3D CT – what is this procedure and what is it for?
3D imaging of the jaw is one of the main dental procedures used in diagnosis. The data obtained allows us to assess the condition of a specific maxillofacial area and plan further treatment.
This diagnostic tool is universal; it is used by both therapists and orthopedists, periodontists and implantologists. Using a 3D image, the therapist assesses the condition of the roots and canals of the tooth, and clarifies the localization of the inflammatory process.
An orthopedist can examine the anatomical structure of the temporomandibular joints, an implantologist can examine the volume and density of bone tissue in the area of the upcoming operation, as well as the parameters of the maxillary sinuses (maxillary sinuses).
Sometimes a large part of the tooth remains, as they say, “behind the scenes”, and the dentist simply cannot see it. Then computed tomography comes to the rescue, which allows you to examine the hidden area and prevent unpleasant consequences for the patient.
Until recently, the “gold standard” for instrumental diagnostics was a panoramic image. Today there is a more advanced method in which the maxillofacial area is scanned using computer technology.
Read also
What is dental restoration
If the aesthetic properties of teeth are lost, a person experiences certain discomfort.
What to do if your tooth aches
Sometimes aching pain in a tooth can appear for no apparent reason at first glance.
Unique visualization method
A computed tomograph produces a high-quality three-dimensional image of an individual tooth, maxillary sinuses, one or both jaws. Unlike standard panoramic images, a 3D tomogram allows the doctor to see the desired anatomical structures in a virtual section, from any angle.
During the procedure, the doctor can enlarge, rotate and study the maxillofacial area of interest at the required angle, which is unrealistic with conventional radiography.
Computed tomography is an integral and primary stage of examination before implantation. It allows you not only to assess the condition of bone tissue, but also to measure its height, width and density. Moreover, three-dimensional beams help to choose the optimal method for installing implants through preliminary virtual surgery.
3D CT is a multi-purpose and indispensable diagnostic tool that makes it possible to avoid many medical errors and complications. Thanks to this examination, the quality of treatment increases significantly and eliminates unnecessary traumatic operations.
Computed tomography in endodontics: a model of modern treatment
Radiography is an important aspect of successful diagnosis of odontogenic and non-odontogenic pathology, treatment of the pulp chamber and root canals through coronal access, biomechanical treatment of root canals, final canal obturation and evaluation of the treatment performed. Images are required throughout the endodontic treatment. Obtaining an image before the intervention is required for a correct assessment of the hard tissues of the tooth and alveolar process, as well as the degree of pathological damage and making the correct diagnosis. Further, obtaining images throughout the treatment is also necessary. Taking an image at the end of treatment allows you to evaluate the manipulations performed. Kells first reported the use of a conductive conductor in the root canal in a "radiograph" in 1899.
Since then, radiology has always played a key role in endodontics. Now, a century later, early efforts have led to the invention of computed tomography (CT) and micro-CT, and the introduction in 1996 of cone beam computed tomography (CBCT) provided the 3D images needed in dental practice.
This new 3D imaging capability has significantly improved the standard of dental treatment around the world. CBCT is gradually becoming the gold standard in providing accurate diagnosis, treatment planning and treatment. Cone beam technology currently has many applications in dentistry, including implant planning, surgical pathology assessment, TMJ assessment, growth and development detection for orthodontic purposes, pre-operative, operative and post-operative assessment for craniofacial trauma, craniofacial reconstruction and oral surgery. . In addition, CBCT is used to identify the exact location of the foreign body in the soft tissue, identifying cleft lip and palate, and the depth of the carious lesion. CBCT is becoming a typical tool in the work of a surgeon, especially an implantologist.
Limitations of 2D Images
The image obtained with a conventional radiograph is a two-dimensional (2D) interpretation of a three-dimensional (3D) object. Characteristics of a 3D object, such as complex dental anatomy and surrounding tissue structure, may be difficult to discern as “shadows” in a 2D image, which can lead to inappropriate endodontic treatment. When analyzing a 2D image, all images are interpreted very freely, introducing an aspect of subjectivity. Limitations of dental radiography may also be due to radiologist error. Any inaccuracies in image acquisition, ranging from incorrect angulation to incorrect configuration of the tooth in relation to the sensor, can lead to errors in the interpretation of the images. Such images of poor quality have artifacts and contribute to incorrect diagnosis. Many researchers, including Goldman, have confirmed the low correlation (47%) among all specialists treating periapical pathology using dental radiography.
