Inflammatory gum disease in adults and children is called gingivitis. It is most often observed in children a few months from birth to 13 years of age, which is explained by the characteristics of the child’s body and poor oral hygiene.
According to statistics, in a child from 2 to 4 years old, gum inflammation occurs in 2% of cases, and by the age of 13, the proportion of this disease in children reaches 80%. Gingivitis cured in time does not become chronic, but if left untreated it can cause the development of periodontitis.
Causes of gingivitis in children
There are many causes for childhood gingivitis. The gums become inflamed due to the functional immaturity of their tissues. In babies under one year of age, the cause of the disease is often teething, when the gums become red and sore. Sometimes inflammation is caused by an allergic reaction to food.
In adolescents, the disease may manifest itself due to the eruption of a permanent tooth. When soreness during brushing does not allow this procedure to be performed efficiently, microbes multiply and gum inflammation develops.
The most common factors that provoke the development of gingivitis in older children are:
Action of microbes
In 90% of cases, the disease appears in a child due to insufficient oral hygiene, as a result of which microorganisms multiply intensively, plaque and tartar form, and stomatitis develops.
Mechanical injury
The integrity of the mucous cavity can be compromised by teething, cuts, scratches, burns, biting, improper brushing of teeth, and eating solid foods.
Foci of infection in the oral cavity
If children have carious teeth, there is a chance that they will develop infectious gingivitis, which affects the gums. Therefore, teeth that require treatment must be treated as soon as possible.
Excessive loads on the dental system
Other causes of gum damage in children may include:
- presence of malocclusion;
- poor nutrition with a lack of vegetables and fruits;
- uneven load on the dental system due to bad habits;
- defects of the oral cavity (short frenulum of the tongue, lips);
- the presence of caries, various infections;
- thermal burn from hot food;
- wearing braces.
Symptoms
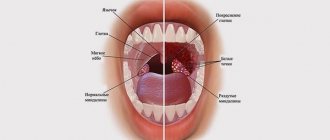
Gingivitis has a main symptom by which it is easily identified - inflammation affecting the child’s gums. The process begins with a slight redness that quickly gains strength. This signal often goes unnoticed by parents, and children go to the dentist with an active inflammatory process, bright red swollen gums, burning, and pain. These signs indicate that the disease has entered an acute phase.
Children suffer most from the catarrhal form of this disease, which can be chronic or acute. In the first case, the symptoms are not pronounced, pain occurs only when brushing, there is slight swelling, redness, and cyanosis of the gums.
A sign of an acute form of the disease is intoxication of the child’s body. It manifests itself as headache, nausea, lethargy, and fever.
The most complex type of disease, ulcerative gingivitis, manifests itself as follows:
- the inflammatory process progresses;
- their structure changes;
- there is an unpleasant odor from the mouth;
- lymph nodes in the neck enlarge;
- saliva is produced profusely;
- the skin turns pale.
If these signs are left unattended, an ulcerative-necrotic form of the disease may occur, when necrotic areas with a gray-green coating and a putrid odor appear on the gums, saliva becomes viscous, body temperature rises and the general condition significantly worsens.. All this indicates severe intoxication in organism.
During puberty in a teenager or if he has problems with hormones, hypertrophic gingivitis occurs. It occurs due to improper orthodontic treatment of dental anomalies. The inflammatory process is accompanied by increased growth of gingival tissue, which leads to partial closure of dental crowns. This form of the disease is usually localized. One or two gums are affected, sometimes the affected area expands. The most common location is the lower anterior incisors and canines.
Atrophic gingivitis does not have a pronounced inflammatory process and occurs without pain, although over time it can be complicated by periodontal disease.
Symptoms of the disease
Herpes sore throat in a child does not manifest itself for seven to fourteen days. This is the incubation period for the disease. Then symptoms appear that are similar to those of other infectious diseases: acute respiratory infections, acute respiratory viral infections, influenza, intestinal infections - therefore, at the initial stage, herpetic sore throat is difficult to diagnose:
- high temperature up to 40°C
- severe sore throat, sore throat, cough
- Gastrointestinal disorders (vomiting, diarrhea, abdominal pain)
- muscle pain
- enlarged lymph nodes in the neck
- In infants, convulsions are possible.
Abdominal pain and digestive disorders are associated with the activity of enteroviruses in the intestines that cause herpes sore throat - they affect the intestinal and stomach mucosa, thereby disrupting their functioning. On the second or third day of illness, a characteristic rash appears on the palate and tonsils, similar to blisters with liquid. The appearance of these rashes is a sign that we are dealing with herpetic sore throat. When these bubbles burst, they form ulcers, which create discomfort and pain in the mouth. A child experiencing severe sore throat may refuse not only food, but also drink. Increased salivation is possible, since the receptors that affect saliva production are constantly irritated.
If the baby has a weak immune system, the formation of bubbles can occur in several “passes” and with a break of two to three days, accompanied by a repeated increase in temperature and symptoms of intoxication. There are cases when rashes appear on the legs, arms and body, but not on the face.
The fever usually subsides on the third to fifth day, and mouth ulcers disappear within a week. When the peak of the disease passes, the child feels significant relief - improvement occurs on the sixth or seventh day after the appearance of the first symptoms. But we must remember that for a certain period the child remains a source of infection! One of the differences between herpes sore throat and acute respiratory infections is the absence of nasal discharge, although swelling of the mucous membrane is present. Also, outbreaks of acute respiratory infections and acute respiratory viral infections in the summer, as a rule, do not happen, which cannot be said about this type of sore throat. In summer, heat contributes to the rapid spread and high activity of enteroviruses, and the number of cases of herpangina increases accordingly.
