues, and are mobile; the skin over them is not changed. Regional lymphadenitis persists much longer than primary chancre. When hard chancre is localized in the area of the oral mucosa and skin of the maxillofacial region, the submandibular, anterior and posterior cervical, and occipital lymph nodes enlarge. In these nodes, intensive reproduction of trepanema occurs.
Hard chancre can be single, but there can be 2-3 of them. Most often it is located on the red border of the lips, mucous membrane of the tongue, palatine tonsils, less often on the gums, mucous membrane of the cheeks, soft and hard palate, or in other areas. The diameter of chancre is on average 5-10 mm, but it can be significantly smaller - from 1 to 3 mm (dwarf chancre) and 1.5-2.0 cm or more (giant chancre). The size, shape, depth of the lesion, and the severity of the chancre depend on its location, the state of the body’s reactivity, and the presence of concomitant diseases.
The development of hard chancre on the oral mucosa in typical cases begins with limited hyperemia and thickening due to the inflammatory infiltrate.
Then its central part becomes necrotic and a flesh-red, painless erosion or superficial saucer-shaped ulcer of a round or oval shape with raised, smooth edges is formed. At the base of the erosion or ulcer, a dense cartilage-like infiltrate is palpated. The bottom of the ulcer is smooth, shiny, meat-red in color, without plaque or covered with a grayish-yellow “greasy” coating.
Atypical forms of chancre are often encountered. In this case, a hard chancre may take the form of a crack, abrasion, erosion, or seizure with a slight infiltrate at the base. Its shape depends on the location.
Sometimes chancre may appear as a limited thickening without erosion. This form is found on the lips - hypertrophic chancre. It is characterized by the appearance of a hemispherical dense formation in the form of a mushroom cap, rising sharply above the level of the red border of the lips, with a diameter of up to 2-3 cm. Its surface is shiny, with scanty discharge. More often, when localized on the lips, the chancre has the appearance of an erosion or ulcer, covered with a brown crust that rises above the surface of the lip.
On the tongue, a hard chancre, due to a pronounced inflammatory infiltrate at the base, protrudes sharply above the level of surrounding tissues and has the shape of a saucer turned upside down. In persons with a folded tongue, the chancre is localized along the folds and has a slit-like shape.
When hard chancre is located in the corners of the mouth, it clinically resembles jams with infiltration at the base.
On the gum, a hard chancre has the appearance of a bright red erosion, which in the form of a crescent is adjacent to several teeth.
When localized on the tonsil, hard chancre can have one of three forms: ulcerative, sore throat-like (amygdalitis) and combined (ulcerative against the background of tonsillitis-like). The tonsil is affected only on one side. It acquires a copper-red color, is enlarged, dense, and painless. In the ulcerative form, an oval flesh-red ulcer with gently sloping, even edges appears against this background. The mucous membrane around the ulcer is hyperemic. The process may be accompanied by pain, sometimes significant.
In an unsanitized oral cavity with poor hygiene, chancroid can be complicated by fusospirochetosis, a staphylococcal infection. Due to the development of an acute inflammatory process, the typical clinical symptoms of syphilis are obscured, pain appears, purulent or necrotic plaque appears at the bottom of the ulcer, and the depth of the ulcer increases.
Secondary syphilis (syphilis secundaria, lues II).
The secondary period of syphilis occurs after the primary, 2-3 months after infection. Its clinical picture is much more varied in the nature of the rashes on the oral mucosa and skin, which is a reflection of the dissemination of the infection. There is a generalization of the process with damage to the mucous membranes in the form of a characteristic rash (syphilides), disturbances in the general condition of the body (malaise, weakness, low-grade fever, headaches, arthralgia); Damage to internal organs, bone and nervous systems, hearing and vision organs is possible. The oral mucosa is one of the favorite places for the localization of syphilides in this stage of syphilis, both secondary fresh and recurrent. Manifestations on the oral mucosa occur simultaneously with the skin ones, but can be isolated. The disease has a wave-like course with a change in active manifestations and clinically hidden (asymptomatic) periods.
Secondary syphilis is characterized by high contagiousness, focal arrangement of elements, frequent absence of subjective sensations, true or false polymorphism. At this stage of the disease, mainly two types of lesions occur in the oral cavity: macular (macular) and papular syphilides.
Spotted syphilide is represented by one of the most common manifestations of secondary syphilis - syphilitic roseola. It appears in the form of a bright red, rounded spot, 0.5-1.0 cm in diameter, sharply demarcated from the unchanged oral mucosa and disappears with pressure. Roseolas tend to coalesce into copper-red erythema. The lifespan of roseola without treatment is about 1 month, during which its shape and color practically do not change.
Syphilitic roseola is most often localized on the mucous membrane of the palatine arches (symmetrically), soft palate, uvula and tonsils. On the skin, roseola is detected on the lateral surfaces of the body, on the chest, abdomen, and less often on the neck, face, and limbs. Patients have no subjective sensations. With recurrent syphilis, roseola occurs without acute inflammatory phenomena; when grouped, they form foci in the form of rings, arcs, semi-arches, etc.