Cone beam computed tomography
CBCT has been used in dentistry since 1981. Unlike a regular CT scan, which creates an image in different layers, CBCT creates an image in 3D pixels called voxels. Since these voxels are isotropic, the object is carefully measured in different directions. This allows you to visualize a geometrically undistorted image of the maxillofacial area, which can be viewed from different angles. In addition, to provide high image resolution, CBCT is available for viewing from different viewpoints (FOV) for use in a variety of situations. In endodontics, an apparatus with a limited FOV is usually sufficient. Typically, the smaller the scan volume, the higher the spatial resolution of the image. Since an early symptom of periapical pathology is discontinuity of the lamina dura and widening of the periodontal fissure, the optimal resolution for CBCT imaging used in endodontics should not exceed 200 nm - the average width of the periodontal space. 3D Accuitomo (K Morita, Corporation, Kyoto, Japan) - the first of the small FOV systems - provides a resolution of 0.125 mm. Orthophos XG3D (Sirons Germany) also provides a 5*5 FOV specifically for endodontic purposes.
CBCT produces much less radiation exposure than conventional CT. The exposure dose when performing digital radiography is comparable to taking conventional diagnostic panoramic or targeted images. Acquiring images for the entire mouth is irradiated at approximately 150 usv. It is obvious that a high-resolution CBCT scan of one tooth, used in the diagnostic process, replaces 3 targeted images. It is difficult to imagine that exposure dose could be more important than obtaining CBCT in a prudent manner to obtain information that is simply not available with other instruments.
CBCT in endodontics
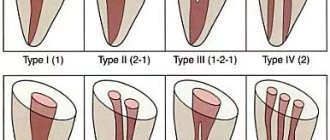
1. Assessment of root canal morphology
The success of endodontic treatment depends on locating all root canals and then evaluating, cleaning, debridement and obturation. The frequency of occurrence of the second mesiobuccal canal (MB2) in maxillary first molars varies from 69% to 93% depending on the chosen method of examination. This variability occurs in the buccolingual plane, where overlapping anatomical structures prevent the identification of structures with small differences in shadow density. Conventional radiography, at best, can only detect 55% of these configurations.
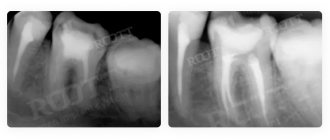
Ramamurthy and Matherene describe the limitations of 2D imaging for identifying MB2 channels (Figure 1).
Photo 1: MB2 image in both first molars
A study conducted by Neelkantan in Indian population found that MB2 canal is most common in the first maxillary molar compared to the second. Also, anatomical type IV canal is more common than in the Mongoloid population.
Baratto Filho examined the internal morphology of extracted maxillary first molars, comparing them with microscopic examination and ex vivo CBCT imaging. Reports showed the presence of 4 canals in 67.14% of teeth and additional root canals in 92.85% of cases in the mesiobuccal root. Clinical evaluation showed a slightly reduced overall rate (53.26%) but an increased detection rate of MB2 (95.63%), while CBCT showed 37.05%. The scientists concluded that CBCT is a good method for the initial assessment of the internal morphology of the upper first molar, but for identifying the orifices, the use of a microscope is the best method. CBCT has also been used to identify the high incidence of distolingual canal in Taiwanese, identify abnormalities in the root canal system of mandibular premolars, and help identify root deviation (Figure 2).
Figure 2: Axial view of C-shaped canals in second molars
With the invention of the new CBCT software Orthophps CG3D/Galelios (Sirona, Germany), the working length of the canals also became feasible. But the accuracy of these data in clinical work has yet to be confirmed (Photo 3).
Photo 3: Tool for measuring the length of the root canal
2. Pathologies in periapical tissues
The most common pathological condition affecting teeth is inflammation of the pulp and periapical areas. CBCT technology now provides the clinician with the ability to view the desired area in three different planes, thereby obtaining 3D information. Lesions contained in cancellous bone with little or no cortical plate may be difficult to diagnose on plain film. Lofthag-Hansen, Stavropoulos, and Wenzel compared the accuracy of limited-FOV CBCT with conventional imaging.
The researchers reported that CBCT provided more accurate diagnostic data (61%) compared with digital (39%) and conventional (44%) radiographs. But although CBCT data is more accurate, researchers are not calling for the complete replacement of conventional intraoral radiography for detecting periapical changes in routine clinical practice due to financial and harmful components. Estrela et al proposed the use of CBCT-based periapical indices to identify pathologies (Figures 4-6).
Figure 4: Periapical cyst in the anterior segment of the mandible A: 3D view showing a large cystic cavity B: Sectional view showing loss of cortical plate C: Axial view showing loss of cortical plate on the labial side and intact plate on the lingual side.
