Osteosynthesis of the jaw is a method of surgical treatment of bone fractures using special, most often metal, structures. Osteosynthesis surgery is performed if the fracture site cannot be secured with splints, and also when it is difficult to fix bone fragments. There are different methods of performing the operation, they can be used depending on the type of injury and its severity.
Osteosynthesis allows you to maintain the required level of blood circulation in the damaged bone, which means that such a fracture will heal faster. Not only the integrity of the bone is restored, but also its structure, and this will take only a few weeks.
During the rehabilitation period, it is important to follow certain rules and monitor your well-being and the condition of your bone tissue. Violations of doctor's instructions can lead to pain and even loss of chewing functions.
Indications for osteosynthesis
Osteosynthesis may be prescribed in the following cases:
- if there are not enough stable molars at the fracture sites;
- upon impact, the fragments moved significantly;
- broken jaw bone behind teeth. With such an injury, individual parts of the bone tissue are displaced;
- the injury occurred as a result of the development of inflammatory diseases that thin the bone tissue;
- in case of a fracture of the lower jaw, if too small or massive fragments have formed;
- if the branches and body of the jaw are incorrectly positioned relative to each other;
- it is necessary to perform reconstructive surgery or osteoplasty.
Microsurgical operations of maxillofacial surgery
Microsurgery is a universal method used in almost all surgical disciplines to eliminate a defect in a particular tissue. In the human body, there are more than 400 donor sites with an axial type of blood supply, from which taking tissue does not cause any harm to the further blood supply of the entire organ. In the reconstruction of the jaws, the main place is played by the property of the flap with the presence of such a quantity and quality of bone that will make it possible to recreate the anatomical integrity of hard tissues and in the future the possibility of use for dental implantation and prosthetics .
For total and subtotal defects of the mandible, a fibular skin-bone flap . The fibula has sufficiently large supporting properties, having a fairly large amount of cortical component, and can be easily modeled to recreate anatomical contours. An iliac or otherwise inguinal skin-bone flap is optimal for the reconstruction of small defects of the lower jaw; in the latter cases, it is sometimes possible to use a free iliac bone.
For total and subtotal defects of the upper jaw, radial skin-bone and fibular skin-bone flaps are optimal. In cases where the defect covers the zygomaticomaxillary buttress in combination with a defect in the alveolar process, it is possible to fill the bone defect with corticocancellous parietal grafts and mandibular grafts taken from the ramus and mental region with free grafts of mesenchymal origin, which is optimal for reconstruction of the middle zone faces.
Of course, the dominant algorithm remains aimed at engrafting the flap on a vascular pedicle. If you have to choose between convenience for subsequent dental implantation in the form of the presence of a cortical plate of the bone component of the autograft in the area of the recreated alveolar process for subsequent implantation and this somehow reduces the reliability of the vascular anastomosis, it is necessary to choose the reliability of engraftment. Disputes often arise between implant surgeons and reconstructive surgeons about how the iliac bone should be positioned in the defect area, but experience shows that there can be no compromises, since in case of thrombosis of the vascular anastomosis, the entire flap is lost. It is also necessary to understand that the location of the spongy component in the area of the alveolar process does not interfere with subsequent implantation, since a new one is formed within 6 months.
To return and normalize chewing function and the ability to eat, it is necessary to have:
- 1. Lips and complex of swallowing organs.
- 2. Presence of jaws.
- 3. The presence of teeth and a bite that provides adequate chewing.
- 4. Presence of buttresses.
- 5. Stabilization of the TMJ.
- 6. Synchronicity of the masticatory muscles.
- 7. Mental balance of the patient.
In the literature, we did not find a specific algorithm or approaches aimed at returning such vital abilities as sucking and swallowing, chewing and normalization of speech function. To normalize the patient's nutrition, the presence of lips is necessary, otherwise salivation occurs, followed by maceration of the skin and the inability to receive and send food into the esophagus. Patients with defects of the soft tissues of the perioral area constantly suffer from gastritis, inflammation of the oropharynx, since the vacuum property of food evacuation into the esophagus is reduced, many adapt to swallow with an open mouth, throwing their head back; in the latter, the absorption of carbohydrates is impaired, since saliva takes part in cleansing the oral cavity from food residues, plaque and bacteria, thanks to its buffering properties, it neutralizes the negative effects of strong acids and alkalis within the buffer capacity, provides the supply of ions necessary for the remineralization of teeth, and has antibacterial, antifungal and antiviral properties. Claude Bernard proved that we recognize the functions of an organ by identifying the consequences of its absence. From the point of view of the functional return of the ability to eat, the second place in our algorithm is the presence of jaws. To eliminate defects in part or the entire jaw, we use preoperative planning.