Syphilitic roseola in the oral cavity should be differentiated from drug-induced catarrhal stomatitis, which is accompanied by burning and soreness of the oral mucosa. All symptoms quickly disappear after stopping taking the medications that caused them.
Erythematous syphilitic tonsillitis should be distinguished from banal catarrhal tonsillitis, in which there is pain, increased body temperature, swelling, and soreness. Differential diagnosis is also carried out with allergic drug lesions of the oral mucosa, which differ from erythematous syphilitic sore throat in the prevalence of the lesion: not only the arches and tonsils are involved, but also the cheeks, tongue and other areas.
Syphilitic roseola rash sometimes has to be differentiated from manifestations of other infectious diseases on the oral mucosa (measles, rubella, typhoid, typhus).
Papular syphilide is the most common form of manifestation of secondary syphilis in the oral cavity, especially its recurrent stage. Papular rashes can form anywhere on the mucous membrane, but most often occur on the tongue, lips, tonsils, soft palate and arches, where they often merge into large plaques. Papular rashes with secondary syphilis are distinguished by a variety of manifestations. They differ in size, shape, color, depth of lesion, outline and many other characteristics. Papules are dense, painless elements with a diameter of 1.0-1.5 cm, protruding above the level of the oral mucosa. They are round or oval, have clear outlines, and are not prone to merging. When the papules resolve, a rim of exfoliating epithelium appears (like Biette’s “collar” on the skin). The color of papules during their development changes from pink-red to copper-red. They are painful, separated from the unchanged mucous membrane. Due to constant maceration in the oral cavity, papules acquire a grayish-white color and tend to grow peripherally. Merging into plaques, they sometimes rise above the level of the oral mucosa. When scraped with a spatula, the plaque covering the papule is removed and the meat-red erosion underneath is exposed. There is an inflammatory rim around the papule. Papules and discharge from the surface of erosions contain a large number of treponemas.
On the oral mucosa, papular syphilides are more often found in the form of an erosive-ulcerative form and are very similar to banal aphthae. In an unsanitized oral cavity, with poor hygienic care, papules can ulcerate or be complicated by fusospirochetosis. In the center of the papules, as a result of maceration and frequent injuries, deep erosion is formed, and sometimes even an ulcer covered with a purulent and bloody coating. In this case, the clinical picture becomes similar to Vincent's stomatitis; significant pain and an area of hyperemia around the papules appear. When papules are localized in the corners of the mouth, due to constant trauma, they can grow and spread to the skin. When opening the mouth, the infiltrated skin and mucous membrane are injured, forming deep bleeding painful cracks, covered with crusts, against the background of a dense infiltrated base.
On the tongue, papules are often localized on its lateral and dorsal surfaces. As a result of constant trauma and exposure to saliva, they are transformed into extensive erosive and ulcerative surfaces, covered with a grayish-whitish coating, with uneven edges and tightly fused to the surrounding tissues.
Often, similar rashes spread to the posterior parts of the oral cavity: the anterior and posterior palatine arches, tonsils and the posterior wall of the pharynx, resulting in hoarseness (syphilitic dysphonia). There are no subjective sensations, with the exception of the feeling of a foreign body.
On the back of the tongue, in the places where papules appear, filiform and mushroom-shaped papillae disappear and elements appear that resemble foci of desquamation, smooth, shiny, sinking below the level of the mucous membrane (“mown meadow plaques”).
Tertiary syphilis (syphilis tertiaria, lues III).
In the tertiary period of syphilis, gummas and tuberculate rashes form on the oral mucosa and on the skin. The disease is characterized by damage to internal organs, nervous and skeletal systems.
Ummotic syphilide can be localized anywhere in the oral mucosa, but is more often observed on the soft and hard palate, as well as on the tongue. Usually a single gumma appears. A painless node forms in the thickness of the oral mucosa, which gradually increases, reaching 1.0-1.5 cm or more in diameter. The center of the gumma is then opened to reveal a deep, crater-shaped ulcer with a necrotic core in the center. The ulcer is painful, surrounded by a dense infiltrate, the mucous membrane over which is colored bluish-brown. Its edges are smooth, not undermined, meat-red in color, covered with small juicy granulations, and bleed easily. As the ulcer clears, its bottom becomes covered with granulations. Healing of the ulcer leads to the formation of a retracted star-shaped scar. This process lasts 3-4 months and is almost not accompanied by subjective sensations. Less commonly, gumma is reabsorbed, followed by cicatricial atrophy or transformed into a dense fibrous node.
Depending on the location of gumma, its clinical picture has certain features. Gummy lesions of the tongue can occur either in the form of the formation of individual gummas (nodular glossitis), or in the form of diffuse sclerotic glossitis, which is the most severe form of damage to the oral mucosa in syphilis. Initially, diffuse infiltration of part of the tongue or its entire thickness occurs, as a result of which the tongue increases, and no nodes are formed.