Figure 5: Chronic periapical abscesses around the right mandibular first molar
Photo 6: Periodontal lesions near the upper left second molar
The CBCT index system consists of 6 grades (0-5) based on determining the largest lesion size in any dimension and taking into account the expansion and destruction of cortical bone.
Using this index, Low came to the conclusion that it is better to use CBCT weeks or conventional radiography to detect periapical pathologies.
Shadow gradient CBCT can help in the differential diagnosis of cyst and granuloma. In general, the ability to detect pathologies of CBCT is as good as that of plain CT. This method can be important for patients who present with pain or poorly localized complaints in the area of previously treated or untreated teeth, where pathology is not detected on a regular x-ray.
3. Root fractures
The usefulness and importance of CBCT in the diagnosis and management of dentoalveolar trauma, especially root fractures, luxation, displacement and alveolar bone fracture, have been extensively studied.
CBCT has found application specifically in the diagnosis of tooth root fractures.
(Photo 7,8) The high importance of CBCT in identifying vertical and horizontal root fractures has also been described in the literature. Elimination of superimposed anatomical structures allows the clinician to clearly analyze the fracture. In addition, 3D reconstruction can be performed on both the dentofacial system and the alveolar bone.
Figure 7: Root fracture in an endodontically treated upper right second molar A: OPG showing previously treated canals of an upper right first molar B: Axial image showing the fracture line along the palatal root C: Sectional view showing the oblique fracture line of the palatal root
Figure 8: Horizontal fracture of the right upper central molar A: 3D image showing the fracture line at the junction of the middle and apical third of the root B: Axial image showing the horizontal fracture line in the anterior aspect of the upper right central incisor C: Oblique fracture line extending from the mesial carp central incisor on a sectional photograph.
4. Root resorption
Root resorption is the loss of hard tooth tissue as a result of osteoclast activity. This may occur as part of a physiological or pathological process. Root resorption can be classified into external and internal, depending on the location of the process relative to the root surface. The first data on internal resorption were obtained in 1830. In comparison with external resorption, internal resorption is a very rare process, the etiology of which is not fully understood. The accuracy of CBCT in determining surface defects, although higher than that of standard techniques, is still not ideal and increases with increasing voxel resolution of the image. CBCT has also been shown to be useful in assessing post-orthodontic apical resorption, in particular the roots of the maxillary lateral incisors in impacted canines.
On CBCT, external resorption appears as uneven radiolucency and an intact tooth canal, while internal resorption appears as a clear focus without tracing the root canal.
CBCT has been successfully used to determine internal resorption and differentiate it from external resorption. Conventional radiography often cannot reveal the correct extent of distribution, localization and source of the resorptive process. CBCT helps in determining treatment tactics, and also offers an accurate prognosis based on the activity and extent of the lesion. Both the treatment and the treatment outcome become more predictable in this way.
5. Postoperative assessment
Monitoring the healing process of apical lesions is an important aspect in the postoperative phase of endodontics. Also, adequate root canal obturation is an important determinant of endodontic success. It can be stated that CBCT is very useful both in starting treatment and in monitoring the subsequent condition of the tooth. Sogur reports that images obtained from conventional X-rays in the postoperative period are more informative than CBCT. The scientist explains this fact by the presence of a large number of artifacts in CBCT images, caused by the presence of gutta-percha and sealer in the canals (Photo 9).
Photo 9: Artifacts of obstructed root canals
The use of CBCT in determining the exact location of the perforation and its role in the subsequent treatment plan is illustrated by Young (Figure 10).
Figure 10: Root perforation clearly visible on axial image
Preoperative assessment of periapical tissues is an important step to prevent complications. The close location of the apex to the mandibular canal, mental foramen and maxillary sinus can be assessed specifically on CBCT images. Rigolone was the first to describe the importance of CBCT for endodontic intervention planning.
The importance of CBCT for apical surgery of teeth close to the maxillary sinus was consistently demonstrated by Nakata, who demonstrated a clinical case of periradicular pathology localized to a specific root. Tsurumachi and Honda described the use of CBCT in locating an endodontic instrument fragment that had entered the maxillary sinus.
Conclusion
Despite the obvious advantages of CBCT technology in dentistry, there are also some disadvantages and limitations. CBCT technology is not currently widely available. Gradually, with the introduction and mastery of specialists, CBCT will become a more common diagnostic method. Although this technique has been on the market for several years, it continues to be expensive. For most endodontic procedures, only a small FOV of 4*4 mm is sufficient.