Preoperative planning of the jaws is carried out using 3D visualization programs that allow modeling the sizes and shapes of autografts, taking into account the positioning of the condylar processes of the lower jaw in the temporal fossae (in the anterior-superior position in the articular cavities) according to CT scans. Despite the fact that we perform reconstruction in the previous bite, most often we have to deal with an already remodeled TMJ and a broken bite. Therefore, planning is necessary taking into account the subsequent achievement of centric occlusion in the centric relation. A functional study of occlusion consists of comparing central occlusion (CO-occlusion in which there is maximum contact between the teeth of the upper and lower jaw) and the central ratio (CO-condition in which the heads of the lower jaw occupy an anterior-superior position in the articular sockets). If there is a significant difference, a description of the differences is required. Thus, a significant difference between these conditions is more common with asymmetric deformations and with Angle class II deformities. Determining the CA is important for correctly drawing up an operational plan.
When planning the elimination of maxillary defects, we take into account the need to restore the buttresses, as well as the air supply of the upper jaw. Buttresses are the most important component for supporting the alveolar process, otherwise mobility of the upper jaw occurs after prosthetics.
Although restoration of the lost maxillary cavity and mucous lining is not possible, restoration of anatomical proximity is necessary, therefore filling the zygomaticomaxillary buttress with ilium is incorrect. It is optimal to use free split mandibular or parietal auto-bone blocks in shape in combination with bone with vascular nutrition. In the future, perhaps with the development of technologies for the use of stem cells, we will learn to restore the true mucous lining of the maxillary or paranasal sinuses.
In the reconstruction of the upper jaw, we use a fibular autograft for the reconstruction of total defects and a radial one for subtotal defects. When a radial skin-bone flap is subsequently used to place dental implants, it becomes necessary to reconstruct the second cortical-spongy layer of the alveolar process on the lingual side, which can be done using parietal or mandibular free autoblocks.
In maxillofacial microsurgery , when it is necessary to recreate bone curves, in the choice of grafts with bone, we are limited to iliac, fibular, and radial flaps, since only the latter allow 3D modeling of the bone component congruent with the defect.
of one-stage reconstruction after resection still remains open in the country . It is necessary to understand that if the reconstruction is not performed simultaneously with the resection of the jaw and even a temporary titanium structure is not applied to maintain the bite, remodeling of the temporomandibular joint occurs, both from the healthy and from the pathological side, and a violation of the trophism of the masticatory muscles. In these cases, before placing dental implants and before prosthetics of the implant, orthodontic fixation of the bite is performed in the form of braces and mini-implants, as well as muscle relaxation of the masticatory muscles on the part of the healthy jaw using Botex therapy or myotronic.
HISTORY OF THE PROBLEM
In our opinion, microsurgical autotransplantation for the purpose of jaw reconstruction has gone through several stages in its development:
Stage 1 – high-quality autograft collection, minimal modeling, and transfer to the recipient area. The main objective of this stage was to ensure graft engraftment (from 1978 to 1990).
Stage 2 included better modeling of autografts using conventional radiographs and wax templates. The main task of this stage was to restore facial aesthetics. The impaired function of the lower jaw was restored after a series of additional corrective operations and removable dental prosthetics (from 1990-1995). Stage 3 - computer modeling of the lower jaw and restoration of chewing function using prosthetics using dental implants. The main goal of this stage is to restore facial aesthetics and chewing function of the lower jaw without the use of additional corrective surgeries (from 1995 to 2011). Stage 4 - restoration of not only an ideal bite and stabilization of the TMJ, but also elimination of the imbalance of the masticatory muscles (in fact, this article opens the 4th stage in the history of maxillofacial microsurgery).
We have developed an algorithm for treating patients with jaw defects: 1. Preoperative 3D planning and production of stereolithographic and bite templates. Planning taking into account subsequent dental implantation and prosthetics. Selecting the optimal flap. 2. Restoration of buttresses, if possible, and the anatomical contours of the alveolar process of the jaws using free and pedunculated bone grafts. 3. Remodeling of the TMJ when eliminating subtotal defects of the lower jaw. 4. Dental implantation and prosthetics.
