Salivary glands – increased salivation and dry mouth
There are a number of tips to help keep
your salivary glands healthy:
First, you need to drink plenty of water. Secondly, you should use chewing gum that does not contain sugar. And thirdly, it is necessary to suck on lollipops, which also do not contain sugar.
In certain cases, your dentist may recommend gargling with artificial saliva. The above drug is sold in spray or liquid form. You do not need a prescription to purchase it, but use it several times a day. However, artificial saliva does not contain proteins, minerals and other necessary elements that are contained in natural salivary fluid. Thus, the above drug will simply be useless for digestion.
Bile in the stomach (duodenogastric reflux)
Duodenogastric reflux is the reflux of the contents of the duodenum into the stomach cavity. Normally, after a certain period of time after food enters the stomach, a portion of bile is released into the lumen of the duodenum, aimed at further, more thorough digestion of the food bolus. The presence of bile creates an alkaline environment in the cavity of the duodenum. At the border of the stomach and duodenum there is a pyloric sphincter, which prevents the movement of food in the opposite direction and separates the acidic environment of the stomach from the alkaline environment of the duodenum. If the function of the sphincter is impaired, for example, if it is not fully closed, the alkaline contents of the duodenum enter the stomach. Burning has an irritating effect on the gastric mucosa, which, when exposed to it regularly, causes a chronic inflammatory process called reflux gastritis.
Excess saliva in the mouth
By and large, a large amount of saliva is not a problem if the condition is not systemic. Typically, the amount of saliva you produce depends on what you drink or eat. In a healthy person, the body easily eliminates excess salivation. In general, excessive salivation is caused by overactivity of the salivary glands, as well as if a person has a disturbed swallowing process.
If you eat a spicy dish during your lunch break, your body will begin to intensively secrete saliva. This is because the taste buds on the tongue help increase the volume of fluid produced. For a visual example, you can put something sharp on your tongue. After a few moments, you will be able to feel a rush of saliva into your mouth. Also, sour foods affect excessive salivation. Accordingly, you can reconsider your diet if you are concerned about excess salivary secretion. In addition, the above symptom may occur as a result of certain diseases and abnormalities, as well as due to the use of special medications.
The role of saliva
As experts explain, saliva performs several important functions at once: it washes away food debris from the teeth, softens food, facilitating its subsequent digestion, and even supplies teeth with calcium, strengthening them. Indeed, chronic dry mouth is often a harbinger of caries. However, our body must produce exactly as much saliva as is necessary to ensure these important processes, and not a drop more. Drooling and the need to constantly swallow saliva can be signs of increased saliva secretion, which can cause a lot of discomfort.
Diseases that cause increased salivation
Experts note a number of diseases that cause our salivary glands to work hard. Among them: central and peripheral paralysis, gastroesophageal reflux disease, mental development disorders, abnormally large tongue, Parkinson's disease, pregnancy (severe toxicosis), poisoning, stroke, rabies.
In addition, there are a number of drugs that cause excess salivary fluid. These include: drugs against schizophrenia, antiepileptic drugs, as well as medications prescribed to patients undergoing radiotherapy. The common medical term for excess salivation is sialorrhea or hypersalivation.
Drooling (sialorrhea, hypersalivation, ptyalism) is characterized by an increase in the amount of saliva with its flow from the oral cavity through the border of the lips in such a volume that it negatively affects the social and domestic activities and daily life of the patient, leading to damage to the soft tissues of the oral cavity, lips and chin . Parkinson's disease (PD) is the most common cause of sialorrhea in adults. The incidence of this suffering in PD varies from 45 to 80% [1, 2]. Some researchers note a lower prevalence of sialorrhea - 10%. Initially, drooling only bothers you at night, but later, as the disease progresses, it also occurs during the day. Although the association of sialorrhea with PD has been known since the time of J. Parkinson's classic monograph, the pathophysiology of sialorrhea has not been sufficiently studied.
