The lower jaw is subject to traumatic damage much more often than other bones of the facial part of the skull. Although it is one of the strongest bones, its mobility and protruding position make it susceptible to fractures. Up to 85% of all injuries to facial bones occur due to fractures of the lower jaw. These figures include both isolated fractures of the lower jaw and fractures with simultaneous damage to other bones of the facial skeleton.
Experts predict that the number of injuries to the lower jaw will only increase, as well as the nature of such injuries. This is facilitated by an increase in the number of vehicles, an increase in their speed limits, as well as complex technical equipment in production.
Types and localization of mandibular fractures
Non-gunshot, most often linear fractures of the mandible occur in the area of the condylar process, the angle of the mandible, the central incisors, the canine and the mental foramen. These places are usually called “places of weakness.”
Direct fractures of the mandible occur at the site of application of force.
Reflected fractures are localized due to the direction of impact and the area of damage. For example, as a result of a lateral impact, a reflected unilateral fracture of the neck of the lower jaw often occurs. The maximum tension in the bone tissue in the midline area is created due to bilateral compression of the mandibular bone in the region of the molars (sixth, seventh and eighth teeth).
How the fragments will be located during a fracture of the lower jaw depends on several factors. These include: the strength of the damaging factor, the volume of the injured area, as well as muscle groups attached to the surface of the injured area.
Technique of transosseous osteosynthesis
The method is suitable for helical fractures.
Screws and bolts are inserted into the body of the tubular bone in a transverse direction. Particular attention is paid to the size of the screws so that they protrude slightly beyond the bone tissue. In this case, the screw head strongly presses the injured bones, which has a positive effect on regeneration. If a sharp fracture line is clearly visible on the x-ray, it is recommended to use a round wire to tightly fasten the fragments. The surgeon carefully drills holes with a minimum diameter according to the markings, through which he pulls the wire. Removal of the wire is carried out immediately after the start of fusion (otherwise atrophic processes may start).
Causes of mandibular fractures
Mandibular injuries are divided into four types:
1. Domestic injuries that arise from conflicts in everyday life or doing housework.
2. Street injuries resulting from the use of vehicles, and street injuries not related to damage in transport. This could be a fall while walking due to ice, other bad weather, or poor health.
3. Sports injuries received while playing sports.
4. Industrial injuries sustained in industrial production in agriculture.
Symptoms of a mandibular fracture
With a fracture of the lower jaw, patients may complain of impaired or limited mobility of the lower jaw, pain that may intensify with movement, biting or chewing, malocclusion, changes in the sensitivity of the skin on the lower lip or chin, bleeding from the oral cavity - a symptom characteristic of ruptures of the mucous membrane .
The range of complaints that the patient presents helps the doctor understand what kind of damage is being discussed and suggest the location of the fracture.
Diagnosis of mandibular fractures
Diagnosis is based on examination data and collection of patient complaints.
During the examination, the doctor pays attention to the condition of the skin, notes whether the patient has bruises, abrasions or wounds, and records the presence of hyperemia, cyanosis and bruising. Notes the presence of asymmetry on the damaged side of the face.
If a fracture of the lower jaw is suspected, the doctor first feels the undamaged area with his fingertips, and then the damaged one. He marks the places of greatest pain, unevenness, violation of integrity, determines the amplitude of movement of the head of the lower jaw in the articular cavity - for this, the doctor places the tip of his finger in the external auditory canal. The doctor determines the condition of the head of the lower jaw or its displacement by palpating the surface in front of the tragus of the ear both in motion and at rest.
Violation of the integrity of the lower jaw confirms a number of symptoms associated with pain in the fracture area:
Symptom of referred pain
(indirect load), in which pain in the fracture area occurs in response to finger pressure on the chin.
Spatula symptom
provokes pain at the site of the jaw fracture, both lower and upper. To do this, a wooden spatula is placed between the patient's teeth, after which the teeth are closed, and the doctor makes a small blow to the outer part of the spatula.
The occurrence of pain with simultaneous pressure and bringing together the angles of the lower jaw may indicate a fracture of the chin.
Impaired pain and tactile sensitivity of the skin of the lower lip and chin may indicate damage to the lower alveolar nerve.