The tongue is dense, “wooden” (as a result of sclerosis), the papillae are smoothed. Subsequently, the infiltrate is replaced by scar tissue, which gradually tightens the tongue, which leads to limited mobility and reduction in size. The back of the tongue becomes unevenly lumpy, cracks appear both longitudinally and transversely, and deep grooves separate the lobules of the inflammatory infiltrate (reminiscent of a quilt). Speech and eating are impaired, and the tongue is easily injured. In case of infection, erosions and ulcers are formed that are prone to malignancy.
The color of the mucous membrane of the tongue depends on the stage of the process: it is bright or dark red in the active stage and grayish-white with a pearlescent tint in the sclerosis stage. There are also combinations of sclerotic glossitis with gums - sclerotic-gummous glossitis. In this case, along with the fibrosclerosing process of the tongue, truly gummous infiltrates are formed in its individual lobules. The period of formation of the gummous infiltrate in the thickness of the tongue is painless, while the appearance of cracks on the sclerotic surface is accompanied by pain, which makes moving the tongue, eating and talking almost impossible.
When gumma is localized on the hard palate, bone tissue and periosteum are very quickly involved in the process, bone necrosis, sequestration, extensive defects, and perforation of the hard palate occur.
Tuberous syphilide on the oral mucosa is less common than gummous syphilide. The tubercles, like gummas, can appear anywhere in the oral mucosa, but are more often localized on the lips, alveolar process and palate. Tuberous syphilide on the oral mucosa is painless, dense tubercles of bluish-red color with a smooth surface with a diameter of up to 0.5 cm (rarely more). They tend to form in groups and then disintegrate quite quickly to form small, deep ulcers. The edges of the ulcers are compacted due to the presence of a dense syphilitic infiltrate, not undermined. After the ulcers heal, rough scars form, on which new tubercles never appear.
Tubercular syphilide on the oral mucosa is characterized by a relatively rapid course: usually several months from the onset of occurrence to the formation of a scar.
Regional lymph nodes in tertiary syphilis may not respond to the process in the oral cavity and give a nonspecific reaction to the addition of a secondary infection.
Syphilis of the tongue in the secondary period of the disease
During the secondary period of syphilis, erosive papules most often appear on the mucous membrane of the tongue - papular syphilide.
Rice. 7. Papules on the tongue are oval in shape, bright red in color, painless and highly contagious.
Rice. 8. The photo shows syphilis of the tongue in the secondary period of the disease. The papules are round, dark pink, single or multiple, devoid of papillae (“mown meadow symptom”).
Rice. 9. Secondary period of syphilis. Papules on the tongue.
Syphilis - types and stages of the disease.
Congenital syphilis is said to occur when a child, while still in the womb, becomes infected from a sick mother. During pregnancy, syphilis can cause fetal death, miscarriage, or stillbirth. Among children born with syphilis, early and late forms of the disease are distinguished. Symptoms of early syphilis appear between the 2nd and 10th weeks of a baby's life and most often include:
- facial deformities (saddle nose, Olympic forehead, poorly developed jaw bones);
- spots, bumps and syphilitic blisters;
- osteochondritis.
Lack of treatment or starting therapy too late can lead to a late form of syphilis, the characteristic symptoms of which are:
- recurrent effusions from the joints;
- interstitial keratitis;
- saber-shaped shins;
- deafness due to damage to the auditory nerve,
- pathological changes in the dentition (the so-called Hutchinson's teeth).
During pregnancy, you should have a blood test to rule out the disease. Treatment of a pregnant woman in the first months of pregnancy increases the likelihood of having a healthy child. During secondary syphilis, doctors distinguish between early and late stages, which are divided into many clinical stages and latent periods.
On average, it takes 21 days from infection to the onset of symptoms, but this period can be extended to three months. We are talking about the early form of syphilis in the first two years after infection. In turn, late syphilis is a much more dangerous stage of the disease, which in the long term leads to serious damage to the musculoskeletal system, cardiovascular, nervous systems, as well as the eyes and brain.
What provokes it?
The source of infection can be medical instruments, including dental ones, if their sterilization regime is violated. A prerequisite for infection with syphilis is a violation of the integrity of the stratum corneum of the skin or the epithelium of the oral mucosa (cracks, abrasions, etc.), although it is believed that the pathogen can penetrate through an intact mucous membrane. Infection with syphilis is also possible when treponema pallidum enters the blood directly, for example during blood transfusions or other medical procedures (injection, surgery, etc.).
Medical workers (usually gynecologists and dentists) can become infected when treating patients, conducting gynecological and dental examinations, operations, opening abscesses, periodontal interventions, as a result of careless handling of endodontic and other instruments. The most dangerous source of infection are patients with active manifestations of syphilis in the primary and secondary periods when the lesions are localized on the genitals and oral mucosa.