Functioning of the salivary glands under physiological conditions
Depending on the size, small and large salivary glands are distinguished. The minor salivary glands are localized in the mucous membrane of the lips, cheeks, tongue, hard and soft palate. The large salivary glands are located outside the mouth. Three pairs of major salivary glands (parotid, submandibular, sublingual) produce and secrete saliva. Parotid glands ( glandula parotidea
) are located directly under the skin, in front and downward from the auricle, on the lower jaw, at the posterior edge of the masticatory muscle.
The external carotid artery and its branches pass through the parotid gland. Per day, the parotid glands secrete about 1/3 of the volume secreted by all salivary glands (approximately 0.2-0.7 liters of saliva).
Submandibular salivary gland ( glandula submandibularis
) is located superficially, under the cervical fascia and skin. Medially it borders with the styloglossus and hyoglossus muscles, above with the lower jaw, and below it emerges from under its lower edge. In front, the gland is in contact with the posterior edge of the mylohyoid muscle, and laterally it is adjacent to the facial artery and vein. The submandibular gland secretes saliva containing both mucous and serous (protein) secretions.
Sublingual gland ( glandula sublingualis
) is located immediately under the mucous membrane of the floor of the mouth, on both sides of the tongue, on the upper surface of the mylohyoid muscle. Laterally it comes into contact with the inner surface of the body of the lower jaw, medially with the genioglossus, geniohyoid, and hyoid-glossus muscles. The sublingual glands secrete saliva containing a serous (protein) secretion. It is richer in mucin than the saliva of the parotid and submandibular glands, has a pronounced alkaline reaction and high phosphatase activity [3].
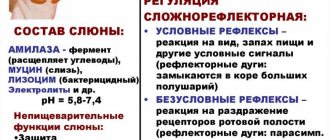
The secretory activity of the salivary glands is regulated by the salivary zone of the cerebral cortex and the nuclei of the brain stem. This zone is excited by signals coming from taste buds. Next, the cortical zones interact with the upper (in the region of the parvocellular reticular nucleus) and lower (in the lateral part of the reticular formation) salivary centers of the brain stem.
The secretory activity of the salivary glands is provided by sympathetic and parasympathetic innervation. However, when eating and swallowing, the activity of parasympathetic innervation is mainly activated. Parasympathetic afferent pathways, receiving a signal from the receptors of the pharynx and esophagus, reach the salivary center located in the medulla oblongata through the system of the vagus nerve and visceral nerves [2–4].
Parasympathetic efferentation occurs through two pathways. The glossopharyngeal nerve innervates the auricular ganglia and subsequently the parotid gland via the auriculotemporal nerve. The facial nerve innervates the submandibular ganglia through the chorda tympani and then through the lingual nerve ensures the functioning of the submandibular and sublingual glands [5] .
The process of salivation is inextricably linked with swallowing. The act of swallowing consists of three phases: oral, pharyngeal and esophageal. The oral phase is voluntary, while the pharyngeal and esophageal phases are involuntary. The act of swallowing begins with the involvement of more than 30 different muscles of the oropharynx to form and move the bolus of food into the esophagus. Subsequently, the upper esophageal sphincter (EES) opens and the food bolus passes from the pharynx into the esophagus and then into the stomach [2, 6]. Central motor control of swallowing function is provided by the premotor cortex, primary motor cortex, basal ganglia, pedunculopontine nucleus, and cerebellum. Central neurons project to the stem swallowing centers, in particular the nuclei of the solitary tract (common to the facial, glossopharyngeal and vagus nerves, providing taste sensitivity). These centers further regulate the functions of structures involved in the swallowing process, such as the tongue, muscles of the larynx, pharynx and upper esophagus. At the same time, the muscles of the tongue are controlled by the nucleus of the hypoglossal nerve; the muscles of the larynx, pharynx and upper esophagus are controlled by n . a mbiguous
(common to the vagus and glossopharyngeal nerves) [4, 7]. In patients with PD, the oropharyngeal phase of swallowing is predominantly affected.