Fractures of the lower jaw are characterized by a change in bite (the teeth of the upper and lower jaws do not close together correctly), which depends on the nature and location of the fracture.
Thus, with a unilateral fracture in the area of the body or angle of the lower jaw, the closure of the teeth will occur on a small fragment.
A unilateral fracture with displacement of the condylar processes is characterized by closure of the molars only on the damaged side, and no contact occurs on the undamaged side.
With a bilateral fracture of the angles or body of the lower jaw, contact is possible between the molars, while the front teeth cannot close - the patient has an open bite.
For a fracture in the central part of the lower jaw, malocclusion may not occur. But if there is displacement of the fragments, the patient will have a tilt of the chewing teeth towards the tongue (tubercular contact).
A change in bite may also be indicated by a shift in the midline between the central incisors on the upper and lower jaws, and a mismatch in the position of the frenulum of the upper and lower lips.
Examination of the oral cavity helps to find breaks in the mucous membrane of the alveolar process, as well as to detect hemorrhages in the area of the transitional fold (often with exposure of bone). Palpation allows you to determine the location of sharp edges under the mucous membrane and confirms abnormal mobility of the lower jaw. If there are displaced fragments, the doctor visually fixes the neck or root of the tooth in the fracture line.
After examination, the nature and location of the fracture is confirmed using X-rays (pictures are taken in frontal and lateral projections) or using multispiral computed tomography. Orthopantomography does not always allow one image to see all the changes that occur due to trauma to the lower jaw. It should be noted that for fractures in the area of the angle, if the fragments are displaced outward, the orthopantomogram may not show the displacement. It should be considered as two lateral radiographs, to which it is necessary to additionally take a radiograph in a frontal projection.
Pictures obtained by orthopantomography can be used as lateral projections, but always require an additional AP picture obtained using radiography.
The x-ray image better shows the violation of the integrity of the bone tissue, the presence of a tooth root in the fracture gap.
After an imaging test, the doctor makes a final diagnosis and determines a treatment plan for the patient.
Closed focal osteosynthesis
Closed focal osteosynthesis is used when the fragments can be easily reduced by hand or for jaw fractures without displacement of the fragments.
Kirchner spokes
Kirschner wires are also used as closed focal osteosynthesis. They are inserted into the fragments using a drill or a special low-speed drill Aoch-3 (M.A. Makienko) so that its length in each fragment is at least 3 cm.
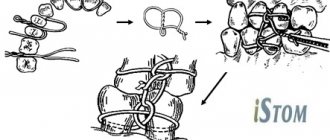
Surround seam (Black method option)
Used when the fracture gap is significantly tilted in the anteroposterior direction. The ligature of the surrounding suture is carried out in such a way that it passes through the middle of the fracture gap and compresses the fragments in the vertical direction, preventing them from moving in the longitudinal direction. The method can be used alone or in combination with the use of a supragingival splint or prosthesis.
Closed extrafocal osteosynthesis
Using a Surround Seam (Black)
Stages of osteosynthesis of mandibular fragments using a surrounding suture
Indications : absence of teeth or insufficient number of stable teeth on fragments, traumatic osteomyelitis, suppuration of a bone wound, pathological fracture. To apply a surrounding suture, use a wire or nylon ligature d = 0.6-0.8 mm, which is carried out using a curved thick hollow needle without a cannula. In case of a unilateral fracture of the lower jaw, one surrounding suture is placed on each side of the fracture gap, departing from it by 1.5-2.0 cm, and one on the opposite side. Typically, a surrounding suture is used for single-jaw fastening of fragments in the case of single, double or bilateral fractures of the lower jaw within the dentition. In this case, a supragingival splint or a removable denture of the patient is used. A dental splint is placed on the alveolar part of the lower jaw, which is fixed to the fragments with surrounding sutures. In the first week the patient should take liquid food, and after 8-12 days he can eat soft food.
S-shaped hooks (M.B. Shvyrkov, V.S. Starodubtsev, V.V. Afanasyev, etc.)