Limiting the FOV not only reduces radiation dose, scan time and artifacts, but also focuses on structures that are familiar to dentists. What is expected in the future regarding endodontics to CBCT? It is not known whether dentists will want to purchase the device themselves or receive images from a special radiologist from the center. One thing is clear: more and more dentists are introducing CBCT into their practices.
Author: Sushma Prashant Jaju , BDS, MDS Operative Dentistry and Endodontics, Dentocare multispecialty Dental Clinic, Nashik, Maharashtra, India
Indications
Computed tomography is prescribed to identify:
- hidden carious lesions;
- defects in the structure of the jaw and dentition;
- fully or partially unerupted teeth;
- dystopic dental units with incorrect location or direction of growth;
- supernumerary teeth;
- damage to the dentition due to jaw fractures and other injuries;
- pathologies of the temporomandibular joint TMJ;
- tumors, cysts and other neoplasms in the jaws;
- condition of periodontal and periodontal tissues in case of gum disease, inflammation in the root area;
- number of roots, canals of teeth;
- cracks in the roots of teeth;
- features of the structure of bone tissue before jaw surgery (installation of implants, bone augmentation).
A 3D photo must be taken before dental implantation. The fact is that the jaw bone is clearly visible on a regular x-ray, but it does not allow assessing the soft tissues. On a three-dimensional tomogram, you can see in detail not only the bone, but also the nerve of the lower jaw, as well as blood vessels.
A 3D tomogram is much more informative than a panoramic image or targeted photographs of all teeth.
Is special training needed?
The preparatory stage includes an initial consultation with a dentist, who conducts a survey to identify possible contraindications. Further preparation depends on what type of research needs to be carried out:
- Normal (without contrast injection). Such a CT scan will not require additional preparation, except for the general requirements: it is recommended to remove all metal objects from the head - earrings, hairpins, etc. if present, remove the hearing aid and removable dentures; warn the radiologist if there are non-removable orthopedic structures in the mouth (this will allow the specialist to adjust the device in a special way).
The lack of serious preparation before taking a CT scan of two jaws or teeth allows diagnostic studies to be carried out immediately after receiving an order from a doctor.
CT scan before implantation
Diagnostics using a computed tomograph before installing implants allows, first of all, to determine whether implantation is necessary at all. The image will give a complete picture, and the doctor will see where the teeth are missing, whether there are problem units, and whether they can be cured.
The 3D tomogram will show:
- hidden carious cavities;
- unerupted and “extra” teeth, which may interfere with the installation of artificial pins;
- properties of roots, canals - curved, narrow and long canals require a special approach, which should be taken into account before implantation;
- bone dimensions in height and width, on the basis of which the type and size of the implant is selected;
- condition of bone beams, partitions, voids in the jaw bone;
- the presence of inflammatory processes in the root area - cysts, granulomas, abscesses where implants are planned to be installed. All this needs to be treated or removed before surgery;
- inflammation in the paranasal sinuses and lacrimal ducts, which can become a temporary obstacle to implantation;
- density, size, inclination of the alveolar process, thickness of the cortical bone layer, taking into account which the optimal type of artificial pin is selected;
- the physiological structure of the maxillary sinuses, the mandibular canal to determine the angle of inclination of the implant rod;
- defects and anomalies in the structure of the dentofacial apparatus;
- quality of installation, strength of fixation of implants after surgery for their implantation;
- severity and nature of traumatic injuries in fractures.
Based on the results obtained, a virtual operation to install the rods is performed. The appropriate size of the titanium pin is selected, its inclination and the point of implantation are determined, bypassing the anatomical structures. Thus, the final outcome of implantation is modeled.
Next, the tomographic data is loaded into the computer, and the program creates a three-dimensional model. The patient’s personal surgical template is printed on a 3D printer - an overlay with guide holes for inserting rods.
During implantation, the template is placed tightly on the gums, and the placement of the pins is carried out with extreme precision.
How long does it take to do a CT scan?
The duration of tomography depends on the type of diagnostic equipment used. Before doing a CT scan of the jaw and teeth, it is better to ask what kind of tomograph is used in the clinic. Modern devices allow you to carry out the necessary manipulations as quickly as possible with minimal radiation. If you are offered a procedure that will last more than 15 minutes, then you should refuse. Only innovative equipment allows you to carry out the required research in just a few minutes, guaranteeing highly detailed images.
On average, everything is done in no more than 10 minutes, taking into account the instruction time and the preparatory stage. Please note that 3Shape is also used for 3D diagnostics, but this intraoral scanner is not suitable for all types of diagnostic studies. The attending physician will be able to determine which scan is required for you after collecting a general clinical picture and based on the reason why you came to the dentist.
Multispiral or cone beam?