Function of the salivary glands in PD
Two causes of drooling in BP are actively debated. One of them is a violation of saliva production, and the other reason may be insufficient saliva utilization. Overproduction of saliva can certainly cause drooling. However, many studies have shown [8, 9] that patients with PD produce even less saliva than healthy people. The exact mechanisms causing the decrease in salivation remain unknown [10].
A decrease in salivary secretion in PD may reflect the involvement of the stem salivary nucleus and cranial autonomic ganglia. One possible explanation is a dopamine deficiency. Experimental studies in animal models have shown that dopamine modulates salivary secretion [11, 12]. Studies in rats have demonstrated that activation of central and peripheral dopamine receptors induces salivation [11]. It is known that damage to the striatum, globus pallidus and the descending pathway to the lateral part of the reticular formation of the midbrain can significantly reduce salivation [13]. Pathological studies have revealed the presence of Lewy bodies in patients with PD both in autonomic formations (in the superior cervical ganglion, sympathetic trunk of the cervix, peripheral vagus nerve) and in the submandibular gland [14]. Although Lewy bodies are found in peripheral ganglia, involvement of the cranial parasympathetic ganglia in the degeneration process has not been established. Dopamine has been confirmed to stimulate salivation, even with the administration of the peripheral D2 receptor blocker domperidone, which is indirect evidence of the involvement of higher levels of regulation in this system, including the basal ganglia and brainstem, which may be responsible for reducing salivation in these patients [15]. .
Studies assessing the intensity of production and rate of salivary excretion of the parotid glands using scintigraphy did not show a difference in saliva production, but the rate of saliva excretion to discrete stimuli was significantly higher in patients with PD compared to healthy controls [16, 17]. Thus, increased salivary flow is not a major contributor to the pathophysiology of drooling in BP. However, increasing the excretion rate partially increases sialorrhea.
In PD, the function of the blood-salivary barrier is disrupted, its permeability to calcium, magnesium and zinc increases and the concentration of copper in saliva decreases. Taking levodopa brings the permeability of the blood-salivar barrier closer to functional compliance with healthy ones [18]. Thus, dopamine regulation of not only the volume of saliva secreted, but also the ratio of its mucosal and serous components and elemental composition is not excluded.
Swallowing dysfunction may be one of the leading causes of drooling in patients with BP. It is known that the dorsal motor nucleus of the vagus nerve is affected already in the early stages of PD, although other central regulators of swallowing remain intact for a long time. At the same time, the pedunculopontine tegmental nucleus, which modulates the activity of the medulla oblongata nuclei, is also affected quite early in PD.
The nucleus ambiguus regulates the function of the striatal muscles of the pharynx and upper esophagus. The dorsal motor nucleus of the vagus nerve controls the intermuscular nerve plexuses of the smooth muscles of the esophagus. While the myenteric plexus and dorsal nucleus are affected in the early stages of PD, the pathology of the oral and pharyngeal stages in patients with PD at the onset of the disease is associated not with the involvement of the nucleus ambiguus, but with a violation of the supramedullary control of swallowing.
Oropharyngeal phase disruption found in PD may contribute to the accumulation of saliva in the oral cavity. Oropharyngeal dysphagia is thought to result from bradykinesia. Animal studies have shown that after injection of 6-hydroxydopamine (6-OHDA), the rate of tongue protrusion slows down in experimental rats, and the average duration of tongue pressure becomes significantly longer compared to the control group [19]. Another study [20] showed that the maximum tongue pressure in patients with severe stages of PD was weaker compared to patients with early or moderate stages, and the transit time of the bolus in the oropharynx was negatively correlated with the speed of tongue movement. Both studies reflect the fact that patients with PD have bradykinesia of the oropharyngeal phase of swallowing and impaired tongue muscle function.
Thus, dysfunction of tongue control contributes to dysphagia and may be a cause of drooling. A videofluorographic study in a model of parkinsonism in rats (after injection of 6-OHDA) showed a slower progression of the food bolus compared to the control group [21].
A study using barium in patients with drooling in PD demonstrated a direct correlation between the severity of dysphagia and the severity of sialorrhea [22]. Scintigraphy showed the presence of subclinical manifestations of dysphagia in all patients with sialorrhea. Patient complaints of drooling aggravated swallowing disorders [17]. Thus, oropharyngeal dysphagia may be a major pathophysiological factor in drooling in PD.