Indications for the use of S-shaped hooks : lack of the required number of teeth in the lower jaw for the application of dental splints, stage II-III periodontitis, low tooth crowns, deep bite, hypertrophic gingivitis. The hook is bent to the shape of a fishing hook using stainless steel wire 1X18H9T with a cross-section of 1.2-1.5 mm. It is distinguished: body, small and large bends. The end of the large bend is sharpened like an injection needle for free and low-traumatic passage through the tissues. First, a splint with hooking loops is applied to the teeth of the upper jaw. The hook is grasped with crampon forceps, the pointed end of the large bend of the hook is inserted into the lower arch of the vestibule of the mouth, directing it downwards, sliding along the outer surface of the jaw. It is advanced below the base of the lower jaw, rotated around the longitudinal axis by 90°, bringing a large bend under the base of the body of the lower jaw. At the same time, give it a vertical position and insert its sting onto the inner surface of the body of the lower jaw, pull the hook up, checking its stable position.
Schematic representation of the stages of osteosynthesis of the lower jaw using S-shaped hooks
S-shaped hooks are placed 1.5 cm away from the fracture gap. After applying the hooks, intermaxillary traction is performed and the fragments are fastened using rubber rings. After treatment is completed, the hook is removed using reverse movements.
Unified hooks (M.B. Shvyrkov, V.S. Starodubtsev, V.V. Afanasyev)
Indications: lack of a sufficient number of teeth on both jaws for splinting, stage II-III periodontitis, low tooth crowns, deep bite, hypertrophic gingivitis, wide interdental spaces, conical teeth, complete absence of teeth in the presence of removable dentures. To make hooks, use wire with a diameter of 1.2 mm made of stainless steel grade 1Х18Н9Т. They bend in the shape of the letter "L". The size of the long arm of the hook (shank) is 12-14 mm, the short one - 5-6 mm. At the end of the short arm, a hook is bent. To apply special hooks, a ball-shaped bur is used to drill channels in the alveolar process of the upper and lower jaw above the apexes of the roots of the teeth in the interdental spaces. The unified hook is inserted with the shank into the trepanation canal up to the mucous membrane. Rubber rings are put on the hooks and intermaxillary traction is performed and the fragments are fastened. After consolidation of the fragments, the hooks are removed.
X-ray of the lower jaw, direct projection. Osteosynthesis using standardized hooks
Federspiel-Dingman-Erich method
Indications : chronic fractures of the upper jaw of any type with fragments that are difficult to compare. Contraindications : simultaneous fracture of the cranial vault, the need for craniotomy, flat occiput of the victim. First, a smooth splint-bracket is applied to the teeth of the upper jaw. A steel wire d = 6-7 mm is bent in an arc and tried on the patient’s head so that the arc is in the plane of the visor and is 6-8 cm from the forehead, the ends of the wire should almost touch the temples above the ears. The ends of the wire (arc) are bent 180° to form loops. Next, a plaster cap is made, into which the previously made wire arch is “plastered.” The soft tissues of the cheeks are pierced with a hollow needle at the level of molars and premolars on both sides and nylon or metal ligatures are passed through the needles, which are fixed at one end to a smooth splint-clip and the other to a wire arch, immobilizing fragments of the upper jaw.
Adams method
Indications: fresh fractures of the upper jaw with easily reducible fragments. Before the operation, a smooth splint-bracket or a splint with hooking loops facing downward and located in the area of the molars is applied to the teeth of the upper jaw. In the case of fractures of the upper jaw of the Le Fort II or Le Fort III types, the ligature is passed around the zygomatic arch on both sides into the vestibule of the mouth at the level of the first upper molars and fixed to the dental splint.
Immobilization of maxillary fragments using the Adams method
In case of a fracture of the upper jaw of the upper type, the ligature is passed through a hole in the outer edge of the orbit 1 cm above the fracture gap. One end of the ligature is passed into the vestibule of the mouth from the inside of the zygomatic bone at the level of the first molar. The other is on the inside of the zygomatic bone, but at the level of the first upper premolar. The ligatures are fixed to the dental splint. If the fragments are significantly displaced and their simultaneous manual reduction is impossible, M.B. Shvyrkov used the lower jaw to compare the fragments. To do this, ligatures were fixed using rubber rings to a splint with hooking loops, previously applied to the lower jaw.