Normally, herpetic sore throat in children lasts from eight to ten days.
Dear parents! Diagnosis and treatment of herpetic sore throat in children must be carried out under the supervision of an otorhinolaryngologist, since it is not always possible to make a correct diagnosis on your own (due to the similarity of the initial symptoms of the disease with other viral diseases). Failure to start proper treatment on time can result in a protracted illness and complications!
Diagnostic methods
The diagnosis is made by a doctor based on the results of studying the medical history and life of the child in combination with a dental examination. The patient’s complaints, the presence of somatic diseases, and whether he is taking medications that may cause the development of gingivitis are clarified.
Then the doctor conducts an external examination, paying attention to maxillofacial anomalies, the condition of the teeth and gums, and makes a diagnosis. The dentist does not require the help of other specialists, since the disease clearly manifests itself externally and does not require instrumental examination.
Treatment
Treatment for childhood gingivitis is practically no different from how adults are treated. Only medications used for them are softer and more gentle. Treatment begins with professional cleaning of hard deposits and plaque of tooth enamel - mechanical or ultrasonic.
If caries is detected during the examination, then therapeutic treatment is carried out. Gingivitis is then treated with medications with antiseptic and anti-inflammatory properties. Measures are taken to eliminate detected pathologies (bite, frenulum, etc. are corrected).
Ointments and gels are considered effective for children under 4 years of age. For example, Cholisal ointment has analgesic and anti-inflammatory properties, which makes it possible to prescribe it to alleviate the patient’s condition, especially when baby or permanent teeth are cutting. Ointments and gels are applied directly to the inflamed area.
Antibiotics in tablets or in the form of injections are prescribed to children in difficult cases (the presence of infections of bacterial origin in the body). At elevated temperatures, rinses, drinking plenty of fluids, antioxidants, antipyretic drugs for children, and taking vitamins are prescribed.
Prevention measures should include regular visits to the pediatric dentist, training in oral care rules, and parental monitoring of the development of hygiene skills.
Rashes in babies
Babies are generous with various rashes. According to the “good” tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of medicinal mixtures, etc. In fact, true allergic rashes in infants are not that common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and Quincke's edema. Acute urticaria is extremely rare in infants - it is an acute allergic reaction in the form of peculiar blistering-type rashes (like a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace behind, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the child’s general anxiety. The most common causes are food proteins (for example, cow's milk), viral infections, insect bites and medications (for example, antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's figure out what is most often unfairly called an allergy:
Erythema toxicum of newborns is a transient, benign rash whose exact cause is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24–48 hours of life. Localization - face, torso, limbs, except palms and soles. Disappears on its own within 5–7 days, sometimes 3 weeks. Does not require treatment.
Newborn acne (infantile acne, neonatal pustulosis) is caused by stimulation of the baby's sebaceous glands by androgens.
The peak of rash occurs in the 3rd week of life. It is most often localized on the face, sometimes spreading to the scalp, less often to the collar area. Resolve spontaneously. The skin requires cleansing and moisturizing; in some cases, the use of medicated creams may be required.
Miliaria is a rash that occurs in poorly “ventilated” areas as a result of blocked sweat glands. Can occur at any age.
Localization - folds of skin, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, there are crystalline prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash ranges from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Calamine-containing lotions and corticosteroid and antibiotic creams may be used to treat some cases of prickly heat and miliaria.
Seborrheic dermatitis is a skin disorder that forms on sebum-rich areas of the skin. The exact cause is unknown (a certain role is played by the skin saprophyte - the Malassezia fungus, which grows well and multiplies in sebaceous secretions).
It can be focal or widespread, dermatitis with pityriasis-like scales, which can form a crust (“cap”, gneiss) on the scalp.
Favorite localization is the scalp, face, folds (!).
It can begin from the 1st - 2nd week of life or later, and resolves spontaneously over several weeks or months.
Treatment involves softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a nonspecific damage to the skin due to prolonged or repeated exposure to a number of substances - saliva, fruit juices, foaming bath products, detergents (their residue on the walls of the bathtub), etc. In infants, saliva often causes dermatitis in the contact area with the pacifier and in the folds of the neck.
As a rule, elimination of the offending agent and short-term administration of anti-inflammatory creams quickly leads to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (a prototype of contact dermatitis) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - area of the diaper or diaper area.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education). Frequently changing diapers, washing the skin and drying it thoroughly helps. Dermatitis is effectively prevented by applying products to clean skin that completely cover it (vaseline, zinc paste). In persistent cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases it is combined with food allergies (the most common “culprits” are cow’s milk, chicken eggs, wheat, fish, soy, nuts).
Most often it starts no earlier than 3 months of life.
The most common localization up to 2–3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and the torso; it never occurs in folds in infants (!).
Exacerbations are triggered by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabric, detergent residues on clothes, etc.
It is treated with careful skin care and the use of anti-inflammatory creams.
There are also:
Pseudoallergic reactions are reactions that are externally similar to allergic ones (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is the increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to enhance the release of these substances in the body, or their increased absorption, due to pathology of the gastrointestinal tract (enzymopathies, inflammation in the intestinal wall, etc.). These products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
The clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains the creation of a “skin barrier” by constantly moisturizing the skin with emollients, stopping exacerbations with anti-inflammatory creams and excluding exacerbation factors.
And the last thing:
Skin infections - herpes virus, staphylococcal pemphigus, candidiasis also occur in infants, do not forget about them. You should consult a doctor immediately if the child is lethargic, has a fever, refuses the breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of blisters, erosion (violation of skin integrity), severe swelling and redness of the skin.
Author:
Eroshkina Maria Sergeevna pediatrician