Another cause of drooling may be impaired motility of the upper esophagus. Data from manometric studies provided evidence of impaired EEC relaxation in patients with PD compared with controls.
Often, a manifestation of PD is a dystonic swallowing disorder [23]. In this case, dysfunction of the pharyngo-cricoid muscles leads to dysphagia. The pharyngo-cricoid muscles are the upper sphincters of the esophagus. Accordingly, impairment of their ability to adequately relax during swallowing can lead to impairment of the ability to swallow solid food. This condition is often called crico-pharyngeal achalasia and is characterized by insufficient relaxation of the upper esophageal sphincter in duration and severity.
However, this factor cannot be the only cause of dysphagia, and if the patient has sufficient pharyngeal propulsive force, swallowing will not be significantly affected [24, 25]. There is probably a combination of disturbances in the oropharyngeal and esophageal phases of swallowing.
Hypomimia, involuntary opening of the mouth, slouching or drooping head can also lead to inability to retain saliva in the mouth [26]. At the same time, there is no evidence that drug-induced dyskinesias can cause drooling. Thus, today three main mechanisms of sialorrhea in PD are considered: increased secretion of saliva, inability to retain saliva in the oral cavity (hypomimia, involuntary opening of the mouth, stooping or drooping head), deterioration of salivary clearance (lingual bradykinesia, oropharyngeal dysphagia, upper sphincter dysfunction esophagus).
Epidemiology and maladjustment
On average, 50% of patients with PD complain of drooling, subclinical sialorrhea is objectified (videofluoroscopy) in 90% [2, 7]. Drooling is present in 86% of patients with dysphagia and only 40% without it [27].
Patients suffering from excessive salivation experience difficulty articulating speech and swallowing, and have bad breath. Constant leakage of saliva from the oral cavity forces one to resort to the use of handkerchiefs or towels, leading to perioral cracking, irritation, and maceration of the skin. Wetness and soiling of clothes and bedding increases the burden on caregivers. Psychologically, excessive drooling can lead to decreased self-esteem and social isolation.
Treatment methods
Treatment of sialorrhea in PD includes methods aimed at reducing saliva production with the prescription of acetylcholine transport blockers, cholinesterase inhibitors; use of clozapine and quetiapine; improvement of motor symptoms of PD with dopaminergic agents and surgical neuromodulation. However, the effectiveness of these methods is only partial, and new pharmacological and non-pharmacological approaches to the treatment of sialorrhea are needed. For this purpose, various groups of drugs are being studied, including anticholinergic drugs, adrenergic receptor antagonists, and botulinum toxins (BTX).
Anticholinergic drugs.
For selective action, blockers of M3-cholinergic receptors, predominantly localized in the salivary glands, are required. This way you can avoid side effects such as confusion, hallucinations, constipation, urinary retention, and drowsiness. For this purpose, the following were studied: sublingual atropine [28], sublingual ipratropine bromide spray [29], oral glycopyrrolate [30], and oral tropical tropamide [31]. Current MDS guidelines for the use of anticholinergic drugs for the treatment of drooling in PD indicate that glycopyrrolate is effective, but proven efficacy lasts for 1 week and there is insufficient information on its tolerability. There is also insufficient information on the effectiveness and tolerability of ipratropine.
Adrenergic receptor agonists
may partially reduce sialorrhea. Clozapine, yohimbine, and α2-adrenergic receptor antagonists have been reported in the literature as having drooling as a side effect. Based on this, α-2-adrenergic receptor agonists should reduce salivation. Specifically, clonidine reduced sialorrhea in a small, randomized, double-blind, placebo-controlled trial of 32 patients [32]. Oral modafinil 100 mg daily also reduces drooling. However, modafinil is an α-1-adrenergic receptor agonist, and the reduction in sialorrhea is most likely due to a reduction in dysphagia rather than suppression of salivary production [32]. Thus, there are currently no recommendations for the use of α2-adrenergic receptor agonists in the treatment of hypersalivation, but clonidine and modafinil may be considered promising agents.