Vision-Billet method
Indications : fractures of the upper jaw accompanied by a fracture of the frontal bone. The method is used when there are indications for craniotomy. First, a smooth Tigerstedt splint is applied to the teeth of the upper jaw. The surgical intervention is performed jointly with a neurosurgeon. After an arcuate incision in the parietotemporal region, a tongue-shaped flap is separated from the bone and the fracture gap is isolated on one side. Behind it, two milling holes are placed at a distance of 1-2 cm from each other. A ligature is passed through them. Both ends of it are passed into the vestibule of the mouth using a hollow needle. The flap is placed in place and the wound is sutured. A similar operation is carried out on the other side. Next, the fragments are set and the ends of the ligatures are fixed to the maxillary splint. M.B. Shvyrkov proposed making one burr hole on the skull, on which an S-shaped hook is fixed. One end of the hook is inserted between the dura mater and the parietal bone, the second is pressed firmly against the outer surface of the bone. A ligature is fixed at this end, which is passed into the vestibule of the mouth in the manner described above and fixed to the splint. PC. Pubis, in case of combined fractures of the upper jaw and frontal bone, proposed strengthening the fragment by tying ligatures on the crown. To do this, an arcuate incision is made to the bone in the parieto-occipital region, and a flap of soft tissue is peeled off. Ligatures are inserted subcutaneously from both sides into the vestibule of the mouth and fixed to the dental splint. After repositioning the fragments, the ends of the ligatures are twisted in the wound on the crown, and the wound is sutured. This method is not suitable for use in patients with an egg-shaped skull.
Kirchner spokes
In case of a fracture of the lower jaw in the chin region, the wire is inserted into the bone at the level of the canine, the bone is perforated and brought out into the sublingual region, then advanced until it comes into contact with the bone of the opposite side and the jaw is perforated. If you insert two parallel wires, you can achieve strong fixation in the presence of a bone defect.
Using Kirschner wires according to V.V. Donskoy with a fracture of the lower jaw in the area of the angle. A Kirschner wire is inserted into the anterior edge of the mandibular ramus in the retromolar region in parallel and at the level of the necks of the molars to a depth of 1.5-2.0 cm. The free end of the wire is bent along the lower dentition under the conditions of repositioning the fragments and tied to the teeth with a ligature wire. Fresh fractures of the upper jaw with easily reducible fragments. For a Le Fort II fracture of the upper jaw, the wire is passed from one zygomatic bone to the other. You can pass the second needle parallel to the first or in an oblique direction to enhance fixation. Old fractures of the upper jaw with fragments that are difficult to reduce. A plaster cap with an arched visor is used. The pin is passed under the zygomatic bone below the fracture gap (Le Fort II) or through the zygomatic bones (Le Fort I) so that the ends of the pin protrude above the surface of the skin on both sides. Rubber rings are put on these ends and connected to the arch using wire hooks, performing reposition in the required direction and subsequent immobilization.
Extraoral devices for immobilization of fragments
Extraoral devices for immobilization of jaw fragments are divided into “static” and “dynamic”. In addition, according to the method of fixation on the jaw, they are divided into “clamp” and “spoke”. Static devices provide only passive fixation of fragments. Using dynamic devices, it is possible to perform fixation, compression and distraction of fragments with movement in a given direction. Some devices have clamps (terminals) that are fixed on the body of the lower jaw, covering its base. Other devices include wires that are inserted into the body of the jaw. They are used to fasten fragments.
Static devices
Apparatus V.F. Rudko .
Apparatus V.F. Rudko
Used in the treatment of linear and comminuted fractures of the lower jaw with an insufficient number of teeth on the fragments. Bone clamps are applied to each of the fragments, 2 cm away from the fracture gap. Then the fragments are reduced and the bone clamps are connected with an extraoral rod. Yu.I. Bernadsky proposed using two parallel rods to increase the rigidity of the fixation. Devices Ya.M. Zbarzha, V.P. Panchokhs are designed on the same principle and differ from the Rudko apparatus in small design features of individual parts. Each device has bone clamps for fragments, which are secured to the body of the lower jaw using a screw device. Devices EK (I.I. Ermolaev - S.I. Kulagov) and A.A. Datsko is fixed on the fragments using knitting needles inserted into the bone using a drill. The introduction of wires through the skin does not require skeletonization of fragments.
First aid for fractures of the lower jaw
It can be carried out either at the scene of the incident or in an ambulance. It can be provided by both medical and non-medical workers in the form of mutual assistance.