A multispiral tomograph performs layer-by-layer scanning of an object along a spiral trajectory caused by the continuous movement of the table and the X-ray tube relative to each other.
Most often, MSCT - multislice computed tomography - is used in maxillofacial surgery for facial injuries and pathologies of the temporomandibular joint.
In dental practice, especially when planning implantation, this method is not widely used due to insufficient data accuracy. Since the patient lies down during the examination, the jaw connection is distorted.
In addition, the radiation level of MSCT can reach 1000 μSv, which is unacceptable, since implantological treatment involves more than one procedure over several months.
Cone beam CBCT is a more modern, accurate and safe method compared to MSCT. Its radiation exposure is less, about 25-50 μSv, which makes it possible to carry out the procedure several times a year.
Contraindications for examination
Research is not recommended if:
- you are overweight;
- you have an exacerbation of pain;
- restlessness is brought to the point of hyperkinesis (uncontrolled movements);
- the period of bearing a child is underway;
- there is an allergy to iodine;
- there is renal failure.
How often can a CT scan of the jaw be done?
Computed tomography is based on the already familiar X-ray radiation. It would seem that in this case it should be carried out quite rarely, for fear of tangible consequences for health. However, this is not true: the tomograph itself is built differently than an x-ray, which helps keep the radiation dose to a minimum. Therefore, you should not expect any irreversible consequences even with repeated use of this technique.
3D CT or panoramic image?
An orthopantomogram allows the doctor to assess the condition of the teeth, root canals, and soft tissues. With its help, hidden inflammations, abscesses and abnormally located teeth are revealed.
However, a panoramic photo does not give a 100% accurate picture; the error is about 20%. Even a slight shift causes the focal spot to shift, and the image is compressed or stretched.
Due to the difference in the refraction of X-rays by tissues of different densities, it is impossible to assess the properties of the cancellous bone layer, since it is simply not visible behind the denser periodontium.
A two-dimensional orthopantomogram is, in fact, an auxiliary technique that gives a general idea of the condition of the oral cavity and identifies mainly obvious pathologies. It does not show the configuration and structure of the alveolar process at the desired level.
The advantage of a three-dimensional 3D tomogram is that it produces not one flat photo, but several consecutive images from different angles.
The doctor sees and evaluates all necessary objects located at any depth, from all sides and at different angles.
Preparatory stage
CT scan of the upper and lower jaw according to the basic (native) protocol does not require special preparation. If a CT scan of the jaw with contrast is prescribed, the diagnosis is usually carried out with a break in food for 2 hours. If the patient suffers from renal failure, tests to determine the level of creatinine in the blood are preliminarily prescribed before contrast tomography. This way, the doctor can assess the possible risks of developing nephropathy after administration of a contrast agent. Before entering the CT room, it is better to change into comfortable clothes and remove all jewelry.
How to make a 3D tomogram
Usually the procedure is performed standing, the patient bites a small flat plate with his teeth and stands without moving for 15 to 30 seconds. The device makes several rotations around the head, managing to take about two hundred pictures in various projections.
In 10-15 minutes, the information is processed and transferred to electronic media.
We invite you to make a three-dimensional tomogram in our clinic using the latest generation dental tomograph. Sign up for the procedure online or by phone at a time convenient for you.
How is a CT scan of teeth and two jaws done?
After the preparatory stage described above, the procedure itself begins with a short instruction - the radiologist explains how and why it is necessary to remain still while the device is operating. After this, the CT scan proceeds as follows:
- if necessary, a contrast agent is introduced at this stage;
- The patient wears a vest with a lead layer, which will provide additional protection to the chest area from radiation;
- depending on the type of scanning equipment used, the patient is asked to stand or sit near the tomograph;
- the radiologist fixes the patient’s head with special supports provided in the tomograph (fixation is carried out in the frontal, temporal and chin parts), and the hands are asked to be placed comfortably on the handrails;
- the specialist starts the equipment and the sensor, which takes and transmits 3D images, begins to rotate around the head (in one revolution, the sensor takes 150-200 high-resolution 2D images, after which it converts them into a three-dimensional picture);
- the sensors take readings for no more than 30 seconds and to obtain the highest quality results and accurate images, it is recommended to remain motionless during this time;
- The radiologist releases the patient's head from fixation on the supports and this is where the procedure ends.
Next, it will take a few minutes for the device to process the scanned data and write it to disk. You may be interested and useful to know - in the article “CT of the jaw for dental implantation” we talk in detail about the features of tomographic studies before implanting artificial roots.
You might be interested in:
Dental diagnostics
Computed tomography of teeth and jaws
X-ray of teeth
3D image of teeth