Botulinum therapy
The main mechanism of action of BTX is inhibition of acetylcholine release. Local injections into the salivary glands inhibit cholinergic parasympathetic and postganglionic sympathetic activity, causing a decrease in salivary secretion. Two serotypes of BTX are being studied to reduce sialorrhea: serotype A and serotype B. Two types of BTX type A, onabotulinumtoxin and abobotulinumtoxin, are used in the treatment of sialorrhea.
Studies have been conducted to study onabotulinumtoxin of various designs (observational, open, open case-control, randomized placebo-controlled) [33-38]. In all of these studies, injections were made into the parotid gland. One of them [37] included patients not only with PD, but also with multiple system atrophy and dementia with Lewy bodies. Two studies [33, 36] used ultrasound guidance. One study [33] showed no difference in the effectiveness of injections with and without ultrasound guidance. The therapeutic effect was assessed after 1–16 weeks. BTX was administered in doses of 5 to 50 units into the parotid gland and 5 units into the submandibular gland with a significant reduction in salivation and a duration of effect of up to 4 months.
Abobotulinum toxin (Dysport) was injected into the parotid gland in all studies. In some of them [39], BTX was additionally injected into the submandibular salivary gland. Most studies did not use additional injection control methods. Only two of them [39, 40] used ultrasound guidance. The duration of outcome assessment ranged from 1 to 4 weeks. All studies demonstrated the effectiveness of abobotulinumtoxin in doses of 75-146.2 units when injected into each parotid gland and 78.7 units into each submandibular salivary gland. Salivation was significantly reduced in patients not only with PD, but also with multiple system atrophy, corticobasal degeneration, and amyotrophic lateral sclerosis [41]. Both according to objective assessment methods and according to the subjective feelings of patients, the therapeutic effect persisted for 1-4 months. Additionally, it was found that there are no significant differences in therapeutic effects between injections of the drug into the parotid or submandibular glands [26].
BTX type B (rimabotulinumtoxin, not registered in Russia) was also injected mainly into the parotid salivary gland [42–47], two studies used ultrasound guidance [31, 45]. All studies demonstrated the effectiveness of BTX type B in doses of 500-2000 and 250 units when injected into the parotid and submandibular glands, respectively, with an average duration of effect of 4.8 months.
The objective of one of the studies was to compare BTX types B and A (randomized, placebo-controlled, crossover, ultrasound-guided) [48]. Either 100 units of abobotulinumtoxin or 1000 units of rimabotulinumtoxin were injected into the parotid gland; either 25 units of abobotulinumtoxin or 250 units of rimabotulinumtoxin were injected into the submandibular gland. When assessing salivation using the DSFS (Drooling Severity Scale and Frequency Scale) and DRS (Drooling Rating Scale) methods 1 month after the injection, the result was better in the group that received BTX type B, but after 2 months the results were equal.
According to MDS recommendations, BTX are effective in the symptomatic treatment of sialorrhea in PD [49]. The therapeutic effect begins 1 week after the injection and lasts 3-5 months. Ultrasound-guided injections may be more accurate. There were no differences in the effectiveness of BTX types A and B. Typical side effects such as dry mouth are mild.
Pharyngeal-cricoid dysphagia can also be successfully compensated with BTX injections. Several injection techniques have been described, including both percutaneous and endoscopic techniques [50, 51]. Administration of BTX type A 30 IU for dysphagia into the pharyngo-cricoid muscle under the control of electromyography and esophagoscopy leads to a decrease in swallowing disorders after 48 hours: swallowing function improves, hyperactivity of the pharyngo-cricoid muscle decreases according to electromyography [52]. Dysphagia usually returns 22 weeks after injection. During these weeks of swallowing improvement, patients regain lost body weight [51, 53]. This fact is important in improving the quality of life of patients.