Microsurgical operation: resection of the lower jaw affected by the tumor with simultaneous reconstruction with a fibular graft on a vascular pedicle
| 1. Resection of the lower jaw affected by the tumor within healthy tissues | ||
| 2. Stage of control of resection according to the preoperative template | ||
| 3. Harvesting the fibula on a vascular pedicle | ||
| 4. Stage of modeling the harvested transplant using the author's device Karayan A.S. and Nazaryan D.N. | ||
| 5. Control of the simulated transplant on the preoperative template | ||
| 6. Fixation of the graft on the vascular pedicle to the remaining healthy fragments of the lower jaw | ||
| 7. Microsurgical stage: under a microscope, the vessels from the lower leg and the external carotid artery, jugular vein are sutured, after suturing the vessels, the clips are removed and the tissue taken from the leg is filled with blood, i.e. the flap becomes alive, but on the jaw. | ||
| 8. Control of blood supply - the final stage of microscopic surgery | Watch the video | |
| 9. The patient’s appearance before and after the operation will be practically unchanged; thanks to one-stage reconstruction, after 6 months the person will be completely rehabilitated | ||
In the scientific and clinical department of maxillofacial and plastic surgery of the Federal State Budgetary Institution NCCO FMBA of Russia under the leadership of Professor Karayan A.S. and Ph.D. Nazaryan D.N. Unique surgeries are performed to eliminate jaw defects. Such operations are performed only in 3 medical centers in Russia.
Types of osteosynthesis
There are several methods of osteosynthesis; the doctor decides what type of operation the patient needs. Most often, surgeons combine several methods with each other to achieve better results.
Osteosynthesis of the jaw can be:
- Open. It is usually used for severe fractures. During the operation, soft tissue is cut and bone fragments are exposed. They are connected to each other and non-functional small fragments are removed, compressed soft tissues and fascia are released. However, with such an operation, there is still the possibility of tissue peeling off from the bone, then the callus at the fracture site will not be formed correctly. And this can affect the patient’s quality of life. In addition, stitches remain on the skin and paresis (decreased activity) of facial muscles is even possible. Depending on the type of fastening device, it is possible that the incision on the face will have to be made again to remove the fastener.
- Closed. The doctor combines bone fragments without cutting facial tissue;
- Focal. The fixing fastener is applied directly to the fracture site;
- Extrafocal. Fasteners are placed on top of the skin, above the fracture site.
The essence of osteosynthesis and what kind of procedure it is
With osteosynthesis, the doctor not only connects the fragments of the damaged jaw, but also securely fastens them with metal structures or glue.
Open focal osteosynthesis is carried out using:
- Bone suture. If the lower jaw or cheekbone is broken and the injury is recent, it can be fastened with a bone suture. For this, stainless steel, titanium wire or nylon thread is used.
During the operation, the doctor dissects the soft tissues of the face and fixes the fragments with wire. If the fragments are connected using a bone suture, the patient retains chewing function and can continue to care for the oral cavity. This method is contraindicated if the fracture site is inflamed or the patient has an infectious or purulent bone lesion.
- Installation of periosteal metal mini-plates. This method has proven itself in the treatment of all types of jaw bone fractures, except those in which a large number of fragments have formed. In this case, it is enough to make an incision only on one side. The doctor aligns the fracture sites, applies mini-plates to them and screws them on. Nowadays, mini-plates are most often fixed inside the oral cavity.
- Fixation with quick-hardening plastics. It is practiced only for fractures of the lower jaw. After exposing the bone fragments, the doctor makes a bone groove and places a special fixing compound in it. Excess plastic is removed with a cutter, after which the wound can be sutured.
- Osteoplast glue. This composition for fixing bone fragments is made of purified epoxy resin with an organic antiseptic - resorcinol. After application, the glue hardens in 8-12 minutes and reliably fixes the combined bone fragments. Nowadays this method is rarely used.
- Metal staples. For osteosynthesis, staples made of nickel-titanium alloy are used. At low temperatures, the alloy becomes plastic and is easy to shape into the desired shape. Then, at room temperature, the staple regains its previous shape. During the operation, it is first cooled, then inserted into the prepared holes on the bone fragments. As soon as the staples warm up, they straighten and securely fix the fracture site. Metal staples are especially convenient for fixing a fracture of the angle of the lower jaw.