The victim’s damaged jaw is temporarily (for several hours) fixed (the upper jaw is pressed to the lower) using bandages or other devices in order to be able to deliver him to a medical facility.
For fixation, the following can be used: a circular bandage parietal-mental bandage, a soft chin sling (Pomerantseva - Urbanskaya), an Entin splint (standard transport rigid bandage), as well as various types of intermaxillary ligature binding. If the patient has a traumatic brain injury, ligature binding is used with extreme caution - fixed jaws do not allow opening the mouth, and can lead to aspiration of vomit or blood.
External transosseous osteosynthesis technique
An operation using a guide apparatus prevents the penetration of bone fragments into the tissue and does not impair the functioning of the joint. This allows you to speed up the restoration of cartilage and bones in the affected area. This operation is recommended for open fractures of the humerus and tibia, as well as for closed fractures of the tibia.
Note! The operation must be performed by an experienced expert, since different types of needles are used and it is necessary to correctly calculate the trajectory of movements and determine the design features of the device. Moreover, all calculations are made during surgery, so you need to act within a narrow time frame. A successful operation allows the patient to rehabilitate in just 20-25 days.
Permanent fixation of fragments
Fragments of the lower jaw can be fixed using conservative and surgical methods.
Permanent fixation can be carried out using: steel standard tape splints (Vasiliev splints), Tigerstedt dental wire splints, dental dentogingival and supragingival plastic splints, which are made in dental laboratories (they are rarely used nowadays).
In recent years, some clinics have begun to use orthodontic screws, which are inserted through the mucosa into the alveolar processes of the jaws, 3 pieces on each side, after which a rubber rod is put on the heads of the screws, providing intermaxillary fixation. This avoids the time-consuming procedure of double-jaw splinting. On the other hand, when inserting screws, the roots of the teeth can be damaged; in addition, there are often situations when the screw, under the action of a rubber rod, becomes mobile, which leads to inadequate intermaxillary fixation and removal of the screw.
If conservative treatment methods do not produce an effect, osteosynthesis is used - this is a surgical method that, with the help of devices, allows you to fix the fragments and eliminate their mobility. Osteosynthesis is performed if the patient has comminuted fractures of the lower jaw, or the displacement of the fragments is so pronounced that they do not allow closed reduction. Osteosynthesis is also indicated in the absence or insufficient number of teeth in the patient.
Approximately 30% of patients with mandibular fractures require surgical treatment. Currently, osteosynthesis is one of the leading methods of surgical care, and is used much more often than in the past.
This is due both to an increase in the arsenal of technical means for performing surgery (the presence of physiodispensers, titanium miniplates), which leads to improved surgical techniques, greater predictability of results, and to the requests of patients, which are aimed at a more comfortable course of the post-traumatic period, reducing the time of intermaxillary fixation, and in some cases, complete abandonment of it.
Methods for treating fractures using surgical techniques make it possible to compare and fix mobile bone fragments in a normal anatomical position. This helps reduce treatment time and achieve early restoration of lower jaw function. However, according to various data from Russian and foreign clinics, there is also a negative aspect of using osteosynthesis - about 30% of patients experience complications after using this technique. This is due to the use of materials to hold fragments: steel, titanium, etc. Even the most bioinert alloys are not ideal. Being in bone tissue, they undergo corrosion and cause galvanosis, which negatively affects the recovery process and can cause purulent-inflammatory complications and pain reactions.
Complications after osteosynthesis
After performing open osteosynthesis, the following pathologies may appear:
- Embolism.
- Osteomyelitis.
- Infectious infection.
- Arthritis.
- Internal bleeding.
To avoid complications, the specialist prescribes antibiotics and medications that prevent the formation of blood clots. If there is pain, swelling, bleeding or elevated body temperature, you should immediately consult your doctor.
Osteosynthesis methods
There are direct and indirect methods of osteosynthesis.
Direct methods:
— intraosseous osteosynthesis using knitting needles, rods, pins and screws,
— bone osteosynthesis using bone plates, staples, circular ligatures, frames,
— intraosseous osteosynthesis based on bone sutures or their combination with knitting needles and staples.