Non-pharmacological treatments
Various non-pharmacological treatments are offered, such as chewing gum, behavior modification, radiation therapy, and surgical methods. However, only 2 studies on this topic have been published. L. Marks et al. [54] conducted a randomized placebo-controlled trial in 6 patients with PD. Patients were required to voluntarily swallow each time they heard a sound. This modified behavior resulted in a significant reduction in sialorrhea as assessed by DRS. At the same time, the results that reached their maximum 1 month after training turned out to be minimal after 3 months. The authors concluded that patient motivation and voluntary control of swallowing should be considered and used in the treatment of patients with sialorrhea.
Another study used bilateral 12 Gy radiotherapy to the parotid and superior submandibular glands [5]. Hypersalivation decreased significantly after 1 month after radiotherapy, and the effect persisted for up to 1 year. The most common adverse events were decreased taste and dry mouth. However, 75% of adverse events were transient.
We have not found any studies in the literature regarding the effect of surgical neuromodulation. It is possible that in some cases, when chronic stimulation of the basal ganglia causes deterioration in swallowing, drooling may increase [56]. A recent study [57] showed an adverse effect of bilateral stimulation of the subthalamic nucleus.
The bottom line is that there are no current recommendations for the use of non-pharmacological methods in the treatment of sialorrhea in BP. However, behavior modification and, in refractory cases, radiotherapy can be considered as additional components of the overall treatment package.
In conclusion, drooling has negative consequences on the lives of both patients with PD and their caregivers. While the leading role in sialorrhea is probably not overproduction of saliva, but swallowing disorders, most treatment methods are aimed at reducing secretion. Currently, injections of botulinum toxins into the major salivary glands are the most effective treatment. The pathophysiology of ptyalism, standardization of diagnostic criteria, methods for assessing severity, and development of treatment strategies for sialorrhea in PD require further study.
Excess saliva, or how to prevent it
By and large, there are three types of therapy that are used to treat increased salivation. These include Botox injections, surgical treatment and medications that are available only by prescription. It all depends on the factors that caused the disease. It is clear that the simplest thing will be to prescribe certain medications. Typically, the above drugs will include scopolamine and glycopyrrolate. Side effects include increased heart rate, trouble urinating, drowsiness, and blurred vision.
For severe forms of drooling, specialists resort to Botox injections into the salivary glands (one or more). The treatment is considered safe, but its effect only lasts for several months. And only in very severe cases do doctors resort to surgery. During surgery, the salivary glands are removed or the direction of the excretory ducts is changed.
With the help of surgery, you can permanently get rid of increased salivation. Salivary glands – increased salivation and dry mouth
Hypersalivation, treatment
To successfully eliminate hypersalivation, treatment must begin with a search for the true cause of the pathology - only an accurate diagnosis will allow one to prescribe effective methods of therapy. In the case where high salivation is caused by diseases of the oral cavity, treatment by a dentist will be necessary: examination and sanitation of the oral cavity, anti-inflammatory therapy.
If the pathology is caused by disturbances in the functioning of other systems (digestive, nervous, endocrine), joint supervision of the dentist and related specialists - gastroenterologist, endocrinologist, neurologist will be required. In any case, even if the problem is caused by some kind of systemic failure in the body, successful therapy will require high-quality sanitation of the oral cavity with the elimination of all infectious and inflammatory foci.
In some cases, hypersalivation is treated with drugs that reduce salivation. You can take such drugs only on the recommendation and under the supervision of a doctor; moreover, you need to remember that sometimes they cause unwanted side reactions. In addition, the doctor may prescribe physiotherapeutic procedures, massage and facial gymnastics, rinsing - all these methods are usually used in combination. In particularly difficult situations, surgical intervention to remove large salivary glands is possible, but surgical treatment is used only as a last resort.