Closed focal osteosynthesis is practiced for healing fracture sites where bone displacement has not occurred. Methods:
- Installation of Kirschner spokes. The doctor inserts metal needles into the bone fragments using a surgical drill. For reliable fixation, the needles are fixed into each fragment to a depth of up to 3 cm. There is no need to dissect soft tissues; the operation is performed through the mouth. This is a low-traumatic practice, but wearing needles creates a lot of inconvenience for the patient.
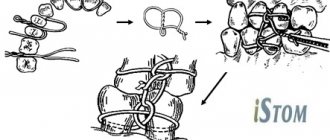
- Applying a surrounding suture. Applicable when the fracture gap is displaced forward or backward along the jaw. In this case, the suture passes through the central part of each bone fragment. If there are a lot of fragments, the operation takes a long time, but this is one of the most reliable methods of osteosynthesis. It allows the patient’s jaws to be restored even after very complex injuries.
Treatment of a jaw fracture
A jaw fracture is a partial or complete disruption of the shape and integrity of bone tissue due to mechanical trauma to the face or under the influence of general diseases. According to statistics, a fracture of the lower jaw accounts for up to 85% of the total number of facial injuries, and even double and triple fractures occur.
It should be understood that damage to the jaw of this kind is a very serious injury, in which contact with a doctor is strictly necessary. Treating a fractured jaw at home is unacceptable and is fraught with problems that will lead not only to the loss of teeth, but also to the destruction of the jaw bone.
Jaw fractures: types and forms
Depending on the cause of the jaw injury:
- traumatic fractures: occur as a result of force on the bone. This type of injury often occurs in traffic accidents, falls, physical violence,
- pathological fractures: caused by the presence of bone diseases, such as an extensive cyst, chronic osteoporosis, malignant neoplasms and others.
Depending on the degree of damage to the jaw bone:
- open fracture: bone fragments protrude beyond the gums, there is a rupture of the mucous membrane,
- closed fracture: the soft tissues of the face and mucous membrane remain intact.
The lower jaw is more susceptible to fractures, since it is the only movable bone of the facial skeleton, representing a complex anatomical structure. Immediate consultation with a doctor is required for timely and correct diagnosis of the nature of the damage.
Jaw fracture: symptoms
- excessive mobility of the lower jaw,
- acute pain with any movement of the jaw,
- mobility or displacement of teeth, the appearance of gaps between them,
- difficulty or impossibility of closing the mouth,
- profuse drooling,
- tongue retraction due to damage to the lower jaw bone,
- rupture of the mucous membrane (with an open fracture),
- bleeding from the wound,
- swelling of soft tissues, including the cheeks - facial asymmetry appears,
- difficulty breathing, problems with speech, chewing and swallowing,
- decreased sensitivity of part of the face due to damage to the nerve located at the base of the lower jaw,
- state of shock, dizziness, concussion and nausea.
Jaw fracture: causes
- exposure to heavy stress: at home, during sports, falls, impacts, road traffic or other accidents,
- diseases of the skeletal system: osteomyelitis, osteoporosis, cysts and tumors - a fracture can occur as a result of a completely insignificant load due to the initial weakening and unsatisfactory condition of the musculoskeletal system,
- complex tooth extraction.
Treatment of a jaw fracture
The sooner you see a doctor, the better, since the consequences of jaw damage pose a serious threat to the body. Among the associated complications: bleeding from the mouth and even ears, concussion, formation and spread of pus throughout the body.
If your jaw is broken, you must call an ambulance or take the victim to the hospital yourself, sitting or lying down with your head to one side. If possible, you can provide first aid: stop the bleeding, secure the jaw, apply cold to the injury site. The next solution to the problem will be the maxillofacial surgeon, whose task is to restore the correct relationship of the jaws:
- stopping bleeding by applying a tourniquet to the blood vessels,
- mandatory administration of anesthesia or anesthesia,
- conducting a diagnostic examination of the condition of the jaw system using x-rays,
- dissection of the trachea (located in the cervical area) and insertion of a tube to facilitate the patient’s breathing,
- splinting the jaw bones or installing special metal plates that will ensure the connection of all parts of the jaw. The doctor can also stitch the crushed bone with a special wire, or secure it with extraoral plates and other structures,
- fixation of the jaw in a stationary state,
- prescribing antibiotics and a special diet.