Indirect osteosynthesis is based on the use of various fixation devices, both extraosseous (bone clamps and clamps) and intraosseous (rods, pins, screws and knitting needles).
Osteosynthesis can be performed both under local anesthesia in combination with neuroleptanalgesia and ataralanalgesia, and under general anesthesia.
The nature of the access (extraoral or intraoral) is determined by the doctor.
If osteosynthesis is performed using an extraoral approach, then in case of a fracture in the area of the angle and body of the lower jaw, the doctor makes an incision in the submandibular region. If the fracture occurred in the frontal area, the incision will be in the submental area. For fractures in the area of the condylar process - in the retromandibular region. During the operation, the doctor exposes bone fragments, removes small fragments, and fixes large fragments and fragments in a normal anatomical position using the selected design.
If the doctor uses intraoral access to perform osteosynthesis, he makes an incision in the mucosa along with the periosteum, then compares the fragments and performs osteosynthesis.
Types of osteosynthesis
There are several methods of osteosynthesis; the doctor decides what type of operation the patient needs. Most often, surgeons combine several methods with each other to achieve better results.
Osteosynthesis of the jaw can be:
- Open. It is usually used for severe fractures. During the operation, soft tissue is cut and bone fragments are exposed. They are connected to each other and non-functional small fragments are removed, compressed soft tissues and fascia are released. However, with such an operation, there is still the possibility of tissue peeling off from the bone, then the callus at the fracture site will not be formed correctly. And this can affect the patient’s quality of life. In addition, stitches remain on the skin and paresis (decreased activity) of facial muscles is even possible. Depending on the type of fastening device, it is possible that the incision on the face will have to be made again to remove the fastener.
- Closed. The doctor combines bone fragments without cutting facial tissue;
- Focal. The fixing fastener is applied directly to the fracture site;
- Extrafocal. Fasteners are placed on top of the skin, above the fracture site.
Bone or wire suture
In 1825, surgeon Rogers from Dublin performed the world's first operation using silver wire. With its help, he connected the fragments of the lower jaw. Later, in 1863, Russian surgeon Yu.K. Szymanowski successfully used a bone suture. From this point on, the bone suture was successfully used for osteosynthesis for many years. The main material was initially stainless steel, later it was replaced by titanium, nichrome, tantalum, etc.
There are various modifications of the bone suture (loop-shaped, cruciform, figure-of-eight, trapezoidal, double, etc.). The choice depends on the nature and location of the fracture.
The application of a bone suture occurs according to certain rules. It is important to make holes for the material in those areas where damage to the mandibular canal and tooth roots is excluded, and no closer than 1.0 cm from the fracture line. Ideally, the suture should cross the fracture line in the middle of the distance between the edge of the mandible and the base of the alveolar process.
Metal Kirschner spokes
This type of wire was first used to treat fractures of the lower jaw in 1933. Intraosseous insertion of these wires can be carried out both percutaneously (without incisions) and with soft tissue incisions.
In 1975 V.V. Donskoy used an original technique, with which he inserted a wire into the branch of the lower jaw through the mucosa without an incision, then carried out a reposition, and fixed it like a splint to the teeth or to a splint. Later, in 1988, Deryabin E.I. and Osipov V.Yu., and Yu.G. Kononenko and G.P. Ruzin proposed modifications of this method in 1991. Today there are many techniques where the wire suture is combined with knitting needles, staples, surrounding wire ligatures, etc.
Indications for the use of osteosynthesis
Osteosynthesis is used in cases where conservative methods of fixing fragments do not give the desired result . — Fractures of the jaws within the dentition with: — insufficient number of stable teeth on the fragments; - significant displacement of fragments and the impossibility of their reposition without surgical intervention. — Fractures of the jaws behind the dentition with displacement of fragments. — Pathological fracture of the jaw resulting from an inflammatory or neoplastic disease of the bone tissue. — Large and small-comminuted fractures of the body and branches of the lower jaw. — Defects of the body and ramus of the jaw with preservation of the condylar process. — The need for osteoplasty and reconstructive surgery.
International standards
A real revolution in maxillofacial surgery occurred in 1958, when M. Muller, M. Allgower, R. Schneider, H. Willenegger organized the International Association for the Study of Internal Fixation (AO/ASIF - Ardeitsgemeinschaft fur Osteosynthesefragen/Association for the Study of Internal Fixation – working association for the study of osteosynthesis/association for the study of internal fixation).