First aid for nausea
Painful sensations in the stomach disrupt the usual rhythm of life, you want to be free from discomfort. To help yourself deal with this, try these tips:
- Take a horizontal position - lying down, a person feels better, especially important for dizziness;
- Wash with cool water;
- It is worth limiting physical activity, it is advisable to maintain complete rest;
- Ventilate the room, fresh air will help improve your well-being;
- Rinse your mouth after vomiting;
- Eat healthy foods (fruits, vegetables, dietary meat);
- Eat often, in small portions, plenty of fluid intake is important (salty, spicy, iron-containing foods are not allowed);
- Drink a glass of water with lemon;
- Try to restore your breathing and relax;
- Turn on calm music, your favorite movie. It is important to calm the nervous system;
- Take antiemetics at night;
- If you have problems with stool, take prebiotics.
As soon as the nausea subsides, see your doctor to determine the cause. Pay close attention to changes in how you feel.
Diseases that cause symptoms
There are a number of diseases that cause these unpleasant symptoms: hypersalivation and nausea. To get rid of them, you need to undergo a course of treatment.
Epidemic encephalitis
The virus that causes this disease has not yet been identified. At first, patients complain of weakness, headache, and fever. After 2 weeks, sleep is disturbed, the patient falls asleep in any place, even in uncomfortable positions, at times it alternates with insomnia. Vision deteriorates and squint may appear. Patients complain of dizziness, nausea, and vomiting.
This disease is not easy to diagnose and is difficult to treat. Antiviral and detoxification therapy should be carried out.
Stomach ulcer
The mucous membrane becomes covered with defects. The causes are stress, poor diet, taking gastrotoxic drugs, diseases of internal organs and systems. Symptoms: pain on an empty stomach, disappears after eating, heartburn, vomiting, which brings relief, hypersalivation, feeling of heaviness after eating.
Gastroscopy can confirm the diagnosis. Treatment is carried out by a gastroenterologist, who prescribes a strict diet and drug therapy.
Worm infestation
This is a helminth infection. They cause intoxication and tissue damage, take away some of the nutrients, thereby weakening the body and reducing immunity. Symptoms: sudden weight loss with the same diet, abdominal pain, flatulence, nausea, vomiting, increased salivation, skin rash and itching, weakness, grinding teeth in sleep. Treatment is taking drugs that destroy parasites. Contact a gastroenterologist or parasitologist.
Consequences of radiation therapy
When treating malignant brain tumors, nausea may occur, which continues to bother you several weeks after completion of treatment. To cope with it, the oncologist prescribes antiemetic drugs, which must be taken half an hour before the procedure. At this time, it is better to avoid fatty and fried foods with a strong smell, you need to eat little and often, and drink more. If the salivary glands are also irradiated, increased salivation may occur. This symptom will go away after treatment is completed.
Diagnosis and treatment of toxicosis
Even with mild manifestations of toxicosis, the doctor will refer you for tests. You will need to undergo a urine test for acetone and ketone bodies, biochemical and general blood tests. In case of severe disease, the patient will be admitted to a hospital. For mild, the most common degree of toxicosis, you will be treated at home under the supervision of a antenatal clinic doctor.
To eliminate discomfort, you need to pay attention to diet . With toxicosis, appetite is not always impaired, sometimes it is even increased, but more often than not even the sight of food does not evoke positive emotions, and sometimes you have to make significant efforts to force yourself to swallow even a piece. Therefore, you can satisfy your culinary whims by introducing coveted pickles, sweet buns or exotic fruits into your diet. Food should be taken frequently, 5-6 times a day, but the portions should be small and the menu varied.
It should be borne in mind that very hot or very cold food will more quickly provoke vomiting. Products should be easily digestible and contain sufficient amounts of vitamins. It is better to drink mineral alkaline water and mint tea.
If you notice that the secretion of saliva is significantly increased , rinsing your mouth with tanning solutions that reduce this process, for example, infusions of sage, chamomile, and mint, will help you. If nausea and vomiting occur in the morning, immediately after waking up, try having breakfast in bed, placing a few crackers, lemon slices or mint gum next to the bed. It’s especially nice if in this situation the future dad shows himself to be a gentleman and serves you a light and healthy breakfast.
If nausea begins in the afternoon , then most likely it is due to nervous tension and fatigue. In this case, you can drink a soothing tea, motherwort or valerian.
If these measures do not help, be sure to inform your obstetrician-gynecologist.