If necessary, surgery can be performed to restore damaged facial tissue. With simple fractures and timely consultation with a doctor, as well as correct adherence to all his recommendations, the functionality of the musculoskeletal system is restored within 3-4 weeks.
Osteosynthesis using ultrasound
With the help of metal fasteners, the jaw bones can be fixed quite firmly. But during surgery, it is most often necessary to cut through facial tissue and the salivary glands or branches of the facial nerve can be damaged.
It is less traumatic to perform osteosynthesis using ultrasound. In this case, the bone-fixing devices can be inserted shallowly into the bone and a small amount of scars remains on the patient’s face.
The doctor uses low-frequency ultrasound on a titanium plate with spikes. A plate with holes for the dental bur is placed at the fracture site and adapted to the shape of the jaw. An instrument is then used to make shallow holes in the bone through the plate. After which low-frequency ultrasound vibrations are directed to the base of the spines. In this way, the spikes gradually sink into the bone tissue, reliably fixing bone fragments. In this case, an antiseptic solution is supplied through the instrument, which treats the wound.
The bone tissue around the spines becomes denser under the influence of ultrasound. This occurs due to the large contact area, reducing pressure on the bone due to the use of a spike and the internal compression force of the bone tissue.
Ultrasonic osteosynthesis can reduce the time of surgery and reduce the amount of postoperative trauma. The method gives fewer complications and provides a good cosmetic effect.
Osteosynthesis
The operation is used to immobilize bone fragments with sutures, metal structures, intraosseous rods, and quick-hardening plastic. Osteosynthesis is carried out in case of ineffectiveness of conservative measures.
Indications for the operation are:
- Fractures in the area of the dentition with the formation of unstable fragments;
- Damage with the formation of a large fragment of bone without teeth;
- Significant displacement of parts of the lower jaw;
- Damage to the branches of the jaw with the formation of bone fragments;
- Fractures associated with pathological processes in the bone (malignant neoplasms, osteomyelitis).
In addition, indications for osteosynthesis surgery are incorrectly healed old jaw fractures.
Carrying out osteosynthesis
Adequate reposition of fragments and their effective fixation are the main stages of surgery for jaw fractures. Osteosynthesis is performed under conduction or intubation anesthesia.
For fractures of the condylar process, open focal osteosynthesis is performed. The doctor cuts the skin and muscles 1-2 centimeters, exposing the bone. At this stage, it is important not to damage the branch of the facial nerve, which innervates the skin and muscles in the lower jaw. After exposing the bone, the periosteum is cut off and the bone is exposed at least two centimeters on both sides of the injury. In case of damage to the chin part of the lower jaw, the incision for osteosynthesis is made in the chin area.
Once the bone is exposed, blood clots and small bone fragments are removed. Usually the method of bone immobilization is chosen before surgery, but during the intervention the surgeon can change the choice. Bone fragments are secured with bone sutures, plates with screws, knitting needles, bone rods and other special devices.
Osteosynthesis can be carried out through access to the oral mucosa. This intervention leaves no scars. However, such access does not always allow the surgeon to perform all the necessary manipulations, so it is used only when indicated.
Osteosynthesis can also be performed without exposing the bone. This operation is possible provided there are no small bone fragments. In this case, the surgeon realigns parts of the jaw with his hands, after which he secures the result with extraoral structures: splints, hooks and knitting needles. Closed osteosynthesis allows the operation to be performed with less trauma. The absence of incisions in the skin and soft tissue prevents the deterioration of the blood supply to the bone, and therefore promotes better healing.
Rehabilitation
Restoration of the jaw structure after uncomplicated fractures lasts 3-4 weeks. Rehabilitation after complicated fractures depends on the nature of the complications and the degree of damage to the jaw. After surgery, a special splint is placed on the jaw for several weeks.
In the postoperative period (as before the operation), a number of medications are prescribed that prevent the development of inflammation in the fracture area and kill bacteria that have entered the lesion as a result of the injury.
When the bone fragments have healed, the splint is removed and special rehabilitation measures are prescribed. They include therapeutic exercises to develop the masticatory muscles and restore mobility of the temporomandibular joint, as well as mechanotherapy.
Fracture of the articular head before and after osteosynthesis with two titanium screws