According to the postulates of AO/ASIF, the osteosynthesis technique implies that:
1. the structures used must be made of bioinert metal alloys;
2. bone fragments must be anatomically accurately compared and fixed;
3. the use of gentle surgical techniques ensures the preservation of blood supply to bone fragments and surrounding soft tissues;
4. stable fixation of fragments is ensured by interfragmentary compression;
5. early application of functional load is indicated;
6. restoration of contractile activity of muscles and movement in the joint.
AO/ASIF staff also developed and implemented metal plate systems for mandibular osteosynthesis:
· dynamic compression plates;
· reconstructive (blocking) plates (Locking reconstruction plates);
· blocking (locking) plates (Locking plates 2.0 mm);
· universal plates (Universal fracture plates);
· mandibular plates (Mandible (Mandible plates 2.0 mm).
They developed dynamic compression plates (DCP), through which it was possible to create compression between fragments for their primary fusion. The design of these plates includes oval holes with beveled walls, which allows the fragments to be brought closer together when the screws are tightened. The use of dynamic compression plates made it possible to achieve stable internal immobilization, reduced the number of cases of delayed fusion of fragments, and eliminated the need for additional fixation. But their use still does not eliminate the risk of microcracks in the area of the fracture line and the development of osteoporosis in the bone at the site of contact with the plate.
The locking plate/screw system, with threaded plate holes and locking screw heads, was developed to prevent bone necrosis under the plate. The system provides rigid fixation of bone fragments using a plate and a plate and screws to each other - this helps prevent the screws from unscrewing and avoid possible displacement of the fragments while tightening the screws in the hole of the plate. The plate itself is located at a certain distance from the surface of the bone, which prevents the development of lysis.
Foreign studies have not revealed significant differences in the effectiveness and possible development of postoperative complications during osteosynthesis with locking plates with screws and non-locking plates.
Another system developed by AO/ASIF experts is the LCP (locking compression plate system with angular stability) is a design of multi-cell plates with numerous holes and consists of two parts: a threaded one for fixing the head of a locking screw and a hole for creating dynamic compression by eccentric insertion of standard cortical or cancellous screws.
Installation of the plate requires special tools and is carried out according to clearly established technology.
If the adjustment of the LCP to the shape and relief of the outer surface of the lower jaw bone is carried out in accordance with the established requirements, then this creates ideal conditions for the fusion of fragments during osteosynthesis of multiple comminuted fractures of the lower jaw of various locations, in case of suppuration of a bone wound, traumatic osteomyelitis, in case of a fracture with the occurrence of a bone defect tissue, fracture of toothless jaws. Limited contact of LCP with bone helps prevent the development of bone necrosis under the plate.
Varieties
There are different ways to fix bone fragments:
- Internal osteosynthesis involves the presence of an incision. The surgeon gains access to the broken bone and performs fixation. To do this use: Screws. Used for fractures of short bones and long heads.
- Plates. They are screwed to the bone. They securely hold the fragments together, but they are not used in children, as they can damage the periosteum and disrupt bone growth.
- Pins and spokes. They are driven into the bone in a longitudinal direction.
- Wire, special threads. They are usually used to hold small fragments in place.
Recommendations
Treatment of mandibular fractures involves long-term immobilization of the jaws, which becomes a significant psychological problem for the patient. The success of treatment directly depends on how closely both the doctor and the patient act together and take the process seriously.
For the entire period of healing of the fracture, the patient is prescribed a diet (maxillary table No. 1 and No. 2); food is allowed to be taken only in a creamy consistency (well boiled and passed through a blender). In most cases, opening the mouth is impossible, because... The patient has an intermaxillary rubber traction device installed. Food is supplied through tubes, tubes and sippy cups.
From the moment of double-jaw splinting or osteosynthesis, the splints are left in place for an average of 21–30 days. If the doctor has confidence in the favorable course of the recovery process, then it is possible to reduce the period of wearing the intermaxillary rubber traction.
Even after removing the splints, the patient cannot fully open his mouth for 1-2 weeks. To restore the function of the chewing and facial muscles, he is prescribed myogymnastics.